-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*For medical professionals to read only for reference to the side effects of chemotherapy, is it really that scary?
With the development of tumor treatment technology, new anti-tumor treatment methods such as targeted therapy and immunotherapy have been born, but chemotherapy still plays an important role
in the field of tumor treatment.
But chemotherapy, while exerting its anti-tumor therapeutic effect, often brings many adverse reactions to patients, and bone marrow suppression is one of
them.
The 2022 Chinese Society of Clinical Oncology (CSCO) Annual Meeting was held
from November 5 to 12 in a combination of online and offline mode.
This CSCO Annual Meeting includes a real-world study
evaluating the protective effects of triraciclib in myelosuppressive protection induced by chemotherapy in patients with extensive small cell lung cancer (ES-SCLC) in China.
This time, the "Medical Tumor Channel" is honored to invite Professor Chen Yongni of Hainan Provincial People's Hospital to give an in-depth interpretation and sharing
of the study and the harm of bone marrow suppression caused by chemotherapy.
Myelosuppression due to chemotherapy
Seriously affects patient efficacy
In view of the clinical manifestations that bone marrow suppression may bring, Professor Chen Yongyi introduced that bone marrow suppression is the most common side effect of tumor chemotherapy and the dose-limiting toxicity of chemotherapy drugs [1].
More than 80% of chemotherapy drugs can lead to bone marrow suppression, mainly neutrophils and thrombocytopenia, and the incidence of chemotherapy-related anemia is about 70%~90% [2].
According to the expert consensus of the Chinese Anti-Cancer Association and the Clinical Oncology Society, the concept of bone marrow suppression after chemotherapy can be divided into chemotherapy-induced neutropenia (CIN) [3], chemotherapy-induced thrombocytopenia (CIT) [4] and tumor chemotherapy-related anemia (CRA) [5].
Among them, CIN is the most common hematologic toxicity of chemotherapy drugs, and severe neutrophil decline increases the risk of invasive infection, which can lead to serious complications
such as sepsis syndrome, septic shock, and even death.
CIT refers to a common complication of tumor treatment caused by anti-tumor chemotherapy drugs that cause platelet counts in peripheral blood to be lower than normal, which may increase the risk of bleeding and endanger the patient's life and health
.
CRA mainly refers to the anemia that occurs in tumor patients during disease progression and treatment, which will lead to multi-organ ischemia and hypoxia changes and reduced immunity, which seriously affects the quality of life of patients [5].
In addition, it should be noted that CIN, CIT and CRA may lead to the reduction or delay of chemotherapy drugs during the treatment of tumor patients, which ultimately affects the efficacy of anti-tumor therapy in patients [3].
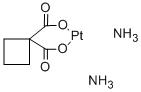
The CDK4/6 inhibitor traracillide is clinical
Bringing a "new model" of chemotherapy
Speaking of the common clinical countermeasures for myelosuppression caused by chemotherapy, Professor Chen Yongyi pointed out that the prevention and treatment methods of CRA mainly include iron supplementation, erythropoietin (EPO) and blood transfusion therapy
.
The prevention and treatment methods of CIT mainly include platelet-stimulating drugs recombinant human thrombopoietin (rhTPO), recombinant human interleukin-11 (rhIL-11) and direct platelet transfusion
.
The commonly used drug for CIN is granulocyte colony-stimulating factor (G-CSF) [2].
Chemotherapy drugs target active cells, but in addition to malignant tumor cells, normal cells such as bone marrow hematopoietic stem cells are also more active, and if chemotherapy drugs damage bone marrow hematopoietic stem cells, it will lead to multilineage myelosuppression [6].
Cyclin-dependent kinase 4/6 (CDK4/6) can be activated upon binding to cyclin D (cyclinD), promoting retinoblastoma protein (Rb) phosphorylation, which in turn promotes the cell cycle from the G1 phase to the S phase [7].
Hematopoietic stem and progenitor cells (HSPCs) in the bone marrow produce circulating neutrophils, red blood cells, and platelets, and their proliferation depends on the activity of CDK4/6 [8].
Traracillide is a highly potent, selective, and reversible CDK4/6 inhibitor that can block the progression of cells from G1 to S phase, inducing HSPC and lymphocyte temporary arrest in G1 phase
.
