-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
1.
1.
Infect
Main complaint : Found lung shadow for more than 1 month
Chief complaintHistory of present illness :
History of present illness-
2021-03-20 Outer hospital physical examination chest CT: Irregular nodules are seen next to the interlobular fissure of the left lower lobe, with a little blurred edge on the edge, about 15mm×13mm
-
2021-04-08 Re-examination of chest CT: the lesion in the lower lobe of the left lung is enlarged than before, about 22mm×16mm
2021-03-20 Outer hospital physical examination chest CT: Irregular nodules are seen next to the interlobular fissure of the left lower lobe, with a little blurred edge on the edge, about 15mm×13mm
2021-03-20 Outer hospital physical examination chest CT: Irregular nodules are seen next to the interlobular fissure of the left lower lobe, with a little blurred edge on the edge, about 15mm×13mm
2021-04-08 Re-examination of chest CT: the lesion in the lower lobe of the left lung is enlarged than before, about 22mm×16mm
2021-04-08 Re-examination of chest CT: the lesion in the lower lobe of the left lung is enlarged than before, about 22mm×16mm
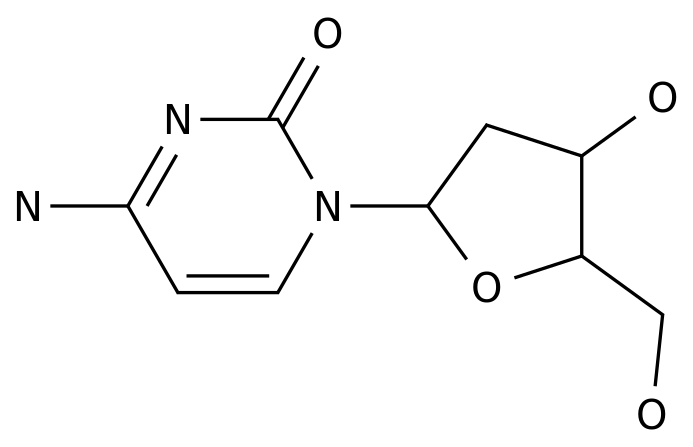
Past history : Allogeneic kidney transplantation was performed on March 2020; current medications: tacrolimus 1 mg bid, mycophenolate mofetil 0.
Past history
2.
2.
【Physical Examination】
-
T 36.
-
He is clear and energetic.
T 36.
T 36.
He is clear and energetic.
He is clear and energetic.
There is no swelling of the superficial lymph nodes all over the body.
The breath sounds on auscultation of the lungs are clear, and the rales are less than dry and wet
.
【Auxiliary Inspection】
【Auxiliary Inspection】-
Blood routine: WBC 8.
2X10^9/L, N 72.
9%, L 18.
2%; -
Inflammation markers: CRP 6.
8mg/L, ESR 2mm/h; PCT 0.
05ng/ml; -
Biochemistry: normal range of liver function, creatinine102 μmol/L;
-
Autoantibody: ANA 1:100, the others are negative;
-
G test, GM test, cryptococcal capsular antigen: negative;
-
Blood EBV/CMV DNA and IgM antibodies: all negative;
-
Cellular immune examination: CD4/CD8 1.
3; CD4+ T lymphocyte absolute count 1052cells/uL; -
Tumor markers: all negative;
Blood routine: WBC 8.
2X10^9/L, N 72.
9%, L 18.
2%;
Blood routine: WBC 8.
2X10^9/L, N 72.
9%, L 18.
2%;
Inflammation markers: CRP 6.
8mg/L, ESR 2mm/h; PCT 0.
05ng/ml;
Inflammation markers: CRP 6.
8mg/L, ESR 2mm/h; PCT 0.
05ng/ml;
Biochemistry: normal range of liver function, creatinine 102 μmol/L;
Biochemistry: normal range of liver function, creatinine 102 μmol/L;
102Autoantibody: ANA 1:100, the others are negative;
Autoantibody: ANA 1:100, the others are negative;
G test, GM test, cryptococcal capsular antigen: negative;
G test, GM test, cryptococcal capsular antigen: negative;
Blood EBV/CMV DNA and IgM antibodies: all negative;
Blood EBV/CMV DNA and IgM antibodies: all negative;
Cellular immune examination: CD4/CD8 1.
