-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Author: This article is the author's permission Chunlan Qiugui NMT Medical publish, please do not reprint without authorization.
Approximately 20% of patients with diffuse large B-cell lymphoma (DLBCL) are refractory to first-line standard treatment (ie treatment is ineffective or relapse within 6 months after treatment), and 20%-25% of patients will be remission with first-line standard treatment Early relapse (relapse within 2 years after treatment), some patients will relapse late after standard first-line treatment (relapse 2 years after treatment).
First-line treatment fails, especially for patients with primary refractory and early relapse DLBCL, the overall prognosis is poor and the survival time is short; while the long-term relapse DLBCL patients have a relatively good prognosis.
This article aims to summarize the treatment progress of patients with relapsed or refractory diffuse large B-cell lymphoma (R/R DLBCL) in recent years for your reference.
R/R DLBCL patients need clear information before starting treatment.
DLBCL first-line treatment has failed.
Before starting subsequent treatment, it is necessary to clarify the following key information: whether the patient is primary refractory, early recurrence or long-term recurrence.
Relapsed or refractory patients undergo pathological biopsy again to confirm the pathological type, and patients with late relapse may have recurrence of indolent lymphoma.
The whole body imaging examination was re-staging.
The occurrence of adverse events in the patient’s previous treatment.
The patient's physical status, important organ functions, etc.
, assess whether the patient is suitable for hematopoietic stem cell transplantation (HCT).
Recent treatment of R/R DLBCL patients suitable for HCT.
High-dose chemotherapy and autologous hematopoietic stem cell transplantation (Auto-HCT) provide a chance of cure for R/R DLBCL patients who are sensitive to chemotherapy.
However, due to the patient's advanced age and the presence of comorbidities, usually only 50% of R/R DLBCL patients are suitable for HCT treatment.
The results of previous clinical studies have shown [1-2] that it is suitable for autologous transplantation of R/R DLBCL patients with commonly used rescue treatment options containing platinum-based chemotherapeutics, such as R-DHAP (rituximab combined with dexamethasone, high-dose arabinocytes) Glycoside and Cisplatin), R-ICE (Rituximab combined with Ifosfamide, Carboplatin and Etoposide), and R-GDP (Rituximab combined with Gemcitabine, Dexamethasone and Cisplatin).
These rescue treatments have similar effects, with approximately 50% of patients achieving complete remission (CR) and receiving transplants.
Therefore, clinicians can choose a rescue treatment plan suitable for patients with R/R DLBCL according to the patient's adverse reactions and organ functions in the previous treatment.
After receiving Auto-HCT treatment, the overall cure rate of R/R DLBCL patients who have obtained CR through second-line rescue treatment is 25%-35% [1-2].
In addition, allogeneic hematopoietic stem cell transplantation (Allo-HCT) can also cure R/R DLBCL patients, but the higher transplant-related mortality usually offsets the advantages of its transplant anti-tumor effect, so it is only suitable for a small number of patients.
Strictly screened patients.
Not suitable for the treatment of HCT R/R DLBCL patients Recent developments R/R DLBCL patients who are not suitable for HCT account for about 50%, mainly including: advanced age, poor health, comorbidities, poor response to salvage therapy, and recurrence after HCT Of patients.
The vast majority of patients with R/R DLBCL will eventually develop into this category as the course of the disease progresses.
Such patients usually choose palliative treatment, including sequential single-agent chemotherapy, and multi-drug treatment options with acceptable adverse reactions.
In recent years, new targeted drugs and new treatments have emerged in an endless stream.
These new drugs and new therapies may have the potential to control the disease for a long time, can bring obvious survival benefits, and bring new ideas to R/R DLBCL patients who are not suitable for HCT.
Hope.
Efficacy of CAR-T cell therapy in R/R DLBCL patients Chimeric antigen receptor (CAR)-T cell therapy is a genetically modified cell therapy that provides new opportunities for R/R DLBCL patients who have undergone multiple treatments in the past.
Hope. The first batch of autologous CAR-T cells that have been approved for R/R DLBCL are CD19-targeting autologous CAR-T cells.
