-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*For medical professionals only
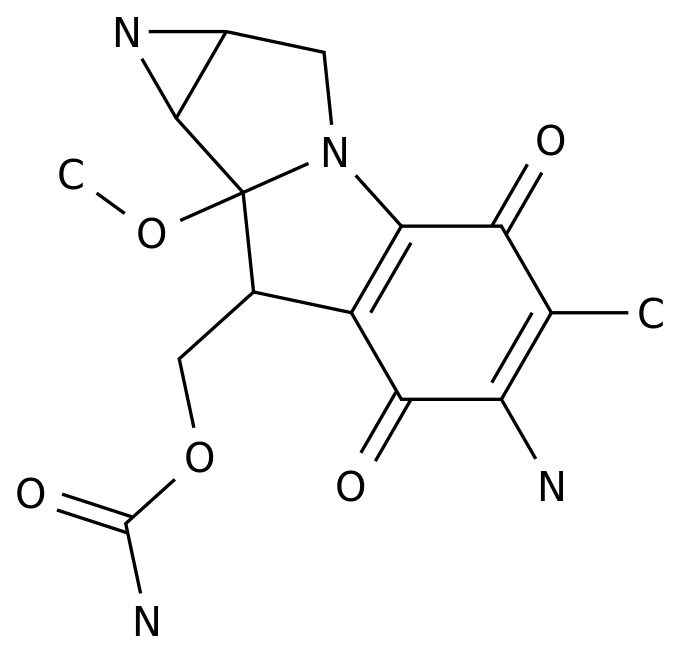
Ositinib is a weapon in the treatment of lung cancer, and corresponding resistance treatment regimens
As a third-generation EGFR-TKI, the emergence of ositinib solves the problem of drug resistance of the first/second generation of EGFR-TKI, and has become a "life-saving straw"
Previously, we have shared with you the main resistance mechanism of ositinib C797S and MET amplification coping strategies, this article will continue to introduce the occurrence and solution of HER2 amplification/mutation after the first-line treatment of ositinib drug resistance, so that clinicians can "worry about drug resistance", rest assured that "good drugs come first", and ultimately better benefit the majority of lung cancer patients
First-line treatment of oxitinib, refreshing PFS and OS history
The FLAURA study is a randomized, controlled, multicenter, double-blind, phase III clinical trial designed to explore ositinib versus first-line treatment of locally advanced or metastatic NSCLC patients with
Data from the FLAURA study show that the first-line treatment of ositinib in patients with EGFR mutation-positive advanced NSCLC significantly prolongs PFS to 18.
Figure 1.
Oshitinib also has advantages
Figure 2.
At present, a number of authoritative guidelines at home and abroad recommend ositinib as the standard first-line treatment for patients with positive EGFR mutation, of which the National Comprehensive Cancer Network (NCCN) guidelines are the preferred recommendation, the European Society of Internal Oncology (ESMO) guidelines are IA and the highest score recommended, and the Chinese Society of Clinical Oncology (CSCO) guidelines are recommended
for Class I.
Figure 3.
First-line treatment of ositinib is unanimously recommended by domestic and foreign guidelines
HER2 amplification/mutation with oxitinib first-line treatment resistance
HER2 is a tyrosine kinase receptor that belongs to the EGFR family
.
Among the different HER family proteins, HER2 has the strongest catalytic kinase activity [3,4].
Its phosphorylation can lead to downstream activation of the PI3-Akt, MAPK, and ERK MET/MAPK pathways [5-7
].
HER2 variants in NSCLC mainly include both amplification and mutation, both of which lead to HER2 activation [8].
The HER2 variant is the oncogenic driver gene of NSCLC and an important mechanism
for acquired resistance to EGFR-TKI.
Clinical studies have shown that the HER2 variant is one of the mechanisms of acquired resistance to ositinib
.
In the FLAURA study, after first-line resistance to ositinib, HER2 amplification occurred in 2% of patients and HER2 mutation in 1% of patients [9
].
In addition, AURA3 studies have shown that HER2 amplification occurs in 5% of patients with first-line resistance to ositinib, and that some patients have other target mutations [10].
