-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Bladder cancer is one of the most common malignancies of the
urinary system.
According to the depth of invasion of local tumors, bladder cancer can be divided into non-muscle-invasive bladder cancer and muscle-invasive bladder cancer (MIBC).
The bladder wall can be divided into four layers from the inside to the outside: mucosal layer, submucosal layer, muscular layer, and serous layer
.
When a tumor invades the muscular layer, serosal layer, and even the organs around the bladder, it is called muscle-invasive bladder cancer
.
Radical cystectomy (RC) after neoadjuvant chemotherapy (NAC) is the standard treatment for muscle-invasive bladder cancer (MIBC
。 Despite receiving aggressive treatment (NAC + RC), more than 40% of patients with MIBC relapse or die
within 3 years.
In addition, NAC remains underutilized in most patients due to cisplatin non-eligibility or chemotherapy-related toxicity.
Therefore, there is an urgent need to develop new treatment options
for MIBC patients.
On October 19, 2022, the Zu Xiongbing team of Central South University published an online title in Cell Reports Medicine (IF=17).
Research paper "Neoadjuvant immunotherapy, chemotherapy, and combination therapy in muscle-invasive bladder cancer: A multi-center real-world retrospective study", To parallelize neoadjuvant immunotherapy (tislelizumab), neoadjuvant chemotherapy (gemcitabine and cisplatin), and neoadjuvant combination therapy in patients with muscle-invasive bladder cancer (tislelizumab + GC) and exploring predictors of efficacy, which conducted a multicenter, real-world cohort study that demonstrated the highest rates of complete response and pathologic de-staging compared
with neoadjuvant immunotherapy or chemotherapy.
In conclusion, this study highlights the benefits of tislelizumab-based neoadjuvant combination therapy for MIBC.
Immune checkpoint blockade (ICB), including anti-PD-1/PD-L1, has shown promising survival benefits and revolutionized the status quo
of treatment for patients with advanced MIBC.
The safety and efficacy of neoadjuvant ICB (NICB) in MIBC has been demonstrated
by two prospective clinical trials.
Similarly, the safety and efficacy of the combination of NAC and NICB in the treatment of MIBC (NAC.
NICB)
。 These clinical trials have initially laid the foundation for the clinical application of neoadjuvant therapy based on anti-PD-1/PD-L1 in MIBC.
The role of emerging anti-PD-1/PD-L1 drugs, such as tislelizumab, in neoadjuvant therapy remains to be further studied, particularly in
Chinese populations.
Tislelizumab is a humanized monoclonal antibody with a higher binding affinity to the PD-1 receptor than common anti-PD-1 drugs
.
The second advantage of tislelizumab is its ability to minimize its binding to Fcγ receptors on macrophages, avoiding antibody-dependent phagocytosis, which is the mechanism
of T cell clearance and potential resistance to anti-PD-1 therapy.
Another significant advantage of tislelizumab over other anti-PD-L1/PD-1 drugs is its lower
price.
Current clinical trials have shown that tislelizumab significantly improves the prognosis of several advanced malignancies, including MIBC
.
In addition, tislelizumab combination chemotherapy has a better survival benefit and similar
side effects compared with chemotherapy alone.
Based on these promising results, tislelizumab has been approved
in China.
In this study, researchers conducted this real-world study at 15 regional medical centers to parallelize the effectiveness and safety
of NAC, NICB, and NAC.
By including 253 patients receiving neoadjuvant therapy from 15 tertiary hospitals (combination therapy: 98 cases, chemotherapy: 107 Immunotherapy: 48 cases).
Studies have shown that neoadjuvant combination therapy achieves the highest rates of complete response and pathological de-staging compared
with neoadjuvant immunotherapy or chemotherapy.
Moreover, the researchers developed and validated a efficacy prediction model with clinical features of pretreatment, which can pinpoint candidates
for neoadjuvant combination therapy.
Preliminary studies have also found that patients who achieve pathologic complete response after neoadjuvant therapy plus maximal transurethral resection of bladder tumors may be safe, and patients who achieve pathological complete response after neoadjuvant therapy plus maximal TURBT can safely receive bladder-sparing therapy
during short-term follow-up.
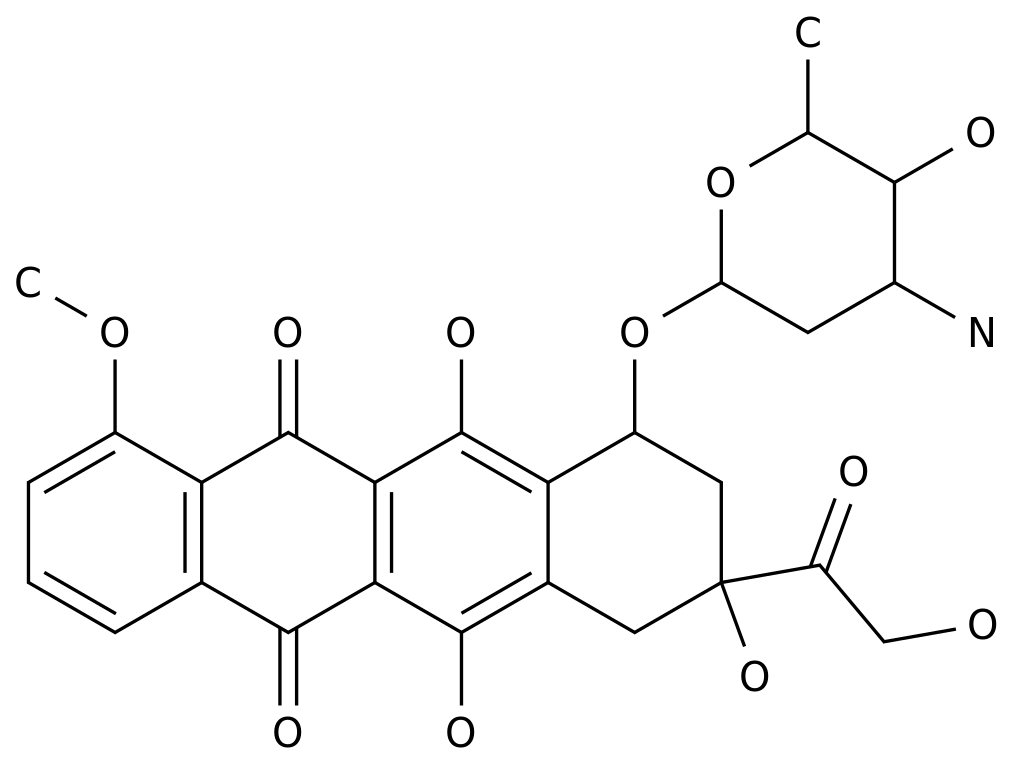
Overview of the study (Image from Cell Reports Medicine).
In conclusion, the study showed that neoadjuvant chemotherapy immunotherapy consisting of GC and tislelizumab achieved the highest complete response rate and pathological de-staging rate compared with neoadjuvant chemotherapy and neoadjuvant immunotherapy alone in the same real-world clinical practice setting, and neoadjuvant chemotherapy immunotherapy can be safely applied to patients with
MIBC.
In addition, the study established and validated a efficacy prediction model that could help identify candidates for neoadjuvant chemotherapy immunotherapy
.
Original link:
#