Application before chemotherapy can temporarily stop cell division, avoid the killing of chemotherapy drugs, avoid bone marrow depletion, protect bone marrow hematopoietic function, and do not affect the anti-tumor treatment efficacy
of chemotherapy.
At present, most of the treatments for myelosuppression can only treat monophyletic myelosuppression, and existing studies have shown that triracillide has a comprehensive protective effect on granulocytes, platelets and red blood cells, and is the world's first drug
with a full bone marrow protective effect administered before chemotherapy.
The CSCO Annual Meeting announces real-world research
Traraciclib is also available in patients with combinations
Benefits
This year's CSCO Annual Meeting included a real-world study conducted by Professor Chen Yongyi and his team evaluating the protective effect of triracillide on chemotherapy-induced myelosuppressive protection in ES-SCLC patients [9].
In response to the results of this real-world study, Professor Chen shared that the main purpose of this real-world study is to evaluate the protective effect
of triracillide on chemotherapy-induced bone marrow suppression in Chinese ES-SCLC patients.
A total of 30 (26 male) patients with ES-SCLC were included, 26 received tramaxilide plus etoposide plus platinum (EP, 2 second-line), 20 of whom were combined with 4 PD-(L)1 inhibitors and 4 were treated with topotecan (TPT) ≥ 2-line therapy
.
The median treatment cycle of triraciclib was 3.
0 (2.
0, 5.
0) cycles, and only 7 patients started triraciclib
from the first cycle of chemotherapy.
The incidence of severe neutropenia (SN) in the first treatment cycle after traracillide was 1 in 30 (3.
3%), and SN occurred
in only 1 patient receiving TPT.
Afebrile neutropenia (FN).
The incidence of grade 3/4 hematologic adverse events was 20.
0%, and the EP and TPT regimens were 11.
5% and 75.
0%,
respectively.
Grade 3/4 neutrophil counts were low, platelet counts were low, and anemia occurred in 16.
7%, 10.
0%, and 10.
0%,
respectively.
Grade 4 thrombocytophonia was recorded in one case in EP and one case in TPT regimens.
No patients reported grade 4 anaemia
.
10.
0% of patients (7.
7% EP and 25.
0% TPT) received intravenous or oral antibiotics
.
16.
7% of patients received G-CSF, compared with 11.
5% and 50.
0%
of patients receiving EP and TPT regimens, respectively.
The cumulative incidence of SN for all treatment cycles after triracillide was 6.
7%, 3.
8% with EP regimen, 25.
0% with TPT regimen, and FN
was not reported.
The incidence of grade 3/4 hematologic adverse events was 36.
7%, and the EP and TPT regimens were 26.
9% and 100.
0%, respectively.
Grade 3/4 neutrophil count is low, platelet count is low, and anemia occur in 30.
0%, 10.
0%, and 13.
3%,
respectively.
Grade 3/4 platelet counts were not seen in first-line EP patients, and grade 4 anemia
was not seen in all patients.
The incidence of intravenous or oral antibiotics was 13.
3%, with EP and TPT regimens 11.
5% and 25.
0%, respectively; 26.
7% of patients received G-CSF
.
The incidence of adverse events (TEAEs) during treatment was 93.
3%, the incidence of ≥grade 3 TEAE was 46.
7%, and the incidence of drug-related TEAE was 33.
3%, all chemotherapy-related
.
The incidence of any SAE is 30%.
Chemotherapy drug reduction occurred in 26.
7% of patients
.
There are no ≥ grade 3 AEs, SAEs associated with traracicillide, and AEs
that cause death.
In this real-world study, the utility of triracillide in combination with chemotherapy was explored, as well as the utility of triracillide in patients receiving immunotherapy in combination chemotherapy
.
In addition, the study included patients receiving 1-3 lines of different treatments, including some patients who had previous myelosuppression and relatively poor bone marrow function, and not all patients were combined with trilacilride in the first cycle of chemotherapy, indicating that trilacilride has a myeloprotective effect
on patients in the real world for different cycles of combination chemotherapy.