3; CD4+ T lymphocyte absolute count 1052cells/uL;
Cellular immune examination: CD4/CD8 1.
3; CD4+ T lymphocyte absolute count 1052cells/uL;
Tumor markers: all negative;
Tumor markers: all negative;
3.
Clinical analysis
Clinical analysis
Medical history features : middle-aged male, after allogeneic kidney transplantation, long-term use of immunosuppressive agents and glucocorticoids, physical examination revealed lung nodules and admitted to the hospital in January, re-examination of chest CT lung lesions increased in the short term, and the original nodule lesions gradually increased
.
Check the white blood cell count, inflammatory markers and cryptococcus, TSPOT.
TB, G test, etc.
all showed no abnormalities
.
Based on the current data, the reasons are as follows:
-
Community-acquired pneumonia : Physical examination found irregular nodules in the left lower lung with exudative foci.
Common community-acquired pneumonia should be considered.
Infectious pathogens include Streptococcus pneumoniae, Staphylococcus aureus, Klebsiella pneumoniae, Mycoplasma, Chlamydia, etc.
However, the patient has no toxic symptoms such as chills and fever and respiratory symptoms such as cough and sputum.
The white blood cell count and inflammatory markers are all normal.
The CT scan at intervals of more than one month shows that the lesion is only slightly enlarged.
These characteristics are inconsistent with ordinary community-acquired pneumonia.
. -
Special pathogen infection after solid organ transplantation : 1 year after kidney transplantation, regular anti-rejection drugs are being used
.
The physical examination found irregular lung nodules or patchy lesions.
Re-examination at 34 days interval showed that the lesions were enlarged without fever and respiratory symptoms.
It is necessary to consider the possibility of opportunistic infections after transplantation, especially special pathogens with low virulence.
, Including Mycobacterium, Nocardia, Cryptococcus, Aspergillus and some rare fungi
.
Consider sending a lung biopsy at the lesion for etiological and histopathological examination to confirm the diagnosis
. -
Neoplastic diseases : In immunosuppressed populations, high-density shadows in the lungs occur, and the possibility of tumors needs to be considered
.
However, for the newly-emerged lesions 1 year after the operation, and the follow-up CT in a short period of time (1 month interval), compared with the tumor, the lesions seem to increase too quickly, and the disease may be small
.
Community-acquired pneumonia : Physical examination found irregular nodules in the left lower lung with exudative foci.
Common community-acquired pneumonia should be considered.
Infectious pathogens include Streptococcus pneumoniae, Staphylococcus aureus, Klebsiella pneumoniae, Mycoplasma, Chlamydia, etc.
However, the patient has no toxic symptoms such as chills and fever and respiratory symptoms such as cough and sputum.
The white blood cell count and inflammatory markers are all normal.
The CT scan at intervals of more than one month shows that the lesion is only slightly enlarged.
These characteristics are inconsistent with ordinary community-acquired pneumonia.
.
Community-acquired pneumonia : Physical examination found irregular nodules in the left lower lung with exudative foci.
Common community-acquired pneumonia should be considered.
Infectious pathogens include Streptococcus pneumoniae, Staphylococcus aureus, Klebsiella pneumoniae, Mycoplasma, Chlamydia, etc.
However, the patient has no toxic symptoms such as chills and fever and respiratory symptoms such as cough and sputum.
The white blood cell count and inflammatory markers are all normal.
The CT scan at intervals of more than one month shows that the lesion is only slightly enlarged.
These characteristics are inconsistent with ordinary community-acquired pneumonia.
.
Special pathogen infection after solid organ transplantation : 1 year after kidney transplantation, regular anti-rejection drugs are being used
.
The physical examination found irregular lung nodules or patchy lesions.
Re-examination at 34 days interval showed that the lesions were enlarged without fever and respiratory symptoms.
It is necessary to consider the possibility of opportunistic infections after transplantation, especially special pathogens with low virulence.
, Including Mycobacterium, Nocardia, Cryptococcus, Aspergillus and some rare fungi
.
Consider sending a lung biopsy at the lesion for etiological and histopathological examination to confirm the diagnosis
.
