-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
The U.S. health care market has undergone tremendous changes since the adoption of the Affordable Care Act (ACA), which has not only had a huge impact on large hospitals, but has also put unprecedented pressure on large communities and rural hospitals. The hospital market has also seen a huge wave of mergers and acquisitions since the 1980s. A large number of small medical institutions have closed down or been merged, for-profit hospital mergers are becoming more serious in the south and rural areas, and non-profit hospital acquisitions or collaborations with small hospitals have become a trend in the north and in small towns.
pressure on U.S. hospitals comes mainly from changes in the payer's. Driven by the ACA, value care has become a major payout, especially with re-entry rates within 30 days under pressure from all hospitals. Hospitals have had to promote out-of-hospital medical services to meet the 30-day re-entry rate, but this has also meant a decline in patient inflows and a decline in revenue growth. If you broaden your horizons to the past 20-30 years, the development of patient services from in-hospital to out-of-hospital is a long-term trend, such as the previous 3-5 days of hospitalization required to open hernia, but now discharged on the same day. This has also reduced the proportion of inpatient revenue in primary hospitals from more than 90 per cent in the 1990s to less than a third, and grass-roots income is increasingly dependent on outpatient and other non-inpatient operations.
but that's just one aspect, and the other problem that has to be faced is the expansion of government health care, especially Medicaid. In the early days of Medicaid's expansion, hospitals of all kinds experienced some growth in revenue and operating profit, largely because Medicaid helped low-paying users gain access to health services and reduce bad debts caused by inability to pay. According to The Urban Institute's 2017 report, Medicaid's expansion generated an average of $5 million in revenue per hospital, reduced unresoled medical expenses by $3.2 million and boosted operating profit by 2.5 points. That's why hospitals have grown so much in previous years.
, however, the government's increasingly flat rate of payouts has put pressure on hospitals with rising costs compared to commercial health insurance. Once expansion slows or ends, hospitals face not only slower revenue growth due to fewer patients, but also lower payouts from government health-care users, who already make up a large proportion of their businesses, which significantly slows the growth of hospital revenue and profits. Because the proportion of users of government health insurance is increasing, the impact on primary hospitals, which previously benefited more obviously, is even greater. Unfortunately, Medicaid expansion has begun to shrink in the face of policy uncertainty, which has put enormous pressure on hospitals.
face these two challenges, primary hospitals have to find a way out, and their solutions are no more than open source savings. First, try to control costs in terms of cost-cutting, but in the face of rising costs of labor, drugs and equipment, many times still powerless, can only be done more in fine management, but this still does not solve the long-term pressure of falling revenue. As a result, open source is still urgent for small hospitals, mainly in two ways, one is to provide more integrated services, such as the packaging of surgical and postoperative services, primary hospitals can provide continuous services for the same patient, rather than leaving them to other outpatient services.
solution is to form an alliance with or merge directly with a large hospital. The advantage of primary hospitals is closer to the user, can be pre-diagnosis and post-diagnosis services are undertaken, and in the face of the value of medical assessment indicators, large hospitals also have the incentive to vertical mergers and acquisitions or cooperation to promote the actual rehabilitation of patients to avoid the problem of repeated hospitalization. However, for primary hospitals, the advantage of co-operation with large hospitals is first and foremost financial, and these small hospitals have easier access to financing. On the other hand, small hospitals can also gain better clinical ability to enhance their attractiveness.
In this unprecedented change in 30 years, the challenges facing primary hospitals in the United States are enormous, and as things stand, vertical cooperation will be the main direction of development for the integration of primary hospitals, while the payer will be the main driving force behind this change. (Diary of the Villageman)




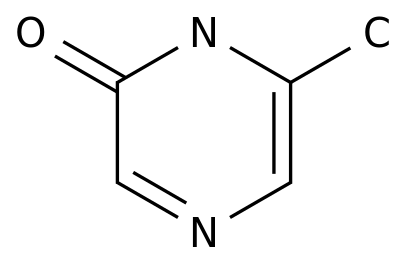
![2-(Hydroxymethyl)benzo[b]thiophene](https://file.echemi.com/fileManage/upload/cas/593/e79a972f-b55d-4dc1-9113-841c417e0a89.png)