-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
The 2021 American Society of Clinical Oncology (ASCO) annual meeting will be held in the near future.
A number of studies announced at the meeting will explore the efficacy and safety of new drugs in acute myeloid leukemia (AML).
The editor now organizes the main content of the research as follows for the reference of readers.
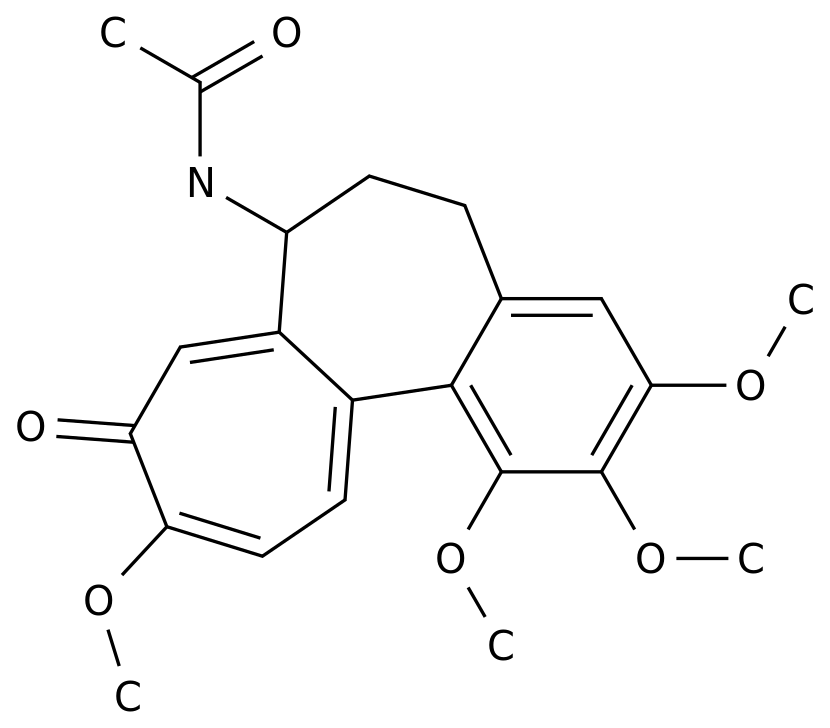
Abstract 7006: Olutasidenib (FT-2102) in the treatment of relapsed and refractory mIDH1 acute myeloid leukemia: Phase II study interim analysis results Research background Oral, potent mIHD1 inhibitor Olutasidenib has shown good results in high-risk AML patients in phase I trials Tolerability and clinical activity (Watts, Blood 2019).
The results of a phase II trial (NCT02719574) of Olutasidenib as a single agent for the treatment of relapsed or refractory (R/R) mIDH1 AML patients are now announced.
Research method The study evaluated the efficacy of AML patients with mIDH1R132X who were first administered ≥180 days before the data cutoff (June 20, 2018).
The primary endpoint of the study was complete remission (CR) + complete remission (CRh) rate with partial hematological recovery.
Study results The study included 153 R/R AML patients who received Olutasidenib monotherapy for a median of 5.
5 months (95% CI: 4.
4-8.
7).
Among them, 43 patients (28%) continued to receive treatment, and 100 patients (72%) stopped treatment.
The most common reasons for stopping treatment were disease deterioration (31%), adverse reactions (14%), death (10%), and transplantation (8%).
The median age of the 123 patients who can be evaluated for efficacy was 71 years (range: 32-87), and the median number of previous treatments was 2 (range: 1-7).
The CR+CRh rate of Olutasidenib in the treatment of AML patients in the study was 33%, of which the CR rate was 30%.
Sensitivity analysis showed that if transplantation or recurrence were regarded as the end of disease remission, the median duration of remission of CR+CRh in AML patients did not reach or was 13.
8 months, respectively.
The overall response rate (ORR) was 46%, and the median duration of ORR was 11.
7 months.
In patients with baseline blood transfusion dependence and CR+CRh after treatment, platelet transfusion independence (TI) and red blood cell TI increased by 100% and 83% at 56 days, respectively.
Platelet TI and red blood cell TI increased at 56 days in patients who did not reach CR+CRh 50% and 56%.