Special pathogen infection after solid organ transplantation : 1 year after kidney transplantation, regular anti-rejection drugs are being used
.
The physical examination found irregular lung nodules or patchy lesions.
Re-examination at 34 days interval showed that the lesions were enlarged without fever and respiratory symptoms.
It is necessary to consider the possibility of opportunistic infections after transplantation, especially special pathogens with low virulence.
, Including Mycobacterium, Nocardia, Cryptococcus, Aspergillus and some rare fungi
.
Consider sending a lung biopsy at the lesion for etiological and histopathological examination to confirm the diagnosis
.
Neoplastic diseases : In immunosuppressed populations, high-density shadows in the lungs occur, and the possibility of tumors needs to be considered
.
However, for the newly-emerged lesions 1 year after the operation, and the follow-up CT in a short period of time (1 month interval), compared with the tumor, the lesions seem to increase too quickly, and the disease may be small
.
Neoplastic diseases : In immunosuppressed populations, high-density shadows in the lungs occur, and the possibility of tumors needs to be considered
.
However, for the newly-emerged lesions 1 year after the operation, and the follow-up CT in a short period of time (1 month interval), compared with the tumor, the lesions seem to increase too quickly, and the disease may be small
.
Fourth, further examination, diagnosis and treatment process and treatment response
Fourth, further examination, diagnosis and treatment process and treatment response-
On April 24, 2021, CT-guided percutaneous lung biopsy will be performed, pathology, routine microbiological examination, and pathogen metagenomic sequencing (mNGS) will be performed
. -
2021-04-25 Preliminary pathology: hyperplasia of fibrous tissue, scattered lymphocytes and plasma cells infiltration, a small amount of hyperplasia of alveolar epithelium can be seen
. -
2021-04-26 Lung tissue mNGS: 85 nucleic acid sequences of Talaromyces marneffei were detected
. -
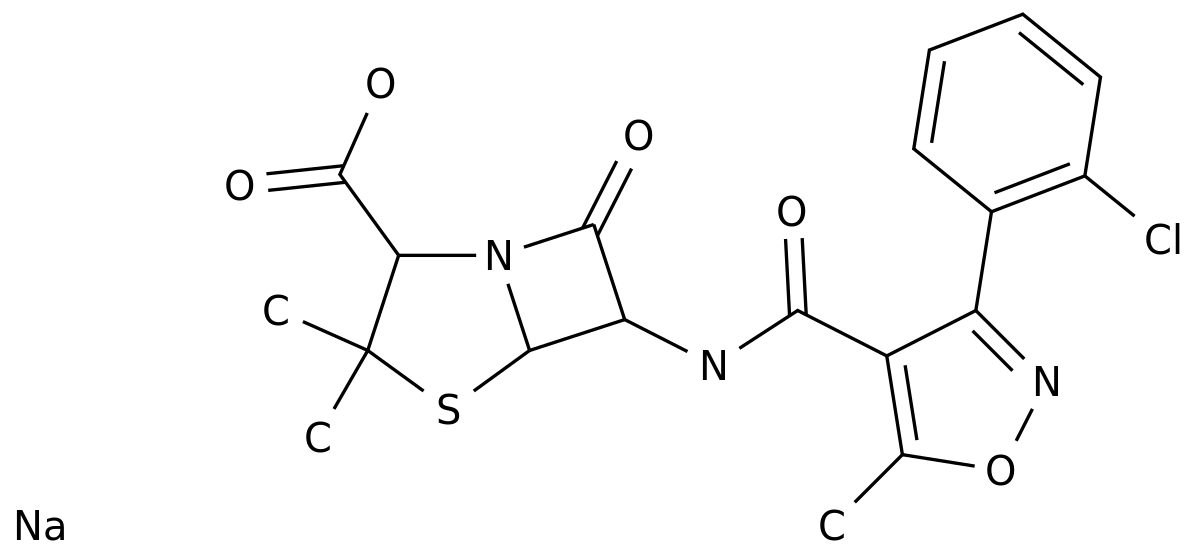
2021-04-27 Considering that the infection of Talaromyces marneffei may be large, due to the status of the patient's kidney transplantation, amphotericin B is not considered for the time being, and voriconazole 200mg q12h ivgtt (first dose of 400mg load) is given
. -
2021-04-30 Peripheral blood mNGS (04-28 sampling): 9 nucleic acid sequences of Talaromyces marneffei were detected
.