However, HER2 amplification is more common after first-line resistance to EGFR-TKI (erlotinib, gefitinib) in a 10% incidence [11].
Figure 4.
Occurrence of mutations and amplification of TKI resistance in the EGFR mutation NSCLC [12].
See the trick to crack the HER2 amplification/mutation after the first-line treatment of ositinib first-line drug resistance
So how should patients with advanced NSCLC with HER2 amplification/mutation after first-line treatment of oxitinib be treated clinically? At present, a number of studies have explored this, and a variety of treatment options such as anti-HER2 monoclonal antibodies, TKI drugs, and antibody-conjugated drugs (ADCs) have shown good application prospects
.
01
Anti-HER2 monoclonal antibody
A single-armed, phase II study evaluating the efficacy and safety of trastuzumab plus paclitaxel in patients with HER2-expressing NSCLC after the progression of EGFR-TKI therapy found that the overall objective response rate (ORR) was 46 percent and that a 100 percent response rate was observed in four patients with HER2 amplification (>10 copies/nucleus) [13].
02
TKI class drugs
Pirrolitinib is an irreversible pan-HER tyrosine kinase inhibitor (TKI) targeting EGFR/HER1, HER2 and HER4
.
A phase II study included 60 patients with HER2 exon insertion mutations who had received at least one platinum-containing regimen of chemotherapy for stage IIIB and IV NSCLC receiving 400 mg of pyrrotinib daily
.
The results showed that pyrrotinib monotherapy had acceptable safety features and promising antitumor activity with an ORR of 30%; The median PFS was 6.
9 months and the median OS was 14.
4 months
.
The phase II PATHER2 study further explored the treatment of pyrrottinib plus the anti-angiogenic drug apatinib for HER2 amplification or mutated advanced NSCLC, and the results showed that the ORR of pyrrrotinib plus apatinib was 45.
5%, and the disease control rate (DCR) was 93.
9% [15].
In addition, a phase II ZENITH20-2 study showed that another pan-HER-TKI class drug, Poziotinib, had an ORR of 28% and a median PFS of 5.
5 months for post-the-line treatment of HER2-20 exon insertion into the mutation NSCLC [16].
03
ADC class drugs
Trastuzumab emtansine (T-DM1) is an ADC class of drugs
consisting of anti-HER2 antibodies, non-cuttable connectors, and payloads.
Preclinical studies have shown that T-DM1 may overcome ositinib resistance [17].
A phase II study included patients who had previously received EGFR-TKI, treated with T-DM1, and observed partial remission (PR) in four patients with HER2 immunohistochemistry (IHC)3+ with an ORR of 20% [18].
In addition, a phase II "basket" study found that in 18 patients with HER2 mutant lung cancer who received multi-line therapy, the ORR treated with T-DM1 was 44% and the median PFS was 5 months [19].
Another ADC-class drug, Trastuzumab deruxtecan (T-DXd), also showed good antitumor activity
in patients with HER2 expression or HER2 mutation NSCLC.
In a cohort of patients with HER2 expression or HER2 mutation NSCLC in a phase I study, the ORR treated with T-DXd was 55.
6% and the median PFS was 11.
3 months [20].
The phase II DESTINY-Lung01 study showed that T-DXd had a confirmed ORR of 55% and a median PFS of 8.
2 months in patients with HER2 mutation NSCLC who had received the current standard of care [21].
In addition, the Phase II DESTINY-Lung02 study included patients with non-squamous NSCLC who had unresectable or metastatic HER2 mutations who progressed after previous systemic therapy
and were given T-DXd.
In the primary efficacy analysis cohort of 52 patients, the ORR was 58% and the median duration of remission (DOR) was 8.
7 months [22].
Based on the results of this study, T-DXd was approved by the U.
S.
Food and Drug Administration in August 2022 for use in adults with HER2 mutation unresectable or metastatic NSCLC who had previously received systemic therapy, becoming the first therapeutic drug
approved for HER2 mutation NSCLC.
04
other
In addition to anti-HER2 therapy, immunotherapy also shows some clinical activity in the HER2 mutation NSCLC
.
One retrospective study found that the first-line treatment of HER2-mutant NSCLC with immunocompromise chemotherapy had an ORR of 52% and a median PFS of 6 months [23].