The median overall survival (OS) of the patients in the study was 10.
5 months.
Among them, the median OS of patients who reached CR+CRh did not reach, and the estimated 18-month OS rate was 87%.
The treatment-related adverse events (TEAE) with an incidence of ≥25% in the study included nausea (38%), constipation (25%), and leukocytosis (25%).
Grade 3-4 TEAEs with an incidence of ≥10% include febrile neutropenia (20%), anemia (19%), thrombocytopenia (16%), and neutropenia (13%).
The researchers assessed the IDH1 differentiation syndrome (all grades) in 21 patients (14%).
Most of the patients were resolved by related treatments, 1 patient died, and 19 patients had leukocytosis.
Study conclusion Olutasidenib is well tolerated in high-risk R/R mIDH1 AML patients and can bring lasting complete remission.
All patients who achieved disease remission achieved TI, and those who achieved CR+CRh had longer remission duration and OS, and had better clinical benefits.
Abstract 7007: The efficacy and safety of Aspacytarabine (BST-236) as a single-agent first-line treatment for AML patients who are not suitable for standard chemotherapy.
Background Aspacytarabine (BST-236) is a prodrug of cytarabine, the mainstay of standard chemotherapy for AML. Cytarabine has certain toxicity and cannot be used in elderly patients and patients with comorbidities.
Aspacytarabine is inactive until it releases cytarabine through pharmacokinetics, reduces the systemic exposure to the peak level of toxic cytarabine, reduces systemic toxicity and relatively protects normal tissues, so that it can be used when it is not suitable to receive high doses of cytarabine.
Glycocytidine is used in the treatment of patients.
A phase IIb study (NCT03435848) explored the efficacy and safety of Aspacytarabine monotherapy in newly diagnosed AML patients who are not suitable for standard chemotherapy.
Research Method The study is an unblinded, single-arm, phase IIb study, which included patients with AML who had secondary AML and had previously received demethylation drugs (HMA).
In the induction treatment and consolidation treatment phases, 1-2 courses and 1-3 courses of 4.
5g/m2/d (including 3g/m2/d cytarabine) Aspacytarabine treatment were received respectively.
Each course consists of 6 times a day Consists of 1 hour infusion.
Results of the study The study is currently ongoing.
The study included 46 newly diagnosed AML patients (median age 75 years) who were not suitable for standard chemotherapy and received Aspacytarabine treatment and completed 1-4 courses of 4.
5g/m2/d Aspacytarabine Treatment, of which 26 (63%) patients had new-onset AML, and 17 (37%) patients had secondary AML.
Six patients (13%) had previously received HMA treatment (median received 12 courses of treatment).
The median baseline ratio of bone marrow blast cells in the study was 52%, 54% and 29% of patients had poor or medium European Leukemia Network (ELN) scores, and 20 patients (43%) had ECOG scores of 2 points.
Aspacytarabine is safe and well tolerated during repeated administration.
Drug-related adverse events of grade ≥2 were mainly hematological events and infections, and the 30-day mortality rate was 11%.
Among the 43 patients whose curative effect can be assessed at present, 15 patients (35%) achieved CR after 1 course (13 patients) or 2 courses (2 patients) of induction therapy, and all patients achieved complete hematological remission ( Median 27.
5 days, range: 22-39 days).
The CR rates for new-onset AML patients and those with poor ELN scores were 46% and 33%, respectively.
Of the 11 patients currently assessable for minimal residual disease (MRD) status, 8 patients (73%) are MRD negative.
Although the duration of Aspacytarabine treatment is limited, the median duration of remission and median OS were not reached for patients in remission at a median follow-up of 12 months and 24 months (end of follow-up).
Research conclusions The research results show that the first-line treatment of Aspacytarabine is not suitable for intensive chemotherapy for AML patients in a limited period of time.
Aspacytarabine may bring new chemotherapy options for these patients.
Abstract 7008: The first phase of human research results of FLT3 inhibitor FF-10101-01 in the treatment of relapsed and refractory AML.