On April 24, 2021, CT-guided percutaneous lung biopsy will be performed, pathology, routine microbiological examination, and pathogen metagenomic sequencing (mNGS) will be performed
.
On April 24, 2021, CT-guided percutaneous lung biopsy will be performed, pathology, routine microbiological examination, and pathogen metagenomic sequencing (mNGS) will be performed
.
2021-04-25 Preliminary pathology: hyperplasia of fibrous tissue, scattered lymphocytes and plasma cells infiltration, a small amount of hyperplasia of alveolar epithelium can be seen
.
2021-04-25 Preliminary pathology: hyperplasia of fibrous tissue, scattered lymphocytes and plasma cells infiltration, a small amount of hyperplasia of alveolar epithelium can be seen
.
2021-04-26 Lung tissue mNGS: 85 nucleic acid sequences of Talaromyces marneffei were detected
.
2021-04-26 Lung tissue mNGS: 85 nucleic acid sequences of Talaromyces marneffei were detected
.
2021-04-27 Considering that the infection of Talaromyces marneffei may be large, due to the status of the patient's kidney transplantation, amphotericin B is not considered for the time being, and voriconazole 200mg q12h ivgtt (first dose of 400mg load) is given
.
2021-04-27 Considering that the infection of Talaromyces marneffei may be large, due to the status of the patient's kidney transplantation, amphotericin B is not considered for the time being, and voriconazole 200mg q12h ivgtt (first dose of 400mg load) is given
.
2021-04-30 Peripheral blood mNGS (04-28 sampling): 9 nucleic acid sequences of Talaromyces marneffei were detected
.
2021-04-30 Peripheral blood mNGS (04-28 sampling): 9 nucleic acid sequences of Talaromyces marneffei were detected
.
-
2021-04-30 Measure the blood concentration of tacrolimus: 15.
6ng/mL, considering the drug interaction between voriconazole and tacrolimus, adjust the tacrolimus dose to 0.
25mg q12h, and monitor the blood concentration at 6 -7ng/mL; -
2021-04-30 trough blood concentration of chavoriconazole: 3.
0mg/L (reference value 1.
0-5.
5mg/L), continue with voriconazole 200mg q12h, then monitor the blood concentration at 2-3mg/L; -
On May 10, 2021, he was discharged from the hospital, and continued with voriconazole 200mg q12h po, and regularly monitored the blood concentration and liver and kidney function
. -
Supplementary report on lung histopathology on May 11, 2021: special stain + negative enzyme label
.
Lung tissue bacteria, fungi, and mycobacteria culture successively returned: all negative
. -
Regular follow-up in the outpatient department, monitoring of CRP, erythrocyte sedimentation rate, liver and kidney function, etc.
, showed no obvious abnormalities, and the blood concentrations of voriconazole and tacrolimus were stable and up to standard
.
Re-examination of lung CT on 2021-05-24 and 2021-07-02 respectively showed that the left lower lung lesion was gradually absorbed than before
.
It is still under treatment and follow-up
.
2021-04-30 Measure the blood concentration of tacrolimus: 15.
6ng/mL, considering the drug interaction between voriconazole and tacrolimus, adjust the tacrolimus dose to 0.
25mg q12h, and monitor the blood concentration at 6 -7ng/mL;
2021-04-30 Measure the blood concentration of tacrolimus: 15.
6ng/mL, considering the drug interaction between voriconazole and tacrolimus, adjust the tacrolimus dose to 0.
25mg q12h, and monitor the blood concentration at 6 -7ng/mL;
2021-04-30 trough blood concentration of chavoriconazole: 3.
0mg/L (reference value 1.
0-5.
5mg/L), continue with voriconazole 200mg q12h, then monitor the blood concentration at 2-3mg/L;
2021-04-30 trough blood concentration of chavoriconazole: 3.
0mg/L (reference value 1.
0-5.