The results of several key clinical studies on patients with relapsed or refractory aggressive B-cell non-Hodgkin’s lymphoma (B-NHL) show that [3-5], CAR-T cell products targeting CD19 (such as Axicabtagene Ciloleucel) , Tisagenlecleucel and Lisocabtagene Maraleucel) have an overall effective rate (ORR) of 52%-82%, and a CR rate of 40%-54%.
Among them, the latest follow-up results of a key clinical study of Axicabtagene Ciloleucel in the treatment of relapsed or refractory aggressive B-NHL [6] showed that after a median follow-up of 27 months, 37% of patients still had persistent CR.
At present, these CAR-T cell products have been approved for the treatment of R/R DLBCL that has previously received ≥2 line therapy.
Whether CAR-T cell therapy can replace Auto-HCT in R/R DLBCL is still inconclusive.
In addition, the special mechanism of CAR-T cell therapy also brings unique adverse reactions, so it may not be suitable for all R/R DLBCL patients.
Previous research reports [3-5] showed that the incidence of grade 3-4 cytokine release syndrome in R/R DLBCL patients with CAR-T cell therapy was 2-22%; the incidence of neurotoxicity was 10-28 %.
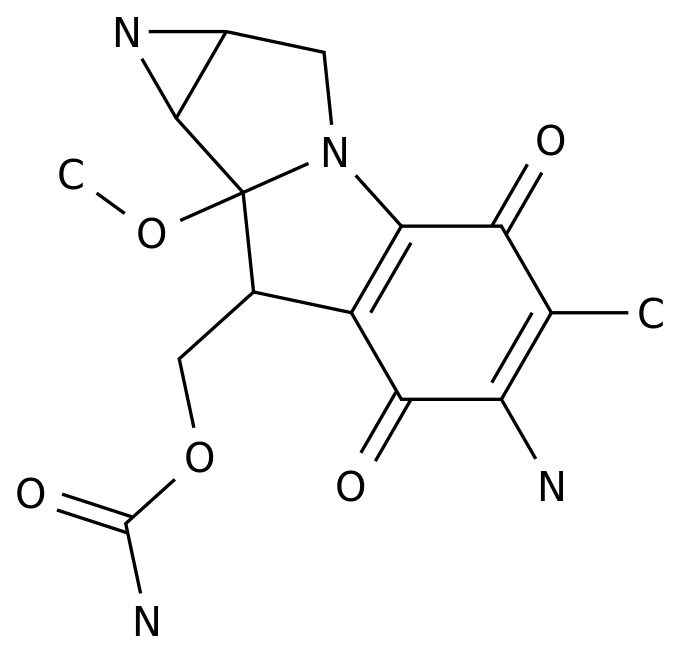
The efficacy of other new drug therapies in patients with R/R DLBCL Polatuzumab Vedotin (Pola) is an antibody-drug conjugate (ADC) that targets CD79b.
ADC has become one of the hottest research in the field of tumor precision therapy.
This kind of drugs couples target-specific monoclonal antibodies with high-killing cytotoxic drugs through specific connectors.
Molecular cytotoxic drugs are efficiently transported to target tumor cells in a targeted manner. A randomized phase II clinical study [7] evaluated Pola combined with bendamustine and rituximab vs bendamustine and rituximab (BR) in R/R DLBCL patients who are not suitable for HCT The efficacy in.
The results showed that Pola combined with bendamustine and rituximab significantly improved the patient's complete metabolic remission (CMR) rate, progression-free survival rate and overall survival rate.
Therefore, the combination of Pola combined with bendamustine and rituximab has been approved for R/R DLBCL patients who are not suitable for HCT.
Selinexor is a selective inhibitor of the nuclear export protein XPO1.
Based on the results of a phase II clinical study [8], the drug has been approved as a single agent for R/R DLBCL patients who have previously received ≥2 line therapy.
Immune checkpoint inhibitors, anti-PD-1 antibodies did not show clinical benefit in R/R DLBCL patients.
Magrolimab is a macrophage immune checkpoint inhibitor.
Early studies have shown that it has a synergistic effect with rituximab [9] and is expected to become a new treatment for patients with R/R DLBCL.
Bispecific antibodies target tumor cells and antigens on T cells to induce T cell activation and produce cell-mediated cytotoxicity.
Belintoux is a bispecific antibody targeting CD19 and CD3.
