-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Hello everyone, and welcome to the lymphoma micro-class
.
I am Dr.
Feng Ru from the Nanfang Hospital of Southern Medical University
.
What I share with you today is: Ibrutinib can improve the efficacy of chimeric antigen receptor T cell (CAR-T) immunotherapy in the treatment of chronic lymphocytic leukemia (CLL)
.
The limitations of CAR-T therapy in CLL curative effect A number of CAR-T therapy related studies have been carried out in recent years, among which the field of hematological tumors has been explored most extensively
.
CAR-T therapy can achieve a higher clinical remission rate in hematological tumors, and CD19 CAR-T therapy also shows a certain effect in CLL
.
However, compared with acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL), the overall response rate and complete response rate of CAR-T therapy for CLL are relatively low
.
This difference in efficacy may be related to abnormal T cells in CLL patients
.
CAR-T therapy requires robust T cell expansion and implantation, and T cell damage caused by disease and treatment in CLL patients affects the expansion of T cells and the efficacy of CAR-T therapy to a certain extent
.
Ibrutinib can improve the efficacy of CAR-T therapy.
So what measures can improve the efficacy of CAR-T therapy? The status of endogenous T cells is related to the efficacy of CAR-T cells in the treatment of hematological malignancies
.
Many treatments for CLL including alkylating agents, fludarabine, and bendamustine can have a serious negative impact on T cell function and may aggravate T cell defects in CLL
.
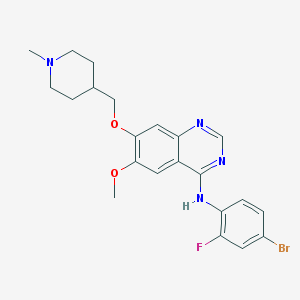
The world's first approved oral BTK inhibitor ibrutinib can not only avoid negative effects on T cells, but also may improve the function of anti-tumor T cells
.
Ibrutinib can inhibit BTK from affecting B cell signaling pathways, it can also inhibit ITK pathways, and regulate T cell differentiation and function
.
In recent years, many studies have proved that Ibrutinib can improve the expansion, implantation, and survival of CAR-T cells, thereby improving the efficacy of CAR-T therapy in CLL patients
.
An article published in the International Journal of Cancer this year evaluated the effect of ibrutinib on the production of CAR-T cells
.
The researchers collected peripheral blood mononuclear cells (PBMC) from 9 healthy donors and 8 CLL patients for CAR-T cell generation, and evaluated the expansion and phenotype of T cells and the function of CAR-T cells
.
The results of the study showed that Ibrutinib significantly improved the activity of CD3+ T cells from healthy donors
.
After the cells derived from CLL patients were cultured with ibrutinib, the CAR-T transduction rate was significantly increased on the 14th day (47% vs 59% without ibrutinib vs.
with ibrutinib, P = 0.
0142) , The absolute number of CAR-T cells on the 14th day also increased significantly (without ibrutinib: 4.
05×106 vs with ibrutinib: 7.
20×106; P=0.
0038)
.
In addition, the differentiation state of the infused CAR-T cells will also affect the proliferation capacity and curative effect in the body
.
Poorly differentiated CAR-T cells, especially naïve-like T cells (TN) and stem cell memory-like T cells (TSCM) have high implantation ability and have long-term persistence in the body
.
CLL patients have the characteristics of dysregulation of T cell developmental subpopulations, which are characterized by a significant decrease in TN cells in the early stage, and an increase in T cell counts in the late developmental stage
.
The results of this study show that in CAR-T cells derived from CLL patients, the addition of ibrutinib can increase the proportion and absolute count of TN cells in CD3+, CD3+/CD4+, and CD8+ T cells
.
In the xenograft mouse model of CLL, the addition of ibrutinib also improved the implantation and efficacy of CAR-T cells
.
In a study published in Blood in 2016, researchers evaluated the efficacy of ibrutinib combined with CD19 CAR-T cells (CTL019) in a mouse model vaccinated with the OSU-CLL cell line
.
The results of the study showed that receiving ibrutinib or CAR-T therapy alone did not affect overall survival, but the combination of ibrutinib and CAR-T regimen not only significantly enhanced the implantation of CAR-T cells in the peripheral blood, but also prolonged Survive
.