A number of studies at home and abroad have confirmed that triracillide can be
ES-SCLC patients reduce the burden of chemotherapy
In July 2022, triracillide received conditional approval in China for use in ES-SCLC patients who have not previously received systemic chemotherapy for prophylactic administration prior to EP regimen therapy to reduce the incidence
of chemotherapy-induced myelosuppression.
In addition, the 2022 CSCO SCLC guidelines have added bone marrow protective drugs to the internal medicine section, and triracillide has been added as a level II recommendation (class 2A)
for first-line and second-line ES-SCLC treatment.
Professor Chen Yongyi said that in three phase II clinical studies abroad, the G1T28-02 study [10] showed that the administration of traracillide to ES-SCLC patients before first-line carboplatin + etoposide treatment could reduce the duration of SN in the first cycle from 3 days to 0 days, and the incidence of SN from 43.
2% to 5.
3%
compared with the placebo group.
The G1T28-05 study [11] showed that traracillide given to patients with ES-SCLC prior to first-line treatment with carboplatin + etoposide + atezolizumab reduced the duration of SN from 4 days to 0 days and the incidence of SN from 49.
1% to 1.
9%
compared with placebo.
The G1T28-03 study [12] showed that traracillide given to patients with ES-SCLC prior to second- and third-line topotecan therapy reduced the duration of SN from 7 to 2 days and the incidence of SN from 75.
9% to 40.
6%
compared with placebo.
A pooled analysis of the G1T28-02 study, the G1T28-05 study, and the G1T28-03 study [13] showed that traracillide significantly reduced haematoxitoxicity due to chemotherapy and reduced haematoxitoxicity-related drug administration and chemotherapy drug reduction due to haematological toxicity
.
Another post-hoc analysis of these three studies, presented at this year's American Society of Clinical Oncology (ASCO) Annual Meeting [14], showed that patients receiving triracillide had fewer myelosuppressive events
due to monolineage and bilineage and trilineage concurrent chemotherapy compared with placebo patients.
Similar trends
can be observed in patients receiving second- and third-line therapy.
In addition, the TRACES study evaluated the safety, efficacy, and pharmacokinetic (PK) data of traracillide in combination with standard chemotherapy in Chinese patients with ES-SCLC [15], including an open-label safety trial component (Part 1) and a double-blind, placebo-controlled portion (Part 2).
The results of the Part 1 study showed that triracillide was comparable
to Western patient data in terms of PK, safety, and bone marrow protection in Chinese patients.
The Part 2 data showed that triracillide before chemotherapy was significantly reduced in the duration of Cycle 1 SN compared with placebo (0 days vs.
2 days, P=0.
0003).
。 Traracillide improved the duration of SN in the first cycle 1 compared with placebo, and was well tolerated by patients receiving either first-line EP (0 days vs.
2 days, P=0.
0021) or second-line TPT (1 day vs.
2 days, P=0.
0418), with fewer grade ≥ 3 adverse events and no fatal adverse events
associated with triracillide.
The real-world study data also confirmed that triracillide has a good overall myeloprotective effect in Chinese ES-SCLC patients receiving a variety of treatment regimens, consistent with the efficacy trend of previous studies at home and abroad, with good safety and no new safety signals
.
Traraciclib protects bone marrow from the source, and it is believed that this new whole bone marrow protector will be widely used in the future to benefit more ES-SCLC patients
.
Professor Chen Yongyi
Chief physician Master tutor
Deputy Director of the Department of Respiratory and Critical Care Medicine, Hainan Provincial People's Hospital
Deputy Director of the Department of Internal Medicine, School of Clinical Medicine, Hainan Medical College
Director of Hainan Respiratory Medicine Quality Control Center
Vice Chairman of the Respiratory Professional Committee of Hainan Medical Association
Member of Lung Cancer Prevention and Control Branch of China Association for the Promotion of International Medical Exchanges
Member of the Thoracic Science Group of the Smart Medical Committee of the World Association of Chinese Physicians
References:
[1] Epstein RS, Aapro MS, Basu Roy UK, et al.
Patient Burden and Real-World Management of Chemotherapy-Induced Myelosuppression: Results from an Online Survey of Patients with Solid Tumors[J].
Adv Ther.