5mg/L), continue with voriconazole 200mg q12h, then monitor the blood concentration at 2-3mg/L;
On May 10, 2021, he was discharged from the hospital, and continued with voriconazole 200mg q12h po, and regularly monitored the blood concentration and liver and kidney function
.
On May 10, 2021, he was discharged from the hospital, and continued with voriconazole 200mg q12h po, and regularly monitored the blood concentration and liver and kidney function
.
Supplementary report on lung histopathology on May 11, 2021: special stain + negative enzyme label
.
Lung tissue bacteria, fungi, and mycobacteria culture successively returned: all negative
.
Supplementary report on lung histopathology on May 11, 2021: special stain + negative enzyme label
.
Lung tissue bacteria, fungi, and mycobacteria culture successively returned: all negative
.
Regular follow-up in the outpatient department, monitoring of CRP, erythrocyte sedimentation rate, liver and kidney function, etc.
, showed no obvious abnormalities, and the blood concentrations of voriconazole and tacrolimus were stable and up to standard
.
Re-examination of lung CT on 2021-05-24 and 2021-07-02 respectively showed that the left lower lung lesion was gradually absorbed than before
.
It is still under treatment and follow-up
.
Regular follow-up in the outpatient department, monitoring of CRP, erythrocyte sedimentation rate, liver and kidney function, etc.
, showed no obvious abnormalities, and the blood concentrations of voriconazole and tacrolimus were stable and up to standard
.
Re-examination of lung CT on 2021-05-24 and 2021-07-02 respectively showed that the left lower lung lesion was gradually absorbed than before
.
It is still under treatment and follow-up
.
Five, the final diagnosis and diagnosis basis
Five, the final diagnosis and diagnosis basisFinal diagnosis:
Final diagnosis:-
Talaromyces marneffei lung infection
-
Postoperative status of allogeneic kidney transplantation
Talaromyces marneffei lung infection
Talaromyces marneffei lung infection
Postoperative status of allogeneic kidney transplantation
Postoperative status of allogeneic kidney transplantation
Diagnose based on:
Diagnose based on:
6.
Experience and experience
Experience and experience
-
The general rule of the distribution of common pathogens infected after solid organ transplantation is: as the postoperative time increases, from surgery-related and hospital-acquired infections, transition to latent infection and reactivation (such as Epstein-Barr virus, cytomegalovirus, etc.
) and Opportunistic infections, including Pneumocystis, Mycobacterium, Nocardia, Toxoplasma gondii, Cryptococcus, and some endemic fungi
.
It is often a relatively rare pathogen or mixed infection, which is prone to clinical omissions
.
For example, Talaromyces marneffei has been more common in patients with advanced AIDS in the past, and reported relatively rarely in transplant patients
.
When it involves the lungs, the lesions can appear in many forms on imaging, such as consolidation, ground glass changes, grid-like nodules, diffuse alveolar infiltration, pleural effusion, hilar/mediastinal lymphadenopathy, etc.
, Even cavitary lesions and mass shadows, there is no specificity, which increases the difficulty of diagnosis and identification, and requires precise pathogenic detection
. -
The diagnostic methods of infectious diseases are limited by their respective detection characteristics and sensitivity, so microbiological examination, pathology, genetic testing, etc.
can complement each other to increase the positive rate of diagnosis.
In this case, there is no clear indication in routine microbial detection and pathology.
Next, mNGS provides an important basis for pathogenic diagnosis
. -
The treatment is mainly based on the experience of HIV patients.
For mild patients, itraconazole is the first choice.
For moderate and severe patients, amphotericin B is the first choice for intensive treatment for 2 weeks, followed by itraconazole for consolidation for 10 weeks; for amphotericin intolerance For patients with B, voriconazole can also be administered intravenously for 2 weeks, followed by oral administration for 10 weeks
.
Clinically, individualized treatment courses should be formulated according to the patient's condition, immunosuppressive basis, and the possibility of recurrence.
If necessary, prolonged maintenance treatment can be carried out until immune reconstitution
.
The patient’s outpatient follow-up lung CT showed that the lesions had improved significantly, but the course of antifungal treatment was appropriately prolonged due to incomplete absorption
. -
This patient was a mild patient after kidney transplantation, so azole drugs were chosen for anti-infection treatment, and voriconazole was chosen for reasons of drug availability
.