The HER2 16 exon jumping mutation is a novel mechanism of ositinib resistance, and in vitro studies have shown that afatinib combined with ositinib can inhibit tumor cell growth and signaling [24,25].
Expert comments: A variety of new drugs and new solutions have emerged, and the prospect of ositinib resistance caused by HER2 amplification/mutation is promising
HER2 amplification/mutation is an important mechanism of ositinib resistance, and in the past, the clinical treatment of such patients was mainly chemotherapy, but the effect was not ideal
.
At present, although there is no consensus on the treatment of acquired HER2 amplification/mutation after oximinib resistance, with the continuous development of various new drugs and new programs, more choices
have been brought to clinical treatment.
For example, anti-HER2 monoclonal antibody trastuzumab, TKI drugs pirrotinib and Poziotinib, ADC drugs T-DM1 and T-DXd, immunotherapy and ositinib combination regimen, etc.
, have shown promising anti-tumor activity in clinical studies, and T-DXd has been approved by the US FDA for HER2 mutation NSCLC therapy
.
In the future, it is expected that these new drugs and new programs can carry out more research, and continue to accumulate evidence-based medical evidence for patients with HER2 amplification/mutation NSCLC after ositinib resistance, providing guidance
for clinical treatment.
Professor Cai Yong
Deputy Director of the Department of Radiotherapy, Shanghai Pulmonary Hospital, Tongji University
Chief Physician Master Supervisor Doctor of Medicine
He is a standing committee member of the Pulmonary Oncology Committee of the Chinese Medical Education Association
Standing Committee Member of the Stereotactic Special Committee of the Chinese Lung Cancer Prevention and Control Alliance
Member of the Tumor Radiotherapy Committee of Wu Jieping Medical Foundation
He is a member of the Lung Cancer Working Committee of the World Association of Chinese Oncologists
Director of Soong Ching Ling Foundation Oncology Medical Care and Regional Industry-University-Research Alliance
He is a member of the Precision Medicine Branch of the Chinese Society of Gerontology and Geriatrics
Member of the Radiation Therapy Youth Committee of Shanghai Anti-Cancer Association
Member of Shanghai Medical and Health Youth Federation
References:
[1].
Soria JC, Ohe Y, Vansteenkiste J, et al.
Osimertinib in Untreated EGFR-Mutated Advanced Non-Small-Cell Lung Cancer.
N Engl J Med.
2018 Jan 11; 378(2):113-125.
[2].
S.
S.
Ramalingam, J.
E.
Gray, Y.
Ohe, et al.
Osimertinib vs comparator EGFR-TKI as first-line treatment for EGFRm advanced NSCLC (FLAURA): Final overall survival analysis.
Annals of Oncology (2019) 30 (suppl_5): v851-v934.
[3].
Hsu C-C, et al.
Exon 16–Skipping HER2 as a Novel Mechanism of Osimertinib Resistance in EGFR L858R/T790M–Positive Non–Small Cell Lung Cancer.
J.
Thorac.
Oncol.
2019, 15,
50–61.
[4].
Yan M, et al.
R.
HER2 expression status in diverse cancers: Review of results from 37,992 patients.
Cancer Metastasis Rev.
2015, 34, 157–164.
[5].
Planchard D, et al.
Correction to: “Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up”.
Ann.
Oncol.
2019, 30, 863–870.
[6].
Lamberti G, et al.
Beyond EGFR, ALK and ROS1: Current evidence and future perspectives on newly targetable oncogenic drivers in lung adenocarcinoma.
Crit.
Rev.
Oncol.
2020, 156, 103119.
[7].
Paez J G, et al.
EGFR Mutations in Lung Cancer: Correlation with Clinical Response to Gefitinib Therapy.
Science 2004, 304, 1497–1500.
[8].
Midha A, et al.
EGFR mutation incidence in non-small-cell lung cancer of adenocarcinoma histology: A systematic review and global map by ethnicity (mutMapII).
Am.
J.
Cancer Res.
2015, 5, 2892–2911.
[9].
Ramalingam S.
S, et al.
Mechanisms of acquired resistance to first-line osimertinib: Preliminary data from the phase III FLAURA study.