Clinical research progress A number of clinical studies exploring the combination of ibrutinib and CAR-T therapy are underway
.
A study reported by Professor Gill’s team at the 2018 ASH meeting included 19 adult CLL/small lymphocytic lymphoma (SLL) patients who had been treated with ibrutinib for at least 6 months without complete remission.
The enrolled patients received CAR-T cells were infused after 1 week of chemotherapy, and he was also treated with Ibrutinib
.
The results of the study showed that the complete remission rate of this program reached 43%, which was higher than the complete remission rate of 21%-29% in the previous study
.
The combination of Ibrutinib and CD19 CAR-T therapy for CLL significantly improved the remission rate and significantly reduced the incidence of grade 3-4 cytokine release syndrome (CRS)
.
In the same year, Professor Gauthier’s team reported a study that included patients with CLL who had progressed after ibrutinib treatment and received ibrutinib combined with CAR-T therapy.
Patients in the group were treated with CAR-T cells at least 2 weeks before leukocyte separation.
At least 3 months later, he received 420 mg/day of Ibrutinib at the same time
.
The results of the study show that compared with CAR-T alone, CAR-T therapy combined with ibrutinib can prevent tumor progression, improve CAR-T cell function, and achieve a higher disease remission rate (88% vs 56%).
At the same time, it can reduce the occurrence of CRS
.
In 2020, Professor Siddiqi’s team reported on CD19 CAR-T therapy Lisocabtagene maraluel (liso-cel) alone or combined with ibrutinib in the treatment of relapsed and refractory CLL/SLL
.
Patients in the combined treatment group in the study continued or restarted ibrutinib treatment at the time of enrollment, and continued to receive ibrutinib treatment for 90 days after liso-cel infusion (if clinical benefit, they can continue to receive ibrutinib treatment )
.
When Liso-cel was infused for a median of 30 days, the total remission rate of the combined treatment group and the single-agent treatment group were 95% and 68%, respectively, and the percentages of negative peripheral blood minimal residual disease (uMRD) were 89% and 75%, within 30 days The proportions of achieving uMRD are 100% and 60% respectively
.
The combination of Liso-cel and ibrutinib is beneficial to CAR-T cell expansion in patients with relapsed and refractory CLL/SLL who have previously received multiple lines of treatment, which can bring rapid disease remission, while improving remission rate and uMRD Proportion
.
At present, there are still many unresolved problems in the combination of ibrutinib and CAR-T therapy, such as the timing, dosage, and maintenance treatment time of the combined use of ibrutinib
.
However, the results of many clinical research data have confirmed that Ibrutinib combined with CAR-T therapy is expected to be a treatment option to further improve the efficacy of patients with B-cell malignancies
.
This is the end of today’s lymphoma micro-class, thank you! Professor Feng Ru, Professor, Chief Physician, Doctoral Supervisor, Department of Hematology, Nanfang Hospital, Southern Medical University, Guangzhou Member of the Oncology Committee and Chronic Lymphocyte Working Group Member of the Expert Committee of the Anti-Leukemia Alliance of the Chinese Society of Clinical Oncology Member of the Lymphoma Professional Committee of the Chinese Elderly Healthcare Association Chairman, Committee of Hematology and Immunology, Guangdong Society of Immunology, Chairman, Committee of Hematology and Oncology, Guangdong Anti-Cancer Association, Chairman, Committee of Lymphoma, Guangdong Anti-Cancer Association, Committee Member, Standing Committee of Hematology Branch, Guangdong Medical Association, Oncology, Guangdong Medical Association Deputy Leader of Lymphoma Group, Chinese Women Physicians Association Member of the Standing Committee of the Hematology Oncology Professional Committee of the Chinese Women Physicians Association Deputy Chairman of the Lymphoma Professional Committee of the Guangdong Provincial Association of Women Physicians How to use CRC numer: MED-ONC-CN-2387.
Approved date: 20210819.
References: 1.
Fuli Fan, et al.
Int J Cancer.
2021 Jan 15;148(2):419-428.
2.
Fraietta JA, et al.
Blood.
2016 Mar 3;127(9):1117-27.
3.
Blood.
2020 May 7;135(19):1611-1612.
4.
ASH 2018.
Abstract 299.
