-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*For medical professionals only
Identify the "tip of the iceberg" as early as possible
In recent years, many studies have pointed to an increasing
risk of death in patients with type 2 diabetes (T2DM) and diabetic nephropathy (DKD).
How to delay the disease progression of patients with DKD is also a topic
that many researchers have been exploring.
At this year's European Association for the Study of Diabetes (EASD) conference, Professor Anna Solini from Italy gave a special report
entitled "What else can we do to prevent and treat diabetic nephropathy".
Anna Solini noted that previous professors such as Fatima Rodriguez of Stanford University Hospital have analyzed the diagnosis of DKD in the real world and found that of the 245,978 patients diagnosed with DKD between January 1, 2017 and June 30, 2019, about 50% of the patients were first identified through electronic health records (HER); Another 50% of patients were diagnosed
by laboratory tests such as urinary albumin creatinine ratio (UACR) or estimated glomerular filtration rate (eGFR).
Of the patients evaluated for UACR/eGFR, more than 90% of patients were diagnosed with DKD
at the first test.
The time from the appearance of UACR/eGFR abnormalities to the diagnosis of DKD, and from the time of diagnosis of DKD to the start of drug therapy suggest that there is a delay
in intervention for DKD in the real world.
Traditional therapeutic agents for DKD include: angiotensin-invertase inhibitors (ACEi), angiotensin-II receptor blockers (ARBs), dihydropyridine calcium-channel blockers (CCBs), sodium-glucose cotransporter-2 inhibitors (SGLT-2i), gluconsin-1 receptor agonists (GLP-1RAs), metformin and other hypoglycemic drugs
.
The above drugs work
mainly by intervening in renal hemodynamics or improving metabolic indicators.
In this presentation, Professor Anna Solini introduced
the four aspects of nonsteroidal mineralocorticoid receptor antagonists, glucose-dependent insulin-promoting polypeptide (GIP) receptors and gluconsion-like peptide-1 (GLP-1) receptors, the role of web-based management measures in DKD management, and emerging therapeutic methods.
Nonsteroidal mineralocorticoid receptor antagonists
are affected by factors such as hyperglycemia, high salt intake, oxidative stress, etc.
, and patients have elevated levels of mineralocorticoids and over-activation of mineralocorticoid receptors (MR), leading to inflammation, glomerulosclerosis, sodium retention, and cardiovascular and renal disease
.
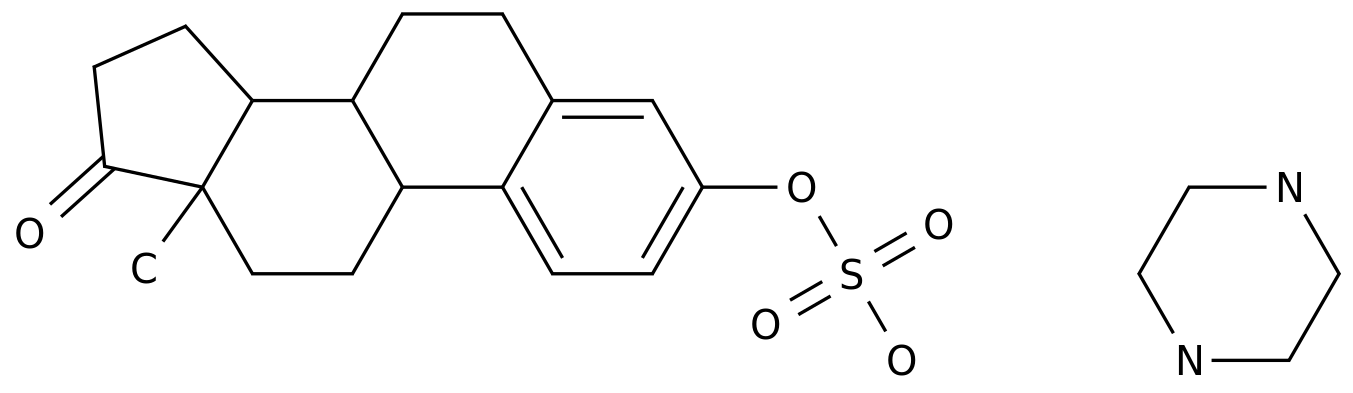
Nectone is a nonsteroidally selective mineralocorticoid receptor antagonist (MRA) that reduces the risk of
chronic kidney disease (CKD) progression, cardiovascular and renal events by binding to MR and blocking its overactivation.
