-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
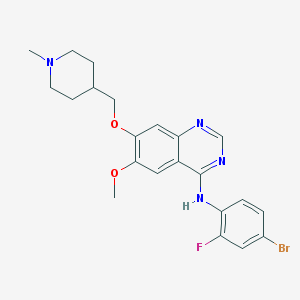
The solution of tumor virus that replicates, selectively infects tumor cells within tumor cells and then kills tumor cells is one of the most promising cancer immunotherapy methods.
tumor virus therapy uses genetic engineering to modify the tumor virus, make it lose its toxicity and retain the virus's ability to replicate, and deliver it to tumor cells, kill tumor cells, and achieve the purpose of treatment.
when cancer cells break and die under the virus infection, newly generated virus particles are released, further infecting the surrounding cancer cells.
mechanism, it can not only directly kill the tumor, but also hope to stimulate the body's immune response, enhance the anti-tumor effect.
in order to make the tumor virus effectively target cancer cells, the specific target of tumor is a major focus in research and development.
interesting, tumors are inherently well suited to be targeted by tumor viruses - when genes such as RAS, TP53, RB1, and PTEN mutate, the cancer cells' ability to fight hiv becomes weaker, giving the tumor virus a chance.
the viruses commonly used at present include adenovirus, pox virus, herpes virus, exovirus, small virus, Newtown disease virus, Kosachi virus and so on.
modified viruses such as the vesicular virus (vesium stomatitis virus, VSV) and the Maraba virus (Maraba virus) can specifically target cancer cells by relying on defects in interferon signaling pathways.
the first tumor virus to be approved by the U.S. FDA for the treatment of melanoma, it was modified by herpes simplex virus type 1, HSV-1.
these viruses are designed to be related to immune responses.
other tumor viruses can be additionally targeted at metabolic abnormalities of malignant tumors.
, for example, pexastimogene devacirepvec (Pexa-Vec) itself has a defective thoracic kinase gene, so it can only be replicated in cancer cells with excess thoratoside kinase activity.
, the B18R gene in the virus has an early termination cryptoon, making its encoded protein less susceptible to interferon identification and binding.
these properties allow these viruses to target tumor cells effectively, with minimal impact on normal cells.
China is one of the early countries to study tumor virus, as early as 2003 and 2005, the CFDA approved two tumor virus products on the market, respectively, Sebeno's life and three-dimensional organisms of Ankeri (H101).
but these two products have not yet been internationally recognized.
only one Amgen company's T-vec (Imlygic, type I herpes simplex virus) is currently FDA-approved for local treatment in melanoma patients and is the first FDA-approved solution to the virus.
, solubility viruses and immune T cells have to go through four key steps if they want to trigger a successful anti-tumor response.
and the tumor virus can assist T cells in these four steps.
1. T cell sensitization (T cell priming) T-cell reaction starts without the identification of specific antigen epithemis, and this complex process cannot be separated from the work of antigen presentation cells.
in cancer, the process of antigen presentation is often negatively affected, leaving the tumor immune "cold."
and tumor viruses can perform a similar role as "vaccines" to promote the presentation and identification of tumor-related antigens.
as mentioned above, local lysoma virus treatment can be done by lysicing cancer cells, releasing a large number of tumor-related antigens, and creating a pro-immune cytokine environment, which facilitates the implementation of antigen synopsis cells to achieve their function.
this idea has been validated in many experiments.
some researchers have found that the chimeric of poliovirus (poliovirus) and the impeachment virus can lead to the release of tumor antigens and lead to a class I interferon response.
these stimuli eventually induce tumor-specific T-cell population growth.
the advantage of this approach, the researchers point out, is that we don't need to know in advance about tumor-related antigens, so it's a simple way to develop individually personalized vaccines.
but we should also note that such methods may not induce enough T-cell reactions.
, the researchers believe that adding tumor-related virus vectors to the tumor virus may improve the effectiveness.
multiple mechanisms of action of the tumor virus 2. The T cells in the circulation of movement and immersion (trafficking and resional) can move to the tumor site for immersion, which plays an important role in the patient's prognosis.
and the use of the tumor virus is expected to enhance the leaching of T cells to tumors. there are a number of potential mechanisms behind this
.
first, viral infections stimulate potential Class I interferon reactions and stimulate the generation of chemofactors, thereby collecting T-cells.
in animal models, whether it's adenovirus, HSV-1, bovine pox virus, or Newcastle virus, can effectively improve the leaching of T cells.
in addition, the solute virus has been shown in clinical trials to improve the leaching of T-cells in melanoma and other advanced cancers.
scientists have also observed positive results in some studies of brain tumors.
, the tumor virus can induce the reaction of TNF, IL-1 beta, and supplements, increase the expression of selectors on endothelial cells, and provide key signals for the leaching of T cells.
third, the tumor virus is modified to target specific cancer-causing signaling pathways.
for example, the WNT-beta-catenin pathway has an immunosuppressive effect and inhibits the antiviral response of cells.
through the transformation, many tumor viruses can be activated by the beta-catenin signaling pathway, promoting tumor-specific virus replication and anti-tumor effect.
fourth, the tumor virus can encode T-cell chemators and is expected to recruit T cells directly without worrying about the expression defects of chemators in the tumor environment.
in the review, the researchers also point out that tumor viruses can also help overcome organizational barriers and further help T-cell immersion.
, for example, it attracts neutrophils to release inflammatory media (inflammatory mediators) in tumor microenvironments, as well as proteases with cytotoxicity and extracellular matrix (ECM) degradation properties.