5.
Gill et al.
Blood.
2018;132 :298.
6.
2020ASH Abstract 544/546.
Stamp "read the original text", we make progress together
.
I am Dr.
Feng Ru from the Nanfang Hospital of Southern Medical University
.
What I share with you today is: Ibrutinib can improve the efficacy of chimeric antigen receptor T cell (CAR-T) immunotherapy in the treatment of chronic lymphocytic leukemia (CLL)
.
The limitations of CAR-T therapy in CLL curative effect A number of CAR-T therapy related studies have been carried out in recent years, among which the field of hematological tumors has been explored most extensively
.
CAR-T therapy can achieve a higher clinical remission rate in hematological tumors, and CD19 CAR-T therapy also shows a certain effect in CLL
.
However, compared with acute lymphoblastic leukemia (ALL) and diffuse large B-cell lymphoma (DLBCL), the overall response rate and complete response rate of CAR-T therapy for CLL are relatively low
.
This difference in efficacy may be related to abnormal T cells in CLL patients
.
CAR-T therapy requires robust T cell expansion and implantation, and T cell damage caused by disease and treatment in CLL patients affects the expansion of T cells and the efficacy of CAR-T therapy to a certain extent
.
Ibrutinib can improve the efficacy of CAR-T therapy.
So what measures can improve the efficacy of CAR-T therapy? The status of endogenous T cells is related to the efficacy of CAR-T cells in the treatment of hematological malignancies
.
Many treatments for CLL including alkylating agents, fludarabine, and bendamustine can have a serious negative impact on T cell function and may aggravate T cell defects in CLL
.
The world's first approved oral BTK inhibitor ibrutinib can not only avoid negative effects on T cells, but also may improve the function of anti-tumor T cells
.
Ibrutinib can inhibit BTK from affecting B cell signaling pathways, it can also inhibit ITK pathways, and regulate T cell differentiation and function
.
In recent years, many studies have proved that Ibrutinib can improve the expansion, implantation, and survival of CAR-T cells, thereby improving the efficacy of CAR-T therapy in CLL patients
.
An article published in the International Journal of Cancer this year evaluated the effect of ibrutinib on the production of CAR-T cells
.
The researchers collected peripheral blood mononuclear cells (PBMC) from 9 healthy donors and 8 CLL patients for CAR-T cell generation, and evaluated the expansion and phenotype of T cells and the function of CAR-T cells
.
The results of the study showed that Ibrutinib significantly improved the activity of CD3+ T cells from healthy donors
.
After the cells derived from CLL patients were cultured with ibrutinib, the CAR-T transduction rate was significantly increased on the 14th day (47% vs 59% without ibrutinib vs.
with ibrutinib, P = 0.
0142) , The absolute number of CAR-T cells on the 14th day also increased significantly (without ibrutinib: 4.
05×106 vs with ibrutinib: 7.
20×106; P=0.
0038)
.
In addition, the differentiation state of the infused CAR-T cells will also affect the proliferation capacity and curative effect in the body
.
Poorly differentiated CAR-T cells, especially naïve-like T cells (TN) and stem cell memory-like T cells (TSCM) have high implantation ability and have long-term persistence in the body
.
CLL patients have the characteristics of dysregulation of T cell developmental subpopulations, which are characterized by a significant decrease in TN cells in the early stage, and an increase in T cell counts in the late developmental stage
.
The results of this study show that in CAR-T cells derived from CLL patients, the addition of ibrutinib can increase the proportion and absolute count of TN cells in CD3+, CD3+/CD4+, and CD8+ T cells
.
In the xenograft mouse model of CLL, the addition of ibrutinib also improved the implantation and efficacy of CAR-T cells
.
In a study published in Blood in 2016, researchers evaluated the efficacy of ibrutinib combined with CD19 CAR-T cells (CTL019) in a mouse model vaccinated with the OSU-CLL cell line
.
The results of the study showed that receiving ibrutinib or CAR-T therapy alone did not affect overall survival, but the combination of ibrutinib and CAR-T regimen not only significantly enhanced the implantation of CAR-T cells in the peripheral blood, but also prolonged Survive
.
Clinical research progress A number of clinical studies exploring the combination of ibrutinib and CAR-T therapy are underway
.