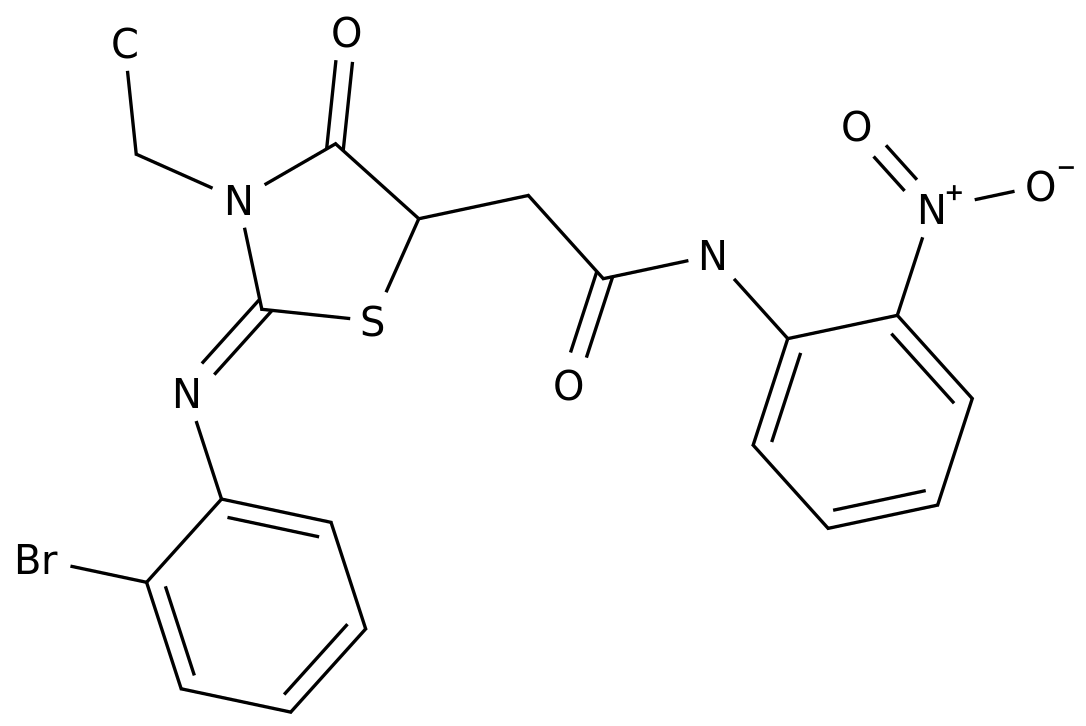
Background FF-10101-01 is a selective and irreversible inhibitor of FMS-like tyrosine kinase 3 (FLT3).
It has strong in vitro activity against AML with FLT3 mutations.
FF-10101-01 for FLT3 internal tandem repeat (ITD) mutations associated with high relapse rate and low survival/remission rate, as well as drug-resistant D835 and F691 tyrosine kinase domain (TKD) and atypical FLT3 activation The mutation has high activity.
The results of a phase I study exploring the safety, efficacy, pharmacokinetics and pharmacodynamics of FF-10101-01 in R/R AML are now announced.
Research method In order to determine the recommended phase II dose, the study included AML patients with or without FLT3 mutations orally once (QD) or twice a day (BID) FF-10101-01 until the patient received no further clinical benefit or appeared Untolerable adverse reactions.
Research results The study included 52 patients, with a median age of 61 years (range: 21-84), and 52% of the patients were women.
Of the 52 patients, 22 (42%) patients had FLT3-ITD mutations, 5 patients had FLT3-TKD mutations, 1 patient had both FLT3-ITD mutations and FLT3-TKD mutations, and 24 patients (46%) in the control group There is no FLT3 mutation.
The study included patients who received continuous administration of 10-225mg QD or 50-100mg BID FF-10101-01.
The median number of previous treatments was 3 (range: 0-6), and most (82%) patients with FLT3 mutations had been treated with FLT3 inhibitors.
The median duration of the study was 5.
7 weeks (range: 0.
1-36).
FF-10101-01 was well tolerated, with a total daily dose of 150 mg.
The most common treatment-related adverse reactions included nausea (n=18, 35%), diarrhea (n=14, 27%), elevated creatine kinase (n=14, 27%), and vomiting (n=10, 19%) ), aspartate aminotransferase increased (n=10, 19%).
