-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Accelerating the development of the COVID-19 vaccine to improve efficiency and avoid wasted resources requires public-private sector cooperation and platforms that can overall co-ordinate clinical trials.
response to SARS-CoV-2, the long-term solution is to successfully develop a safe, effective and controllable quality vaccine, through mass vaccination active prevention, to protect countries from SARS-CoV-2. The specific needs of vaccines in different countries and regions around the world, as well as the wide geographical diversity of THE COVID-19 epidemic, require multiple effective vaccine development paths. The collaboration between biotechnology companies and pharmaceutical companies is critical. In order to effectively prevent SARS-CoV-2 infection, it depends on the complete research and development path of effective vaccine research and development, so industry, government and academia are required to work together to complement each other's strengths and win-win cooperation.
April, at the critical juncture of the COVID-19 pandemic, the National Institutes of Health (NIH) announced extensive collaboration between several federal research institutions and 16 pharmaceutical companies to coordinate and accelerate the development of COVID-19 therapeutic drugs and vaccines through the public-private partnership model. Recently, Fred Hutchinson Cancer Research Center, Professor of Medicine and Testing Medicine at the University of Washington, Founder of the HIV Vaccine Clinical Trials Network, Dr. Lawrence Corey, Dr. John R. Mascola of the National Institute of Allergy and Infectious Diseases (NIAID) Vaccine Research Center, Dr. Anthony Fauci, Director of NIAID, Dr. Francis S. Collins, Director of NIH, co-authored an article in the Journal of Science detailing the ACT IV program and the program's progress.partnership, called ACTIV, will establish a collaborative framework that prioritizes vaccines and drug candidates, streamlines clinical trials, coordinates registration processes, and integrates, integrated, leveraged, and synergies, to achieve the goal of rapidresponse to the COVID-19 pandemic and possible future pandemics through effective cooperation mechanisms. ACTIV plans to use a parallel and parallel approach to generate basic safety and efficacy data for several candidate vaccines, accelerate the development of multiple vaccine platforms, and accelerate the goal of vaccine approval and distribution.
THE ACTIV PROGRAM HAS FOUR FAST-TRACK AREAS OF INTEREST, EACH LED BY A ROBUST WORKING GROUP OF SENIOR SCIENTISTS REPRESENTING GOVERNMENT, INDUSTRY AND ACADEMIA. For each fast track, there are specific refinements to the ground.
.
, details of the protective immune response to SARS-CoV-2 are not yet known. Data from patients infected with SARS-CoV-1 and patients with recent SARS-CoV-2 confirm edifying a relatively high immune response after infection, especially antibody response stomping proteins that mediate the virus into cells. However, there is a lack of understanding of the type or level of invivia required to prevent subsequent reinfection, as well as the potential duration of the associated protection. In the animal model of SARS-CoV-1, the use of recombinant sub-proteins against viruses, nucleic acid-vector vaccines, and the passive transfer of neutralizing antibodies to the stingproteins have been shown to be protective of experimental infections. But protecting against infection, regulating virus replication, and changing the end of the disease process vary. The data give the optimistic that a highly immunogenic vaccine will produce the antibody response required for protection in a quality and quantity. But there is a lack of understanding of the role of T-cell immunity in preventing early infections or improvements, both in animal challenge models and in human coronavirus diseases. These factors are the reason why vaccines cannot be targeted only in vaccine development.
is the most important goal for any vaccine that is used for wide vaccination. Theoretically, there is a risk of increased SARS-CoV-2 infection after vaccination if given a defective vaccine. There have been reports of coronavirus infection in cats, and this phenomenon has been observed in some SARS-CoV-1 vaccine challenge animal models. These preclinical data show that the increase in respiratory syndrome associated with the vaccine is caused by poor protective antibodies (producing immune complex deposits) and the immune response of TH2-assisted cell bias. There is a need for a more in-depth exploration of the potential mechanisms of vaccine-induced immune enhancement and ways to minimize this risk. Therefore, it is very important to construct the correct antigen that can trigger the structural correct antibody that is functionally effective. This is an important lesson learned from the occurrence of vaccine-induced lower respiratory diseasein in infants who were vaccinated against for the inactivated respiratory syncytial virus (RSV) in Formarin in the late 1960s. Animal models of SARS-CoV-2 infection are being developed and are expected to better understand the protective-related immune response through these animal models.