Figure 1 The FIDELITY study, which synthesized populations from FIDELIO-DKD and
FIGARO-DKD studies, with a total of 13,026 participants with a median follow-up of 3 years, analyzed
the renal outcomes of patients with T2DM with DKD treated with fenerione.
The results find:
- Compared with placebo, the risk of eGFR decline ≥57% and eGFR decline of ≥40% was significantly reduced compared with placebo (see Figure 2);
- The incidence of compound renal outcomes (the time of the first occurrence of renal failure, a persistent decline in eGFR to 57%, or kidney death) was significantly lower in the phenanedione group than in the placebo group
.
360 patients (5.
5%) occurred in the fenetridone group and 465 patients (7.
1%) in the placebo group [HR, 0.
77; 95% confidence interval, (0.
67, 0.
88); P = 0.
0002];
- The incidence of complex renal outcomes (renal failure, sustained decline in eGFR up to 40%, or renal death) was significantly lower in the fenetrione group than in the placebo group
.
854 patients (13.
1%) occurred in the fenerione group and 995 patients (15.
3%) in the placebo group [HR, 0.
85; 95% confidence interval, (0.
77, 0.
93); P = 0.
0004]
。
Figure 2
By analyzing the use of SGLT-2i in the FIDELITY study, it was found that the renal benefit of fenerone was not related
to the use of SGLT-2i.
in the United States and Europe.
During the 2-year follow-up of the SURPASS-4 study, the average reduction of eGFR in patients in the Tirzepatide group was 1.
4 ml/min/1.
73 m2, and there was no significant change in UACR compared with baseline; In the insulin glargine group, eGFR decreased by 3.
6 ml/min/1.
73 m2, and UACR continued to rise
.
In addition, Tirzepatide reduced the magnitude of eGFR reduction regardless of whether the patient was using SGLT-2i or not
.
But although GLP-1/GIP receptor combination agonists have shown clear renal benefit in studies, there are still several things that need to be clarified: (1) The direct effect of GIP on the kidneys is not yet clear: it is currently unclear whether the human kidney expresses the GIP receptor, how the role of GIP on perirenal adipose tissue, and whether GIP can improve vascular endothelial function are also unclear
.
(2) The pharmacokinetics of Tirzepatide is not affected
by kidney function.
(3) In the future, there is an urgent need for randomized controlled studies (RCTs) comparing the effects of GLP-1RA and Tirzepatide on the kidneys
.
of network-based management measures in DKD management In a retrospective study, it was found that the predictive value of machine learning algorithm (MLA)-based predictive models for DKD progression was better than the risk score recommended by the Centers for Disease Control and Control (CDC), where the area under the subject's work characteristic curve (ROC) (AUC) predicted DKD progression was greater than 75%, up to 82%, The CDC risk score predicts less than 70%
of the area under the ROC curve for DKD progression.
The Department of Nephrology, First Medical Center of the General Hospital of the People's Liberation Army of the Chinese People's Liberation Army constructed a 3-year DKD risk prediction model
for T2DM patients with normal albuminuria based on MLA and electronic medical records (EMR).
The study included 816 patients with T2DM (585 men) from the PLA General Hospital for 3 years
.
Using 46 medical characteristic indicators easily available in EMR, a predictive model
based on 7 machine learning algorithms [LightGBM), extreme gradient enhancement, adaptive enhancement, artificial neural network, decision tree, support vector machine, logistic regression] was developed.
Using the area under ROC to evaluate the performance of the model, the results show that the LightGBM model AUC is the largest (see figure below), indicating that the model is a promising tool
in the crowd management strategy to promote T2DM care in the EMR era.
In this model, the variables were sorted from highest to lowest contribution to DKD risk over the next 3 years, followed by baseline age, high homocysteine, high glycosylated hemoglobin (HbA1c), high body mass index (BMI), low serum albumin (Alb), low eGFR, high bicarbonate, and high LDL levels
.
