-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Case data
The patient, a 69-year-old female, had a history of right breast cancer resection, developed cough and sputum, and was referred to our department due to abnormal chest shadow (Figure 1A, top left).
General laboratory tests show C-reactive protein levels of 0.
92 mg/dl
.
CT shows cavitary lesions in the upper lobe of the left lung, multiple nodules and consolidation of the lobe of the tongue lobe (Figure 1A, upper right).
Nontuberculous mycobacterial (NTM) lung disease is suspected, repeat sputum examination of acid-fast bacilli (AFB) (smear, culture, and PCR), no mycobacteria
detected.
Bronchoscopy was performed, and Kinyoun's modified Ziehl–Neelsen staining detected filamentous branched microorganisms in the bronchial lavage fluid (Figure 1A, below).
AFB culture and PCR of the lavage solution were negative, but bacterial cultures of gram-positive bacteria were positive
.
16SRRNA gene sequencing was used to identify the isolate as Nocardiosis and confirmed as pulmonary nocardiosis
.
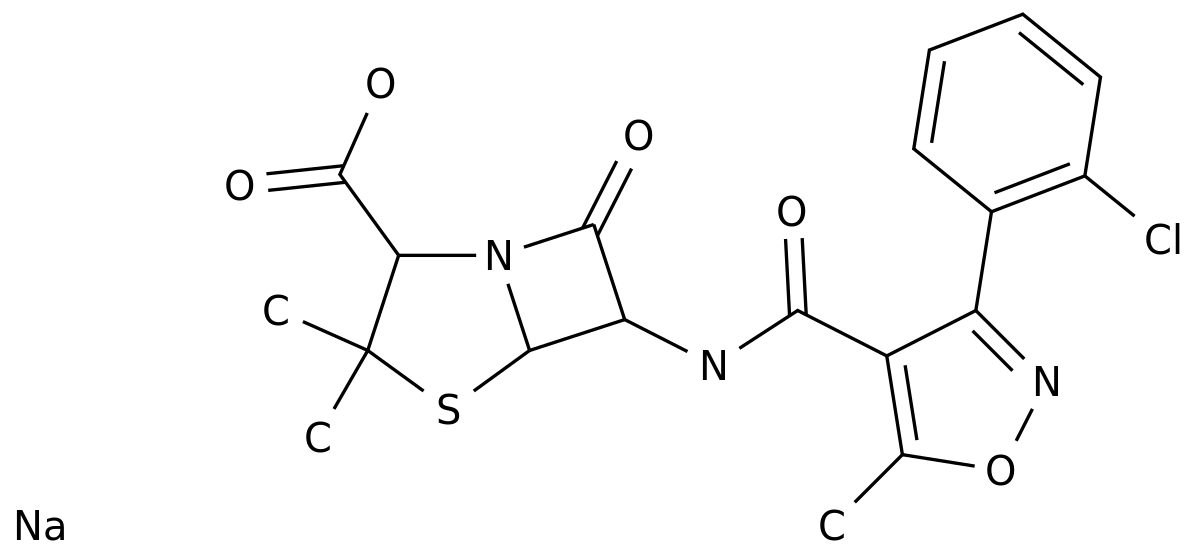
According to the results of the drug susceptibility test, the patient was given imipenem treatment for 2 weeks and then switched to oral faropenem treatment
.
After 2 months, CT showed improvement in all lesions (Figure 1B).
Fig.
1 Results of radiological examination before treatment (top left: chest x-ray, upper right: CT) and Kinyoun-modified Ziehl–Neelsen staining of bronchial lavage fluid (bottom); B CT results after 2 months of treatment showed significant improvement
in lesions.
Analyze the discussion
Nocardiosis is a gram-positive aerobic bacterium that is usually found in soil, water, or air
.
Mycelium can be formed in the air, human inhalation of mycelial fragments is the main route of infection, can also enter the human body through broken skin or digestive tract, usually sporadic
.
The disease tends to occur in immunocompromised patients, and the predisposing factors are corticosteroids, immunosuppressants or broad-spectrum antibiotics, kidney transplantation, malignant tumors, AIDS, etc.
, such as this patient has a history of
right breast cancer resection.
Pulmonary nocardiosis is the most common clinical manifestation of nocardiosis infection, often causing symptoms such as cough, sputum production, shortness of breath, chest tightness, fever and night sweats, weight loss, and progressive fatigue, without obvious specificity
.
CT images of pulmonary nocardiosis are diverse
.
Bilateral lung consolidation, nodules, masses, and cavitation are common in immunosuppressed patients, while nodular/bronchiectasis is
often observed in immunocompetent patients.
Nocardiosis with predominance of midlobe and/or lobe lesions should be differentiated from
NTM lung disease.
Some cases involve co-infection with NTM pulmonopathy and some are colonized, making diagnosis of similar cases challenging, regardless of NTM test results, nocardiosis
should be considered in the differential diagnosis of NTM pulmonalosis-like lesions.
Because the clinical symptoms and imaging manifestations of pulmonary nocardiosis are atypical, in addition to the NTM lung disease considered in this case, pulmonary nocardiosis is also easily misdiagnosed as radiation mycosis and tuberculosis, and should be distinguished from other lower respiratory tract infections
.
Nocardiobacter infection should also be considered
in immunocompromised patients with acute, subacute, and chronic pneumonia.
At present, the diagnosis of Nocardiosis infection is mainly based on microbiological examination, and the traditional method mainly relies on smear, culture, and biochemical reaction identification, but with the development of molecular biology technology, whether it is mass spectrometry identification of cultured colonies, or direct high-throughput sequencing with specimens, the application of new methods has greatly improved the identification speed and accuracy
.
For the treatment of pulmonary nocardiosis, the recommended preferred regimen in "Fever: Sanford Antimicrobial Guidelines (48th Edition)" is a combination of sulfamethoxazole (15 mg/kg·d, intravenous) or oral divided into 2~4 times + imipenem (500 mg q6h, intravenous) for × 3~4 weeks, followed by a reduction of the compound sulfamethoxazole to 10 mg/kg·d 2~4 times ×for 3~6 months, and the secondary regimen is imipenem (500 mg q6h, intravenously) + amikacin (7.
5 mg/kg q12h, intravenously) × 3~4 weeks, followed by oral compound sulfamethoxazole, the course of treatment for immunocompetent patients is 3 months, and the course of treatment for immunocompromised patients is 6 months
.
References:
1.
Nakagoshi K, Yaguchi T, Takahashi K,et al.
Pulmonary nocardiosis caused by Nocardia pneumoniae mimicking non-tuberculous mycobacterial disease.
QJM.
2022 Sep 22; 115(9):625-626.
2.
Han Yungang, Han Junlei, Chen Huihui, Li Zheng, Zhao Yue, Xia Shuang, Cheng Meijin, Wang Wei, Ma Bing.
Clinical features and pathogenic bacteria resistance in 42 patients with pulmonary nocardiosis[J].
Chinese Journal of Infection Control,2022,21(07):668-674.
)
3.
LI Lanjuan,WANG Yuming.
Infectious Diseases.
Eight-year textbook 3rd edition.
Beijing:People's Medical Publishing House,2015.
]
4.
Fever Sanford Antimicrobial Therapy Guidelines: 48th Edition / David N.
Gilbert et al.
editors; Translated by Fan Hongwei.
—Beijing: Peking Union Medical College Press, 2019.
5