how to define the main endpoints of the effectiveness of the COVID-19 vaccine also needs to be discussed. The two most frequently mentioned cases include: (1) prevention of infections defined by serum transformation (also known as impotence, seroconversion) and (2) prevention of diseases with clinical symptoms, in particular improving the severity of the disease, including the frequency of diseases requiring intensive medical care; This requires a careful assessment of the severity of vaccination on the various epidemiological and medical settings of COVID-19 disease in the young and older population, as well as in minorities with inadequate medical care. All these issues need to be assessed under these initial effectiveness test conditions. Reaching these endpoints may also be associated with reduced vector-based transmission rates.
estimates that asymptomatic infections account for 20 to 40 per cent of total cases of COVID-19, so more enrollees are involved in clinical trials as the main endpoint associated with reducing disease. Initial effectiveness trials may require a large number of initial registrations, while continuous monitoring of serological and clinical endpoints. The lack of an accurate understanding of morbidity leads to a certain degree of complexity in the development of clinical trialprogrammes at serological endpoints, which is a major challenge for all. A key requirement of this multi-trial strategy is the establishment of independent laboratories with similar or identical validation serological trials to establish a coordinated bridge between multiple vaccine products and multiple vaccine efficacy trials. These laboratories should be required in all clinical trials, or key specimens from the trials should be shared. The parameters of distinguishing the immune response from vaccination from the immune response caused by infection are being studied in depth, and there is an urgent need to develop trials to address this problem.
need to comprehensively evaluate vaccine effectiveness trials from a benefit and risk perspective. The likelihood of REexposure of SARS-CoV-2 is much higher than that of SARS-CoV-1, which disappears from community transmission, so a long-term assessment of the potential enhancement of reexposure is required. This requirement does not conflict with approval based on the above e-end; Since decreased immunity can often be observed in people with coronavirus infection, it is necessary to continue to explore the persistence of clinical and serological endpoints. The coronavirus has a single-stranded RNA genome with a relatively high mutation rate. Although there have been some genetic drifts during the evolution of the SARS-CoV-2 outbreak, no significant variation of sting protein has been observed so far, especially in areas where antibodies are neutral;
.
suggested that a controlled human challenge trial could be conducted, with a small number of volunteers vaccinated and then using the SARS-CoV-2 challenge. Such experiments may be useful if they are designed to define potential immunocorrelations or to screen for less effective vaccine methods. However, this approach is flawed in terms of pathophysiology and safety. Although the risk of serious illness or death in young healthy individuals with COVID-19 is relatively low, it is not zero; The SARS-CoV-2 is designed to challenge the virus strain and cause mild illness in most volunteers and may not be repeated with the pulmonary pathophysiology symptoms observed in some patients. In addition, some of the efficacy in young healthy adults cannot predict similar efficacy in older populations with major secondary factors associated with COVID-19 disease, nor can it be demonstrated to reduce transmission among the main susceptible populations. Whether such trials are worth continuing, or whether they will have a beneficial impact on the vaccine development schedule, will require a careful assessment by an independent team of ethicists, clinical trial experts and vaccine development experts.
encouraging is the rapid progress in the development of a number of vaccines and the progress of several major vaccine platforms towards clinical evaluation. These include traditional recombinant proteins, replication and non-replicated viral vectors, as well as nucleic acid DNA and mRNA methods. These vaccine platforms have their own advantages and limitations. Key features of these vaccine platforms include speed of production and production flexibility, safety and reactive, body fluids and cellular immunogenicity characteristics, immune continuity, production scale and cost, vaccine stability, and cold chain requirements. No vaccine or vaccine platform can meet global needs alone, so a multi-pronged strategic approach is critical.
several companies are developing nucleic acid-based vaccines, including Moderna, BioNTech/Pfizer, CuraVac (mRNA-based) and Inovio (DNA-based). DNA vaccines and mRNA vaccines can be produced quickly based on virus sequences and are therefore progressing rapidly. Currently, the optimal immunogenicity of DNA requires an electro-perforation or syringe delivery device that allows DNA to enter cells. The mRNA vaccine uses lipid nanoparticles to protect and deliver mRNA, which can be effectively used as an adjugate of immunogens. However, the amplification and temperature stability of these lipid nanoparticles need to be solved. Although the early clinical experience of nucleic acid vaccines is very rich, no vaccine has been licensed for widespread use. Thus, while there is no shortage of optimistic hope ahead, there are still some uncertainties that need to be assessed as soon as possible for the immunogenicity and safety of these products, while addressing the problems faced by lack of business experience.