Grade 3-4 differentiation syndrome was observed in patients receiving 75-150 mg/day dose (n=4, 8%).
Dose-limiting cardiotoxicity (heart failure with reduced ejection fraction, increased grade 3 troponin/CK) was observed in patients who received a total daily dose of ≥200 mg.
The cytogenetic complete remission (CRc) rate of 30 patients with evaluable efficacy was 13%, 1 patient who received 75 mg BID dose (FLT3-ITD mutation) reached CR, and 1 patient who received 100 mg BID dose (FLT3) -Wt mutation) achieved complete remission (CRp) with incomplete recovery of platelets, and 2 patients who received 50 mg BID doses achieved complete remission (CRi) with incomplete recovery of blood counts.
One patient had previously received FLT3 inhibitor (Jiri Tinib) disease progression after treatment.
The median time to disease remission in the study was 13.
3 weeks. Four patients who received 50-150 mg daily doses achieved partial remission (PR), of which two patients had FLT3-ITD mutations and had previously been treated with FLT3 inhibitors.
When the dosage is ≥75mg BID, the trough plasma concentration is >90ng/ml, and it is associated with >90% inhibition of p-FLT3 during the administration period.
Research conclusions The FLT3 inhibitor FF-10101-01 has shown a certain effect on R/R AML patients with FLT3-ITD mutations who are resistant to geritinib and other FLT3 inhibitors.
The dose of 50-75 mg BID is well tolerated and can bring sustained FLT3 inhibition.
Reference source: 1.
Stephane De Botton, et al.
Effect of olutasidenib (FT-2102) on complete remissions in patients with relapsed/refractory (R/R) mIDH1 acute myeloid leukemia (AML): Results from a planned interim analysis of a phase 2 clinical trial.
2021 ASCO Annual Meeting.
Abstract 7006.
2.
Jessica K.
Altman, et al.
Efficacy and safety of aspacytarabine (BST-236) as a single-agent, first-line therapy for patients with acute myeloid leukemia unfit for standard chemotherapy.
2021 ASCO Annual Meeting.
Abstract 7007.
3.
Mark J.
Levis, et al.
Phase 1 first-in-human study of irreversible FLT3 inhibitor FF-10101-01 in relapsed or refractory acute myeloid leukemia.
2021 ASCO Annual Meeting.
Abstract 7008 .
Poke "read the original text", we make progress together
A number of studies announced at the meeting will explore the efficacy and safety of new drugs in acute myeloid leukemia (AML).
The editor now organizes the main content of the research as follows for the reference of readers.
Abstract 7006: Olutasidenib (FT-2102) in the treatment of relapsed and refractory mIDH1 acute myeloid leukemia: Phase II study interim analysis results Research background Oral, potent mIHD1 inhibitor Olutasidenib has shown good results in high-risk AML patients in phase I trials Tolerability and clinical activity (Watts, Blood 2019).
The results of a phase II trial (NCT02719574) of Olutasidenib as a single agent for the treatment of relapsed or refractory (R/R) mIDH1 AML patients are now announced.
Research method The study evaluated the efficacy of AML patients with mIDH1R132X who were first administered ≥180 days before the data cutoff (June 20, 2018).
The primary endpoint of the study was complete remission (CR) + complete remission (CRh) rate with partial hematological recovery.
Study results The study included 153 R/R AML patients who received Olutasidenib monotherapy for a median of 5.
5 months (95% CI: 4.
4-8.
7).
Among them, 43 patients (28%) continued to receive treatment, and 100 patients (72%) stopped treatment.
The most common reasons for stopping treatment were disease deterioration (31%), adverse reactions (14%), death (10%), and transplantation (8%).
The median age of the 123 patients who can be evaluated for efficacy was 71 years (range: 32-87), and the median number of previous treatments was 2 (range: 1-7).
The CR+CRh rate of Olutasidenib in the treatment of AML patients in the study was 33%, of which the CR rate was 30%.
Sensitivity analysis showed that if transplantation or recurrence were regarded as the end of disease remission, the median duration of remission of CR+CRh in AML patients did not reach or was 13.
8 months, respectively.
The overall response rate (ORR) was 46%, and the median duration of ORR was 11.
7 months.