It is active in R/R DLBCL, but its development is hindered by related neurotoxicity and other aspects.
In addition, bispecific antibodies targeting CD3 and CD20 are currently under development, and early studies have shown preliminary efficacy.
Other new drugs also include drugs targeting the apoptosis pathway (Bcl-2 inhibitor Venecla), drugs targeting the B cell receptor pathway (BTK inhibitor Ibrutinib), and targeting epigenetic regulatory factors Drugs (EZH2 inhibitor Tazemetostat).
However, these new drugs have limited efficacy in R/R DLBCL patients, and it is not clear whether combined therapy can improve the efficacy [10].
Reference 1.
Crump M, Kuruvilla J, Couban S, etal.
Randomized comparison of gemcitabine, dexamethasone, and cisplatin versusdexamethasone, cytarabine, and cisplatin chemotherapy before autologousstem-cell transplantation for relapsed and refractory aggressive lymphomas:NCIC-CTG LY.
12.
J Clin Oncol 2014;32:3490-6.
2.
Gisselbrecht C, Glass B, Mounier N,etal.
Salvage regimens with autologous transplantation for relapsed large B-celllymphoma in the rituximab era.
J Clin Oncol 2010;28:4184-90.
3.
Abramson JS, Palomba ML, Gordon LI, etal.
Lisocabtagene maraleucel for patients with relapsed or refractorylarge B-cell lymphomas (TRANSCEND NHL001): a multicentre seamless designstudy.
Lancet 2020;396:839-52.
4.
Neelapu SS, Locke FL, Bartlett NL, etal .
Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-CellLymphoma.
N Engl J Med 2017;377:2531-44.
5.
Schuster SJ,Bishop MR, Tam CS, et al.
Tisagenlecleucel in adult relapsed or refractory diffuse large B-celllymphoma.
N Engl J Med 2019;380:45-566.
Locke FL, Ghobadi A, Jacobson CA, etal.
Long-term safety and activity of axicabtagene ciloleucel in refractorylarge B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1-2 trial.
Lancet Oncol 2019;20:31-42.
7.
Sehn LH, Herrera AF, Flowers CR,et al.
Polatuzumab vedotin in relapsed or refractory diffuse large B-cell lymphoma.
JClin Oncol 2020;38:155-65.
8.
Kalakonda N, Maerevoet M, Cavallo F,etal.
Selinexor in patients with relapsed or refractory diffuse large B-celllymphoma (SADAL): a single-arm, multinational, multicentre, open-label, phase 2trial.
Lancet Haematol 2020;7(7):e511-e522.
9.
Advani R, Flinn I, Popplewell L, etal.
CD47 blockade by Hu5F9-G4 and rituximab in non-Hodgkin's lymphoma.
N Engl JMed 2018;379:1711-21.
10.
Laurie H.
Sehn, and Gilles Salles.
DiffuseLarge B-Cell Lymphoma.
N Engl J Med 2021;384:842-58.
Stamp "read the original text", we make progress together
Approximately 20% of patients with diffuse large B-cell lymphoma (DLBCL) are refractory to first-line standard treatment (ie treatment is ineffective or relapse within 6 months after treatment), and 20%-25% of patients will be remission with first-line standard treatment Early relapse (relapse within 2 years after treatment), some patients will relapse late after standard first-line treatment (relapse 2 years after treatment).
First-line treatment fails, especially for patients with primary refractory and early relapse DLBCL, the overall prognosis is poor and the survival time is short; while the long-term relapse DLBCL patients have a relatively good prognosis.
This article aims to summarize the treatment progress of patients with relapsed or refractory diffuse large B-cell lymphoma (R/R DLBCL) in recent years for your reference.
R/R DLBCL patients need clear information before starting treatment.
DLBCL first-line treatment has failed.
Before starting subsequent treatment, it is necessary to clarify the following key information: whether the patient is primary refractory, early recurrence or long-term recurrence.
Relapsed or refractory patients undergo pathological biopsy again to confirm the pathological type, and patients with late relapse may have recurrence of indolent lymphoma.
The whole body imaging examination was re-staging.
The occurrence of adverse events in the patient’s previous treatment.
The patient's physical status, important organ functions, etc.
, assess whether the patient is suitable for hematopoietic stem cell transplantation (HCT).