Ann.
Oncol.
2018, 29, viii740.
[10].
Papadimitrakopoulou V.
A, et al.
Analysis of resistance mechanisms to osimertinib in patients with EGFR T790M advanced NSCLC from the AURA3 study.
Ann.
Oncol.
2018, 29, viii741.
[11].
Wu SG, Shih JY.
Management of acquired resistance to EGFR TKI-targeted therapy in advanced non-small cell lung cancer.
Mol Cancer.
2018; 17(1):38.
[12].
Johnson M, et al.
Treatment strategies and outcomes for patients with EGFR-mutant non-small cell lung cancer resistant to EGFR tyrosine kinase inhibitors: Focus on novel therapies.
Lung Cancer.
2022; 170:41-51.
[13].
de Langen AJ, Jebbink M, Hashemi SMS, et al.
Trastuzumab and paclitaxel in patients with EGFR mutated NSCLC that express HER2 after progression on EGFR TKI treatment.
Br J Cancer 2018; 119:558–564.
[14].
Zhou C, Li X, Wang Q, et al.
Pyrotinib in HER2-Mutant Advanced Lung Adenocarcinoma after Platinum-based Chemotherapy: A Multicenter, Open-label, Single-arm, Phase II study.
J Clin Oncol.
2020; 38(24):2753-61.
[15].
Yang G, Xu H, Yang L, et al.
Efficacy and safety of pan-ErbB inhibitor pyrotinib combined with antiangiogenic agent apatinib for HER2-mutant or amplified metastatic NSCLC: a phase II clinical study.
J Clin Oncol 2021; 39(15 Suppl):9035.
[16].
Le X, Cornelissen R, Garassino M, et al.
Poziotinib in Non-Small-Cell Lung Cancer Harboring HER2 Exon 20 Insertion Mutations After Prior Therapies: ZENITH20-2 Trial.
J Clin Oncol.
2022; 40(7):710-718.
[17].
S.
La Monica, D.
Cretella, M.
Bonelli, et al.
Trastuzumab emtansine delays and overcomes resistance to the third-generation EGFR-TKI osimertinib in NSCLC EGFR mutated cell lines, J.
Exp.
Clin.
Cancer Res.
36 (1) (2017) 174.
[18].
S.
Peters, R.
Stahel, L.
Bubendorf, et al.
Trastuzumab Emtansine (TDM1) in Patients with Previously Treated HER2-Overexpressing Metastatic NonSmall Cell Lung Cancer: Efficacy, Safety, and Biomarkers, Clin Cancer Res 25 (1) (2019) 64–72.
[19].
B.
T.
Li, R.
Shen, D.
Buonocore, et al.
Ado-Trastuzumab Emtansine for Patients With HER2-Mutant Lung Cancers: Results From a Phase II Basket Trial, J.
Clin.
Oncol.
36 (24) (2018) 2532–2537.
[20].
J.
Tsurutani, H.
Iwata, I.
Krop, et al.
Targeting HER2 with Trastuzumab Deruxtecan: A Dose-Expansion, Phase I Study in Multiple Advanced Solid Tumors, Cancer Discov, 2020.
[21].
B.
T.
Li, E.
F.
Smit, et al.
Trastuzumab Deruxtecan in HER2-Mutant Non-Small-Cell Lung Cancer, N Engl J Med.
386 (3) (2022) 241–251.
[22].
Saalfeld FC, Wenzel C, Christopoulos P, et al.
Efficacy of immune checkpoint inhibitors alone or in combination with chemotherapy in NSCLC harboring ERBB2 mutations.
J Thorac Oncol 2021.
S1556-0864(21)02292-9.
[24].
Offin M, Somwar R, Rekhtman N, et al.
Acquired ALK and RET gene fusions as mechanisms of resistance to osimertinib in EGFR-mutant lung cancers.
JCO Precis Oncol 2018; 2:1–12.
[25].
Zeng L, Yang N, Zhang Y.
GOPC-ROS1 rearrangement as an acquired resistance mechanism to osimertinib and responding to crizotinib combined treatments in lung adenocarcinoma.
J Thorac Oncol 2018; 13:e114–e116.