3. Avoiding immunosuppressa does not mean that T cells are effective in attacking tumors even if they successfully immerse them in the tumor.
the researchers point out that t-cells still need to overcome immune-suppressing molecules such as IL-10, TGF beta, and IDO in the environment after entering the tumor.
in this regard, the tumor virus is expected to induce pro-inflammatory auxiliary T-cell 1 (pro-rhywy T helper 1), thus altering the inhibitory tumor microenvironment.
, it is also expected to kill immunosuppressive cells directly.
, perhaps the most interesting thing about the tumor virus is the ability to turn "cold tumors" into "hot tumors".
in one study, researchers first removed tumors from patients with triple-negative breast cancer and implanted in situ.
follow-up findings show that the use of the tumor virus causes T-cells to react to tumor antigens and prevents tumor recurrence.
and the use of immunocheckpoint inhibitors can further enhance the effectiveness of treatment.
other preclinical trials have also demonstrated the potential of the solution virus to be used with immunocheckpoint inhibitors.
in clinical trials, this potential has been proven again.
both PD-1 inhibitors and CTLA4 inhibitors, in combination with talimogene laherparepvec, can increase the number of CD8 and CD4-positive T cells in patients, indicating that there may be systemic immune effects.
although the trial is still in phase 1, the overall rate of remission against advanced melanoma was 62% and the total remission rate was 33%.
, patients with low immunocellular immersion also achieved good results, indicating that "cold tumors" also responded to immunocheckpoint inhibitors under the action of the tumor virus.
study published in Cell has also attracted a lot of attention.
in addition to making tumors "hot" from "cold", some existing studies are also trying to deliver immunocheckpoint inhibitors with the solute virus.
this practice requires the coding of immunocheckpoint inhibitors in the tumor virus to avoid the toxicity of combination therapies.
, the tumor virus is specific to cancer cells and can be more targeted at releasing drugs in the right place.
currently, two studies have been initially attempted.
But we would also like to admit that there are still many technical and institutional challenges to be solved.
. The final step in successful immunotherapy in combination with tumor cells is the identification, binding, and attack of tumor cells by T cells.
in order to avoid the recognition of T cells, tumor cells can lower the pathways involved in antigen presentation and Class I MHC.
and the tumor virus is expected to reverse it to some extent.
, for example, the reovirus (reovirus) increases the expression of Class I MHC and/or Class II MHC on tumor cells and antigen-presenting cells.
similar, HSV-infected tumor cells promote the maturation of dendritic cells and the expression of Class II MHC.
researchers also point out that the tumor virus is expected to use a new approach to promote the binding of T-cells to tumor cells.
currently, a class of molecules called bispecific T-cell ers (Bispecific T cell, BiTE) binds to molecules that activate T cells such as CD3 and with antigen targets on the surface of cancer cells.
these innovative treatments have yielded positive results in the treatment of blood cancers, but their application in solid tumors may be limited by tumor microenvironments and/or off-target side effects.
the tumor virus that encodes BiTE is expected to solve these bottlenecks.
in an early study, a BiTE that binds directly to EPHA2 and CD3 was integrated into the tumor virus and released biTE at tumor cells, killing cancer cells that were not infected with the virus.
another study, BiTE, combined with EpCAM and CD3, also activated T cells in tissue biopsy samples.
intracanceriasic inquisitive lysises that encode IL-7 and IL-12 can increase the immune status of anti-tumor efficacy of immunology inhibitors in the micro-environment of anti-tumor tumors, which is a key indicator to determine the effectiveness of immunotherapy antitumor.
data have been available to support the role of tumor-immersed lymphocyte (TIL) activation and proliferation in improving the therapeutic benefits of immunotherapy for patients with solid tumors. In a new study
, in a new study to further improve the anti-cancer potential of the tumor virus, researchers from Japan's Bird's University and Astellas Pharmaceuticals Inc. genetically modified the tumor-soluble bovine pox virus to deliver two cytokines --- IL-7 and IL-12 to help stimulate the anti-tumor immune response.
related findings were published on January 15, 2020 in the journal Science Translational Medicine, with the title "Intratumoral expression of IL-7 and IL-12 using an oncolytic virus virus es systemic sapery to immune checkpoint checkpoint".
the paper's author, Shinsuke Nakao of Astellas Pharmaceuticals.
images from Science Translational Medicine, 2020, doi: 10.1126/scitranslmed.aax7992.
Nakao and his team found that injecting the tumor-selective tumor tumor tumor il-7 and IL-12-coded tumor-selective tumor bovinepox virus (oncolyticvaccinina virus) into an immune-active tumor-activated tumor with previously immune progenitors even caused the tumor to subside completely, even for tumors that accumulate in the distance.
mice that achieved complete tumor regeneration developed resistance when they were attacked again by the same tumor cells, suggesting that they established long-term tumor-specific immune memory.
in a non-reactive tumor model of immunocheckpoint inhibitor sepsis anti-PD-1 or anti-CTLA4 antibody monodrug, the combination of this viral therapy with anti-PD-1 anti-or CTLA4 antibodies in combination with this virus therapy can further improve anti-tumor activity compared to the use of only this viral therapy.
these findings show that intratumor injections carry genes code IL-7 and IL-12 are anti-tumor activity in tumors that are directly injected with the tumor of the tumor bovinepox virus and in tumors that do not inject this solution bovinepox virus, thus making tumors sensitive to immunoosepoint inhibitors.
The Nakao team also observed the benefits of intratumor IL-7 and IL-12 expression in human-derived mice that carry human cancer cells.
these data support further research in patients with non-inflammatory solid tumors.
.