In patients with baseline blood transfusion dependence and CR+CRh after treatment, platelet transfusion independence (TI) and red blood cell TI increased by 100% and 83% at 56 days, respectively.
Platelet TI and red blood cell TI increased at 56 days in patients who did not reach CR+CRh 50% and 56%.
The median overall survival (OS) of the patients in the study was 10.
5 months.
Among them, the median OS of patients who reached CR+CRh did not reach, and the estimated 18-month OS rate was 87%.
The treatment-related adverse events (TEAE) with an incidence of ≥25% in the study included nausea (38%), constipation (25%), and leukocytosis (25%).
Grade 3-4 TEAEs with an incidence of ≥10% include febrile neutropenia (20%), anemia (19%), thrombocytopenia (16%), and neutropenia (13%).
The researchers assessed the IDH1 differentiation syndrome (all grades) in 21 patients (14%).
Most of the patients were resolved by related treatments, 1 patient died, and 19 patients had leukocytosis.
Study conclusion Olutasidenib is well tolerated in high-risk R/R mIDH1 AML patients and can bring lasting complete remission.
All patients who achieved disease remission achieved TI, and those who achieved CR+CRh had longer remission duration and OS, and had better clinical benefits.
Abstract 7007: The efficacy and safety of Aspacytarabine (BST-236) as a single-agent first-line treatment for AML patients who are not suitable for standard chemotherapy.
Background Aspacytarabine (BST-236) is a prodrug of cytarabine, the mainstay of standard chemotherapy for AML. Cytarabine has certain toxicity and cannot be used in elderly patients and patients with comorbidities.
Aspacytarabine is inactive until it releases cytarabine through pharmacokinetics, reduces the systemic exposure to the peak level of toxic cytarabine, reduces systemic toxicity and relatively protects normal tissues, so that it can be used when it is not suitable to receive high doses of cytarabine.
Glycocytidine is used in the treatment of patients.
A phase IIb study (NCT03435848) explored the efficacy and safety of Aspacytarabine monotherapy in newly diagnosed AML patients who are not suitable for standard chemotherapy.
Research Method The study is an unblinded, single-arm, phase IIb study, which included patients with AML who had secondary AML and had previously received demethylation drugs (HMA).
In the induction treatment and consolidation treatment phases, 1-2 courses and 1-3 courses of 4.
5g/m2/d (including 3g/m2/d cytarabine) Aspacytarabine treatment were received respectively.
Each course consists of 6 times a day Consists of 1 hour infusion.
Results of the study The study is currently ongoing.
The study included 46 newly diagnosed AML patients (median age 75 years) who were not suitable for standard chemotherapy and received Aspacytarabine treatment and completed 1-4 courses of 4.
5g/m2/d Aspacytarabine Treatment, of which 26 (63%) patients had new-onset AML, and 17 (37%) patients had secondary AML.
Six patients (13%) had previously received HMA treatment (median received 12 courses of treatment).
The median baseline ratio of bone marrow blast cells in the study was 52%, 54% and 29% of patients had poor or medium European Leukemia Network (ELN) scores, and 20 patients (43%) had ECOG scores of 2 points.
Aspacytarabine is safe and well tolerated during repeated administration.
Drug-related adverse events of grade ≥2 were mainly hematological events and infections, and the 30-day mortality rate was 11%.
Among the 43 patients whose curative effect can be assessed at present, 15 patients (35%) achieved CR after 1 course (13 patients) or 2 courses (2 patients) of induction therapy, and all patients achieved complete hematological remission ( Median 27.
5 days, range: 22-39 days).
The CR rates for new-onset AML patients and those with poor ELN scores were 46% and 33%, respectively.
Of the 11 patients currently assessable for minimal residual disease (MRD) status, 8 patients (73%) are MRD negative.
Although the duration of Aspacytarabine treatment is limited, the median duration of remission and median OS were not reached for patients in remission at a median follow-up of 12 months and 24 months (end of follow-up).
Research conclusions The research results show that the first-line treatment of Aspacytarabine is not suitable for intensive chemotherapy for AML patients in a limited period of time.
Aspacytarabine may bring new chemotherapy options for these patients.
Abstract 7008: The first phase of human research results of FLT3 inhibitor FF-10101-01 in the treatment of relapsed and refractory AML.