The pharmacokinetics of voriconazole is non-linear, and it is mainly metabolized by liver cytochrome P450 isoenzymes (CYP2C19, CYP2C9 and CYP3A4), while about 15-20% of Asians are low-metabolized
.
Therefore, therapeutic drug monitoring (TDM) is recommended especially for patients with liver insufficiency, low metabolism, poor curative effect, or toxic reactions
.
At the same time, voriconazole itself is also a cytochrome P450 inhibitor.
The patient has been taking the immunosuppressant tacrolimus (which belongs to the cytochrome 3A enzyme system metabolism) for a long time.
The external hospital test indicated that the patient was "tacrolimus-low metabolite".
, The application of voriconazole is likely to further inhibit the metabolism of tacrolimus
.
Therefore, we closely monitored the two drugs for TDM, and reduced the dose of tacrolimus to 0.
25 mg bid according to the drug concentration, while the blood concentration of voriconazole also reached a steady state, and the anti-Talaromyces marneffei effect was good, and no obvious renal transplantation was found.
Adverse reactions
.
The general rule of the distribution of common pathogens infected after solid organ transplantation is: as the postoperative time increases, from surgery-related and hospital-acquired infections, transition to latent infection and reactivation (such as Epstein-Barr virus, cytomegalovirus, etc.
) and Opportunistic infections, including Pneumocystis, Mycobacterium, Nocardia, Toxoplasma gondii, Cryptococcus, and some endemic fungi
.
It is often a relatively rare pathogen or mixed infection, which is prone to clinical omissions
.
For example, Talaromyces marneffei has been more common in patients with advanced AIDS in the past, and reported relatively rarely in transplant patients
.
When it involves the lungs, the lesions can appear in many forms on imaging, such as consolidation, ground glass changes, grid-like nodules, diffuse alveolar infiltration, pleural effusion, hilar/mediastinal lymphadenopathy, etc.
, Even cavitary lesions and mass shadows, there is no specificity, which increases the difficulty of diagnosis and identification, and requires precise pathogenic detection
.
The general rule of the distribution of common pathogens infected after solid organ transplantation is: as the postoperative time increases, from surgery-related and hospital-acquired infections, transition to latent infection and reactivation (such as Epstein-Barr virus, cytomegalovirus, etc.
) and Opportunistic infections, including Pneumocystis, Mycobacterium, Nocardia, Toxoplasma gondii, Cryptococcus, and some endemic fungi
.
It is often a relatively rare pathogen or mixed infection, which is prone to clinical omissions
.
For example, Talaromyces marneffei has been more common in patients with advanced AIDS in the past, and reported relatively rarely in transplant patients
.
When it involves the lungs, the lesions can appear in many forms on imaging, such as consolidation, ground glass changes, grid-like nodules, diffuse alveolar infiltration, pleural effusion, hilar/mediastinal lymphadenopathy, etc.
, Even cavitary lesions and mass shadows, there is no specificity, which increases the difficulty of diagnosis and identification, and requires precise pathogenic detection
.
The diagnostic methods of infectious diseases are limited by their respective detection characteristics and sensitivity, so microbiological examination, pathology, genetic testing, etc.
can complement each other to increase the positive rate of diagnosis.
In this case, there is no clear indication in routine microbial detection and pathology.
Next, mNGS provides an important basis for pathogenic diagnosis
.
The diagnostic methods of infectious diseases are limited by their respective detection characteristics and sensitivity, so microbiological examination, pathology, genetic testing, etc.
can complement each other to increase the positive rate of diagnosis.
In this case, there is no clear indication in routine microbial detection and pathology.
Next, mNGS provides an important basis for pathogenic diagnosis
.
The treatment is mainly based on the experience of HIV patients.
For mild patients, itraconazole is the first choice.
For moderate and severe patients, amphotericin B is the first choice for intensive treatment for 2 weeks, followed by itraconazole for consolidation for 10 weeks; for amphotericin intolerance For patients with B, voriconazole can also be administered intravenously for 2 weeks, followed by oral administration for 10 weeks
.
Clinically, individualized treatment courses should be formulated according to the patient's condition, immunosuppressive basis, and the possibility of recurrence.