A study reported by Professor Gill’s team at the 2018 ASH meeting included 19 adult CLL/small lymphocytic lymphoma (SLL) patients who had been treated with ibrutinib for at least 6 months without complete remission.
The enrolled patients received CAR-T cells were infused after 1 week of chemotherapy, and he was also treated with Ibrutinib
.
The results of the study showed that the complete remission rate of this program reached 43%, which was higher than the complete remission rate of 21%-29% in the previous study
.
The combination of Ibrutinib and CD19 CAR-T therapy for CLL significantly improved the remission rate and significantly reduced the incidence of grade 3-4 cytokine release syndrome (CRS)
.
In the same year, Professor Gauthier’s team reported a study that included patients with CLL who had progressed after ibrutinib treatment and received ibrutinib combined with CAR-T therapy.
Patients in the group were treated with CAR-T cells at least 2 weeks before leukocyte separation.
At least 3 months later, he received 420 mg/day of Ibrutinib at the same time
.
The results of the study show that compared with CAR-T alone, CAR-T therapy combined with ibrutinib can prevent tumor progression, improve CAR-T cell function, and achieve a higher disease remission rate (88% vs 56%).
At the same time, it can reduce the occurrence of CRS
.
In 2020, Professor Siddiqi’s team reported on CD19 CAR-T therapy Lisocabtagene maraluel (liso-cel) alone or combined with ibrutinib in the treatment of relapsed and refractory CLL/SLL
.
Patients in the combined treatment group in the study continued or restarted ibrutinib treatment at the time of enrollment, and continued to receive ibrutinib treatment for 90 days after liso-cel infusion (if clinical benefit, they can continue to receive ibrutinib treatment )
.
When Liso-cel was infused for a median of 30 days, the total remission rate of the combined treatment group and the single-agent treatment group were 95% and 68%, respectively, and the percentages of negative peripheral blood minimal residual disease (uMRD) were 89% and 75%, within 30 days The proportions of achieving uMRD are 100% and 60% respectively
.
The combination of Liso-cel and ibrutinib is beneficial to CAR-T cell expansion in patients with relapsed and refractory CLL/SLL who have previously received multiple lines of treatment, which can bring rapid disease remission, while improving remission rate and uMRD Proportion
.
At present, there are still many unresolved problems in the combination of ibrutinib and CAR-T therapy, such as the timing, dosage, and maintenance treatment time of the combined use of ibrutinib
.
However, the results of many clinical research data have confirmed that Ibrutinib combined with CAR-T therapy is expected to be a treatment option to further improve the efficacy of patients with B-cell malignancies
.
This is the end of today’s lymphoma micro-class, thank you! Professor Feng Ru, Professor, Chief Physician, Doctoral Supervisor, Department of Hematology, Nanfang Hospital, Southern Medical University, Guangzhou Member of the Oncology Committee and Chronic Lymphocyte Working Group Member of the Expert Committee of the Anti-Leukemia Alliance of the Chinese Society of Clinical Oncology Member of the Lymphoma Professional Committee of the Chinese Elderly Healthcare Association Chairman, Committee of Hematology and Immunology, Guangdong Society of Immunology, Chairman, Committee of Hematology and Oncology, Guangdong Anti-Cancer Association, Chairman, Committee of Lymphoma, Guangdong Anti-Cancer Association, Committee Member, Standing Committee of Hematology Branch, Guangdong Medical Association, Oncology, Guangdong Medical Association Deputy Leader of Lymphoma Group, Chinese Women Physicians Association Member of the Standing Committee of the Hematology Oncology Professional Committee of the Chinese Women Physicians Association Deputy Chairman of the Lymphoma Professional Committee of the Guangdong Provincial Association of Women Physicians How to use CRC numer: MED-ONC-CN-2387.
Approved date: 20210819.
References: 1.
Fuli Fan, et al.
Int J Cancer.
2021 Jan 15;148(2):419-428.
2.
Fraietta JA, et al.
Blood.
2016 Mar 3;127(9):1117-27.
3.
Blood.
2020 May 7;135(19):1611-1612.
4.
ASH 2018.
Abstract 299.
5.
Gill et al.
Blood.
2018;132 :298.
6.
2020ASH Abstract 544/546.
Stamp "read the original text", we make progress together