Recent treatment of R/R DLBCL patients suitable for HCT.
High-dose chemotherapy and autologous hematopoietic stem cell transplantation (Auto-HCT) provide a chance of cure for R/R DLBCL patients who are sensitive to chemotherapy.
However, due to the patient's advanced age and the presence of comorbidities, usually only 50% of R/R DLBCL patients are suitable for HCT treatment.
The results of previous clinical studies have shown [1-2] that it is suitable for autologous transplantation of R/R DLBCL patients with commonly used rescue treatment options containing platinum-based chemotherapeutics, such as R-DHAP (rituximab combined with dexamethasone, high-dose arabinocytes) Glycoside and Cisplatin), R-ICE (Rituximab combined with Ifosfamide, Carboplatin and Etoposide), and R-GDP (Rituximab combined with Gemcitabine, Dexamethasone and Cisplatin).
These rescue treatments have similar effects, with approximately 50% of patients achieving complete remission (CR) and receiving transplants.
Therefore, clinicians can choose a rescue treatment plan suitable for patients with R/R DLBCL according to the patient's adverse reactions and organ functions in the previous treatment.
After receiving Auto-HCT treatment, the overall cure rate of R/R DLBCL patients who have obtained CR through second-line rescue treatment is 25%-35% [1-2].
In addition, allogeneic hematopoietic stem cell transplantation (Allo-HCT) can also cure R/R DLBCL patients, but the higher transplant-related mortality usually offsets the advantages of its transplant anti-tumor effect, so it is only suitable for a small number of patients.
Strictly screened patients.
Not suitable for the treatment of HCT R/R DLBCL patients Recent developments R/R DLBCL patients who are not suitable for HCT account for about 50%, mainly including: advanced age, poor health, comorbidities, poor response to salvage therapy, and recurrence after HCT Of patients.
The vast majority of patients with R/R DLBCL will eventually develop into this category as the course of the disease progresses.
Such patients usually choose palliative treatment, including sequential single-agent chemotherapy, and multi-drug treatment options with acceptable adverse reactions.
In recent years, new targeted drugs and new treatments have emerged in an endless stream.
These new drugs and new therapies may have the potential to control the disease for a long time, can bring obvious survival benefits, and bring new ideas to R/R DLBCL patients who are not suitable for HCT.
Hope.
Efficacy of CAR-T cell therapy in R/R DLBCL patients Chimeric antigen receptor (CAR)-T cell therapy is a genetically modified cell therapy that provides new opportunities for R/R DLBCL patients who have undergone multiple treatments in the past.
Hope. The first batch of autologous CAR-T cells that have been approved for R/R DLBCL are CD19-targeting autologous CAR-T cells.
The results of several key clinical studies on patients with relapsed or refractory aggressive B-cell non-Hodgkin’s lymphoma (B-NHL) show that [3-5], CAR-T cell products targeting CD19 (such as Axicabtagene Ciloleucel) , Tisagenlecleucel and Lisocabtagene Maraleucel) have an overall effective rate (ORR) of 52%-82%, and a CR rate of 40%-54%.
Among them, the latest follow-up results of a key clinical study of Axicabtagene Ciloleucel in the treatment of relapsed or refractory aggressive B-NHL [6] showed that after a median follow-up of 27 months, 37% of patients still had persistent CR.
At present, these CAR-T cell products have been approved for the treatment of R/R DLBCL that has previously received ≥2 line therapy.
Whether CAR-T cell therapy can replace Auto-HCT in R/R DLBCL is still inconclusive.
In addition, the special mechanism of CAR-T cell therapy also brings unique adverse reactions, so it may not be suitable for all R/R DLBCL patients.
Previous research reports [3-5] showed that the incidence of grade 3-4 cytokine release syndrome in R/R DLBCL patients with CAR-T cell therapy was 2-22%; the incidence of neurotoxicity was 10-28 %.
The efficacy of other new drug therapies in patients with R/R DLBCL Polatuzumab Vedotin (Pola) is an antibody-drug conjugate (ADC) that targets CD79b.
ADC has become one of the hottest research in the field of tumor precision therapy.
This kind of drugs couples target-specific monoclonal antibodies with high-killing cytotoxic drugs through specific connectors.