If necessary, prolonged maintenance treatment can be carried out until immune reconstitution
.
The patient’s outpatient follow-up lung CT showed that the lesions had improved significantly, but the course of antifungal treatment was appropriately prolonged due to incomplete absorption
.
The treatment is mainly based on the experience of HIV patients.
For mild patients, itraconazole is the first choice.
For moderate and severe patients, amphotericin B is the first choice for intensive treatment for 2 weeks, followed by itraconazole for consolidation for 10 weeks; for amphotericin intolerance For patients with B, voriconazole can also be administered intravenously for 2 weeks, followed by oral administration for 10 weeks
.
Clinically, individualized treatment courses should be formulated according to the patient's condition, immunosuppressive basis, and the possibility of recurrence.
If necessary, prolonged maintenance treatment can be carried out until immune reconstitution
.
The patient’s outpatient follow-up lung CT showed that the lesions had improved significantly, but the course of antifungal treatment was appropriately prolonged due to incomplete absorption
.
This patient was a mild patient after kidney transplantation, so azole drugs were chosen for anti-infection treatment, and voriconazole was chosen for reasons of drug availability
.
The pharmacokinetics of voriconazole is non-linear, and it is mainly metabolized by liver cytochrome P450 isoenzymes (CYP2C19, CYP2C9 and CYP3A4), while about 15-20% of Asians are low-metabolized
.
Therefore, therapeutic drug monitoring (TDM) is recommended especially for patients with liver insufficiency, low metabolism, poor curative effect, or toxic reactions
.
At the same time, voriconazole itself is also a cytochrome P450 inhibitor.
The patient has been taking the immunosuppressant tacrolimus (which belongs to the cytochrome 3A enzyme system metabolism) for a long time.
The external hospital test indicated that the patient was "tacrolimus-low metabolite".
, The application of voriconazole is likely to further inhibit the metabolism of tacrolimus
.
Therefore, we closely monitored the two drugs for TDM, and reduced the dose of tacrolimus to 0.
25 mg bid according to the drug concentration, while the blood concentration of voriconazole also reached a steady state, and the anti-Talaromyces marneffei effect was good, and no obvious renal transplantation was found.
Adverse reactions
.
This patient was a mild patient after kidney transplantation, so azole drugs were chosen for anti-infection treatment, and voriconazole was chosen for reasons of drug availability
.
The pharmacokinetics of voriconazole is non-linear, and it is mainly metabolized by liver cytochrome P450 isoenzymes (CYP2C19, CYP2C9 and CYP3A4), while about 15-20% of Asians are low-metabolized
.
Therefore, therapeutic drug monitoring (TDM) is recommended especially for patients with liver insufficiency, low metabolism, poor curative effect, or toxic reactions
.
At the same time, voriconazole itself is also a cytochrome P450 inhibitor.
The patient has been taking the immunosuppressant tacrolimus (which belongs to the cytochrome 3A enzyme system metabolism) for a long time.
The external hospital test indicated that the patient was "tacrolimus-low metabolite".
, The application of voriconazole is likely to further inhibit the metabolism of tacrolimus
.
Therefore, we closely monitored the two drugs for TDM, and reduced the dose of tacrolimus to 0.
25 mg bid according to the drug concentration, while the blood concentration of voriconazole also reached a steady state, and the anti-Talaromyces marneffei effect was good, and no obvious renal transplantation was found.
Adverse reactions
.
references
references[1] Harrison Infection (First Chinese Edition), 2019
[1] Harrison Infection (First Chinese Edition), 2019[2] Chan JF, et al.
Talaromyces (Penicillium) marneffei infection in non-HIV-infected patients.
Emerg Microbes Infect.
2016 Mar 9;5(3)
Talaromyces (Penicillium) marneffei infection in non-HIV-infected patients.
Emerg Microbes Infect.
2016 Mar 9;5(3)
[3] Chen Ken et al.
Interpretation of "Guide to Individualized Voriconazole Medication" [J].
Journal of Clinical Drug Therapy, 2019, 17(03)
Interpretation of "Guide to Individualized Use of Voriconazole" [J].
Journal of Clinical Drug Therapy, 2019, 17 (03) Interpretation,
leave a message here