Sanofi, Novavax is developing a vaccine that uses traditional recombinant protein technologies to express the stinging protein, and although it takes longer to establish a cell line than a nucleic acid vaccine, it has been approved for protein and protein granule vaccines, including hepatitis B, human papvirus, chickenpox-shingles and influenza vaccines, with robust and reliable commercial experience. Protein vaccines require an effective adjuvant, which is essential for inducing an immune response to TH1;
virus vector vaccine sits the gene code of the virus of concern into one of several carriers with good characterization, including adenovirus (Ad) and blister-type oral itisvirus (VSV). Replication of defective adenovirus 26 (rAd26), which is effective against Ebola virus infection, has recently been shown to prevent Ebola virus infection, and Johnson and Johnson is developing rAd26 for COVID-19. The platform has the potential for mass production. The problem that pre-existing immunity (preexisting immunity) for possible specific viral vectors may weaken immunogenicity needs to be addressed in early trials. The recombinant chimpanzee AdOx1, developed by Oxford University and AstraZeno, has also entered clinical trials. A similar version of the ChAd vaccine product. Tests have been conducted in previous clinical trials to demonstrate safety and immunogenicity. The VSV vector vaccine platform has the ability to replicate, so it can be used to induce robust and reliable single dose, and may have a long-lasting immune response. The VSV Ebola vaccine produced by Mercado has been approved and is very effective after single-dose inoculation, although its response to the vaccine may be limited in some populations. These different methods offer the potential to amplify production for large-scale vaccination of the relevant vaccines.
under the ACTIV Public Sector-Private Sector Partnership Program, NIH works with a number of agencies under the Department of Health and Human Services (HHS), including the Food and Drug Administration (FDA), the Centers for Disease Control and Prevention (CDC) and the Biomedical Advanced Research and Development Authority (BARDA); This open forum enables discussionand discussions and consensus on vaccine trial design, rapid data sharing and close public-private sector cooperation for rapid and effective research into vaccine efficacy. There is a consensus that vaccine trials require the use of a common independent laboratory, or the provision of samples and data to produce alternative markers (alternative endpoints), which will eventually speed up approval and a comprehensive comparison of effectiveness. The Common Ethics Review Board (IRB) and the Common Cross-Test Data and Security Monitoring Committee (DSMB) should be used to coordinate regulatory frameworks for all developers so that regulators and the public can objectively assess the size of the effects between different paths. As the candidate vaccine prepares to enter Phase 1 clinical, phase 3 clinical planning must be specifically planned. While much of the focus is on trials across the United States, the COVID-19 prevention network under the ACTIV programme has a global focus and must also be coordinated with the World Health Organization (WHO), the Alliance for Epidemic Innovation Alliance and other global partner groups.
the need to coordinate the overall programme in order to be able to conduct an open and transparent evaluation of the relative effectiveness of each vaccine approach. Such coordination is best achieved through public-private partnerships such as ACTIV to gain government-supported centres.




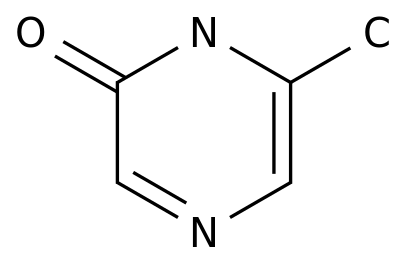
![2-(Hydroxymethyl)benzo[b]thiophene](https://file.echemi.com/fileManage/upload/cas/593/e79a972f-b55d-4dc1-9113-841c417e0a89.png)