Molecular cytotoxic drugs are efficiently transported to target tumor cells in a targeted manner. A randomized phase II clinical study [7] evaluated Pola combined with bendamustine and rituximab vs bendamustine and rituximab (BR) in R/R DLBCL patients who are not suitable for HCT The efficacy in.
The results showed that Pola combined with bendamustine and rituximab significantly improved the patient's complete metabolic remission (CMR) rate, progression-free survival rate and overall survival rate.
Therefore, the combination of Pola combined with bendamustine and rituximab has been approved for R/R DLBCL patients who are not suitable for HCT.
Selinexor is a selective inhibitor of the nuclear export protein XPO1.
Based on the results of a phase II clinical study [8], the drug has been approved as a single agent for R/R DLBCL patients who have previously received ≥2 line therapy.
Immune checkpoint inhibitors, anti-PD-1 antibodies did not show clinical benefit in R/R DLBCL patients.
Magrolimab is a macrophage immune checkpoint inhibitor.
Early studies have shown that it has a synergistic effect with rituximab [9] and is expected to become a new treatment for patients with R/R DLBCL.
Bispecific antibodies target tumor cells and antigens on T cells to induce T cell activation and produce cell-mediated cytotoxicity.
Belintoux is a bispecific antibody targeting CD19 and CD3.
It is active in R/R DLBCL, but its development is hindered by related neurotoxicity and other aspects.
In addition, bispecific antibodies targeting CD3 and CD20 are currently under development, and early studies have shown preliminary efficacy.
Other new drugs also include drugs targeting the apoptosis pathway (Bcl-2 inhibitor Venecla), drugs targeting the B cell receptor pathway (BTK inhibitor Ibrutinib), and targeting epigenetic regulatory factors Drugs (EZH2 inhibitor Tazemetostat).
However, these new drugs have limited efficacy in R/R DLBCL patients, and it is not clear whether combined therapy can improve the efficacy [10].
Reference 1.
Crump M, Kuruvilla J, Couban S, etal.
Randomized comparison of gemcitabine, dexamethasone, and cisplatin versusdexamethasone, cytarabine, and cisplatin chemotherapy before autologousstem-cell transplantation for relapsed and refractory aggressive lymphomas:NCIC-CTG LY.
12.
J Clin Oncol 2014;32:3490-6.
2.
Gisselbrecht C, Glass B, Mounier N,etal.
Salvage regimens with autologous transplantation for relapsed large B-celllymphoma in the rituximab era.
J Clin Oncol 2010;28:4184-90.
3.
Abramson JS, Palomba ML, Gordon LI, etal.
Lisocabtagene maraleucel for patients with relapsed or refractorylarge B-cell lymphomas (TRANSCEND NHL001): a multicentre seamless designstudy.
Lancet 2020;396:839-52.
4.
Neelapu SS, Locke FL, Bartlett NL, etal .
Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-CellLymphoma.
N Engl J Med 2017;377:2531-44.
5.
Schuster SJ,Bishop MR, Tam CS, et al.
Tisagenlecleucel in adult relapsed or refractory diffuse large B-celllymphoma.
N Engl J Med 2019;380:45-566.
Locke FL, Ghobadi A, Jacobson CA, etal.
Long-term safety and activity of axicabtagene ciloleucel in refractorylarge B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1-2 trial.
Lancet Oncol 2019;20:31-42.
7.
Sehn LH, Herrera AF, Flowers CR,et al.
Polatuzumab vedotin in relapsed or refractory diffuse large B-cell lymphoma.
JClin Oncol 2020;38:155-65.
8.
Kalakonda N, Maerevoet M, Cavallo F,etal.
Selinexor in patients with relapsed or refractory diffuse large B-celllymphoma (SADAL): a single-arm, multinational, multicentre, open-label, phase 2trial.
Lancet Haematol 2020;7(7):e511-e522.
9.
Advani R, Flinn I, Popplewell L, etal.
CD47 blockade by Hu5F9-G4 and rituximab in non-Hodgkin's lymphoma.
N Engl JMed 2018;379:1711-21.
10.
Laurie H.
Sehn, and Gilles Salles.
DiffuseLarge B-Cell Lymphoma.
N Engl J Med 2021;384:842-58.
Stamp "read the original text", we make progress together