2020, 37(8):3606-3618.
[2] Chinese Society of Clinical Oncology (CSCO) Expert Committee of Integrated Traditional Chinese and Western Medicine, et al.
Expert consensus on the diagnosis and treatment of integrative medicine of integrative medicine caused by antitumor drugs caused by bone marrow suppression[J].
Journal of Clinical Oncology,2021,26(11):1020-1027.
)
[3] SHI Yanxia, XING Junyuan, ZHANG Jun, et al.
Expert consensus on the diagnosis and treatment of neutropenia caused by tumor chemotherapy (2019 edition)[J].
Chinese Clinical Oncology, 2019, 46(17): 876-882.
)
Chinese expert consensus on the diagnosis and treatment of thrombocytopenia caused by cancer chemotherapy (2018 edition)[J].
Chinese Journal of Oncology, 2018, 40(09): 714-720.
)
[5] SHI Yanxia, XING Fenyuan, ZHANG Jun, et al.
Chinese expert consensus on the diagnosis and treatment of chemotherapy-related anemia in oncology (2019 edition)[J].
Chinese Clinical Oncology,2019,46(17):869-875.
)
[6] Li C, Hart L, Owonikoko TK, et al.
Trilaciclib dose selection: an integrated pharmacokinetic and pharmacodynamic analysis of preclinical data and Phase Ib/IIa studies in patients with extensive-stage small cell lung cancer.
Cancer Chemother Pharmacol.
2021, 87(5):689-700.
[7] Shapiro GI.
Cyclin-dependent kinase pathways as targets for cancer treatment[J].
J Clin Oncol.
2006, 24(11):1770-83.
[8] Bisi JE, Sorrentino JA, Roberts PJ, Tavares FX, Strum JC.
Preclinical Characterization of G1T28: A Novel CDK4/6 Inhibitor for Reduction of Chemotherapy-Induced Myelosuppression[J].
Mol Cancer Ther.
2016, 15(5):783-93.
CHEN Yongyan, MENG Chong, LIU Lirong, et al.
Traracillide's first real-world study in patients with extensive-stage small cell lung cancer in China: Results of a real-world study from the Boao Lecheng International Medical Tourism Pilot Zone in Hainan.
2022 CSCO
[10] Weiss JM, Csoszi T, Maglakelidze M, et al.
Myelopreservation with the CDK4/6 inhibitor trilaciclib in patients with small-cell lung cancer receiving first-line chemotherapy: a phase Ib/randomized phase II trial[J].
Ann Oncol.
2019,30(10):1613-1621.
[11] Daniel D, Kuchava V, Bondarenko I, et al.
Trilaciclib prior to chemotherapy and atezolizumab in patients with newly diagnosed extensive-stage small cell lung cancer: A multicentre, randomised, double-blind, placebo-controlled Phase II trial [J].
Int J Cancer.
2020 ,148(10):2557–70.
[12] Hart LL, Ferrarotto R, Andric ZG, et al.
Myelopreservation with Trilaciclib in Patients Receiving Topotecan for Small Cell Lung Cancer: Results from a Randomized, Double-Blind, Placebo-Controlled Phase II Study[J].
Adv Ther.
2021,38(1):350-365.
[13] Weiss J, Goldschmidt J, Andric Z, et al.
Effects of Trilaciclib on Chemotherapy-Induced Myelosuppression and Patient-Reported Outcomes in Patients with Extensive-Stage Small Cell Lung Cancer: Pooled Results from Three Phase II Randomized, Double-Blind, Placebo-Controlled Studies.
Clin Lung Cancer.
2021 Sep; 22(5):449-460.
[14] Jerome HG, et al.
Impact of trilaciclib on multilineage chemotherapy-induced myelosuppression events in patients with extensive-stage small cell lung cancer: Post-hoc analyses of data from randomized clinical trials.
2022 ASCO, Abstract 8568.
[15] Ying Cheng, Lin Wu, DingZhi Huang.
Myeloprotection with Trilaciclib in Chinese Patients with Extensive-Stage Small Cell Lung Cancer Receiving Standard Chemotherapy (TRACES).
2022 WCLC, Abstract EP08.
02-078.