Background FF-10101-01 is a selective and irreversible inhibitor of FMS-like tyrosine kinase 3 (FLT3).
It has strong in vitro activity against AML with FLT3 mutations.
FF-10101-01 for FLT3 internal tandem repeat (ITD) mutations associated with high relapse rate and low survival/remission rate, as well as drug-resistant D835 and F691 tyrosine kinase domain (TKD) and atypical FLT3 activation The mutation has high activity.
The results of a phase I study exploring the safety, efficacy, pharmacokinetics and pharmacodynamics of FF-10101-01 in R/R AML are now announced.
Research method In order to determine the recommended phase II dose, the study included AML patients with or without FLT3 mutations orally once (QD) or twice a day (BID) FF-10101-01 until the patient received no further clinical benefit or appeared Untolerable adverse reactions.
Research results The study included 52 patients, with a median age of 61 years (range: 21-84), and 52% of the patients were women.
Of the 52 patients, 22 (42%) patients had FLT3-ITD mutations, 5 patients had FLT3-TKD mutations, 1 patient had both FLT3-ITD mutations and FLT3-TKD mutations, and 24 patients (46%) in the control group There is no FLT3 mutation.
The study included patients who received continuous administration of 10-225mg QD or 50-100mg BID FF-10101-01.
The median number of previous treatments was 3 (range: 0-6), and most (82%) patients with FLT3 mutations had been treated with FLT3 inhibitors.
The median duration of the study was 5.
7 weeks (range: 0.
1-36).
FF-10101-01 was well tolerated, with a total daily dose of 150 mg.
The most common treatment-related adverse reactions included nausea (n=18, 35%), diarrhea (n=14, 27%), elevated creatine kinase (n=14, 27%), and vomiting (n=10, 19%) ), aspartate aminotransferase increased (n=10, 19%).
Grade 3-4 differentiation syndrome was observed in patients receiving 75-150 mg/day dose (n=4, 8%).
Dose-limiting cardiotoxicity (heart failure with reduced ejection fraction, increased grade 3 troponin/CK) was observed in patients who received a total daily dose of ≥200 mg.
The cytogenetic complete remission (CRc) rate of 30 patients with evaluable efficacy was 13%, 1 patient who received 75 mg BID dose (FLT3-ITD mutation) reached CR, and 1 patient who received 100 mg BID dose (FLT3) -Wt mutation) achieved complete remission (CRp) with incomplete recovery of platelets, and 2 patients who received 50 mg BID doses achieved complete remission (CRi) with incomplete recovery of blood counts.
One patient had previously received FLT3 inhibitor (Jiri Tinib) disease progression after treatment.
The median time to disease remission in the study was 13.
3 weeks. Four patients who received 50-150 mg daily doses achieved partial remission (PR), of which two patients had FLT3-ITD mutations and had previously been treated with FLT3 inhibitors.
When the dosage is ≥75mg BID, the trough plasma concentration is >90ng/ml, and it is associated with >90% inhibition of p-FLT3 during the administration period.
Research conclusions The FLT3 inhibitor FF-10101-01 has shown a certain effect on R/R AML patients with FLT3-ITD mutations who are resistant to geritinib and other FLT3 inhibitors.
The dose of 50-75 mg BID is well tolerated and can bring sustained FLT3 inhibition.
Reference source: 1.
Stephane De Botton, et al.
Effect of olutasidenib (FT-2102) on complete remissions in patients with relapsed/refractory (R/R) mIDH1 acute myeloid leukemia (AML): Results from a planned interim analysis of a phase 2 clinical trial.
2021 ASCO Annual Meeting.
Abstract 7006.
2.
Jessica K.
Altman, et al.
Efficacy and safety of aspacytarabine (BST-236) as a single-agent, first-line therapy for patients with acute myeloid leukemia unfit for standard chemotherapy.
2021 ASCO Annual Meeting.
Abstract 7007.
3.
Mark J.
Levis, et al.
Phase 1 first-in-human study of irreversible FLT3 inhibitor FF-10101-01 in relapsed or refractory acute myeloid leukemia.
2021 ASCO Annual Meeting.
Abstract 7008 .
Poke "read the original text", we make progress together