Figure 3
The purpose of the multiparameter response efficacy (PRE) score is to predict the long-term efficacy
of a drug by using changes in multiple early clinical parameters after it.
Studies of drugs such as ARB, GLP-1RA, and SGLT-2i have shown that changes in PRE scores are more reliable in predicting the long-term efficacy of drugs than changes in any single biomarker (see figure below
).
Figure 4
DKD can be prevented
by treating multiple targets.
Techniques such as technology-assisted team care and regular feedback can improve multiple indicators and clinical outcomes in patients with T2DM, but the effect of this intervention on patients with DKD is unclear
.
Professor Juliana C.
N.
Chan of the Prince of Wales Hospital of the University of Chinese Hong Kong and others evaluated the effects of the Asia Diabetes Joint Assessment (JADE) website, nurse reminders and team care on multiple risk factors for patients with DKD, and the results showed that the proportion of patients with multiple indicators in the web-based intervention treatment group was the highest compared with conventional treatment (see figure below).
Figure 5
Emerging therapeutic measures such as endothelin receptor antagonists, apoptosis signal-modulating kinase-1 activators, JAK-STAT inhibitors, calorie restriction, and reduction of end-of-products (AGEs) in food can improve inflammation and glomerulosclerosis, and have been shown to reduce urine protein and delay the decline rate
of eGFR.
- The SONAR study showed that the selective endothelin A receptor antagonist Atrasentan treatment significantly reduced the risk of
the primary renal compound endpoint [HR 0.
65;95% CI (0.
49 to 0.
88);p = 0.
0047], serum creatinine multiplication, and progression to ESRD in patients with T2DM and CKD.
- Selonsertib belongs to the apoptosis signal-modulating kinase-1 activator that exerts a kidney-protective effect
primarily by inhibiting inflammation and glomerulosclerosis.
Glenn M.
Chertow et al.
studied the effect of Selonsertib on patients with DKD, which included 333 patients with T2DM and DKD, with a mean age of 62 years, baseline eGFR 31 ml/min/1.
73m2 The results were randomly divided into placebo group (n=85), Selonsertib 2mg group (n=81), 6mg group (n=84), and 18mg group (n=83), and the results showed that at 48 weeks, the change of eGFR from baseline was not statistically significant between groups, but the eGFR decline in the Selonsertib 18mg group was 71% lower than that in the placebo group during 4 weeks to 48 weeks of treatment (see figure below).
Figure 6
- The mechanism of the protective effect of calorie restriction on the kidneys is unclear
.
Changes in weight loss, blood pressure, cholesterol, fasting insulin levels, insulin resistance, insulin growth factor-1, body temperature, energy expenditure at rest, oxidative stress, and inflammatory mediators may all be related
to kidney protection.
Nephropathy that may benefit from calorie restriction includes CKD, DKD, obesity-associated nephropathy, polycystic kidney, and ischemia-reperfusion injury
.
However, the adherence to long-term calorie restriction, long-term effects on health, effects on protein-energy balance, effects on wound healing, and effects on bone mineral salt metabolism still need attention
.
- Different foods have different levels of late glycosylation end products (AGEs), and red meat has higher levels of AGE, such as beef
.
However, the same kind of food is processed by different cooking methods, and the AGE content is also significantly different
.
For example, the AGE content of roast beef is significantly higher than that of boiled beef, the AGE content of fried potato chips is much higher than that of boiled potato chips, and the use of vinegar and lemon juice pretreatment before roast beef can significantly reduce the AGE content
of beef.
All in all, foods with high fat content also have higher AGE content, and cooking methods such as high-temperature frying can further increase the AGE content in food compared to the practice of
boiling.
Professor Anna Solini concluded by saying that we still need more evidence-based medical evidence
for DKD prevention and control.
Through the control of multiple metabolic indicators such as blood glucose, blood pressure, and blood lipids, team-based comprehensive management measures such as RAS blockers, nonsteroidal mineralocorticoid receptor antagonists (fenerone), SGLT-2i, GLP-1RA, statins, etc.
, through continuous support to promote patient self-management, etc.
, are conducive to the management
of patients with DKD.
This article is written by the review experts
Reference source:
com).