-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
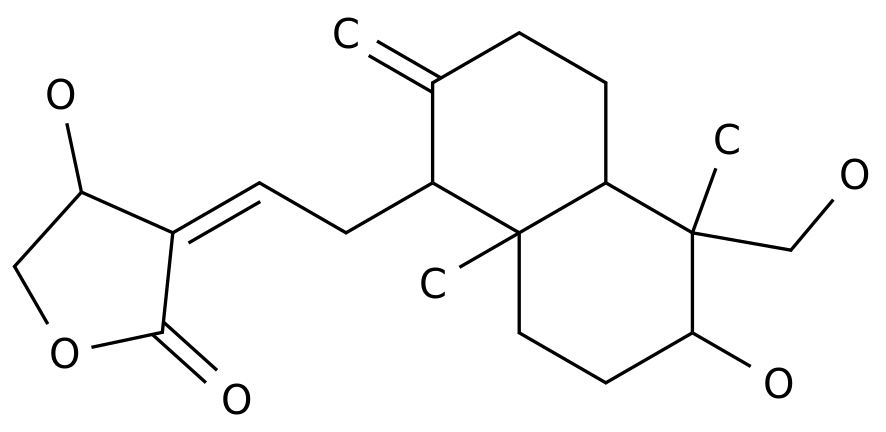
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
For Medical Professionals Only, 4 Antibiotic Options for Gram-Negative Drug-Resistant Infections Currently, the rising antimicrobial resistance remains a deadly problem that threatens global health
.
In clinical practice, how to select effective antibiotics to treat drug-resistant pathogen infections is still a challenging topic
.
Recently, the European Society for Clinical Microbiology and Infectious Diseases (ESCMID) proposed new guidelines for the treatment of third-generation cephalosporin-resistant Enterobacteriaceae (3GCephRE) and carbapenem-resistant Gram-negative bacteria (CRE).
Recommendations, focusing on the effectiveness of antibiotic combination therapy versus monotherapy
.
Jie Xiaoyao will analyze and interpret the guide with you.
The article is highly professional and full of dry goods.
It is recommended to read it after collection
.
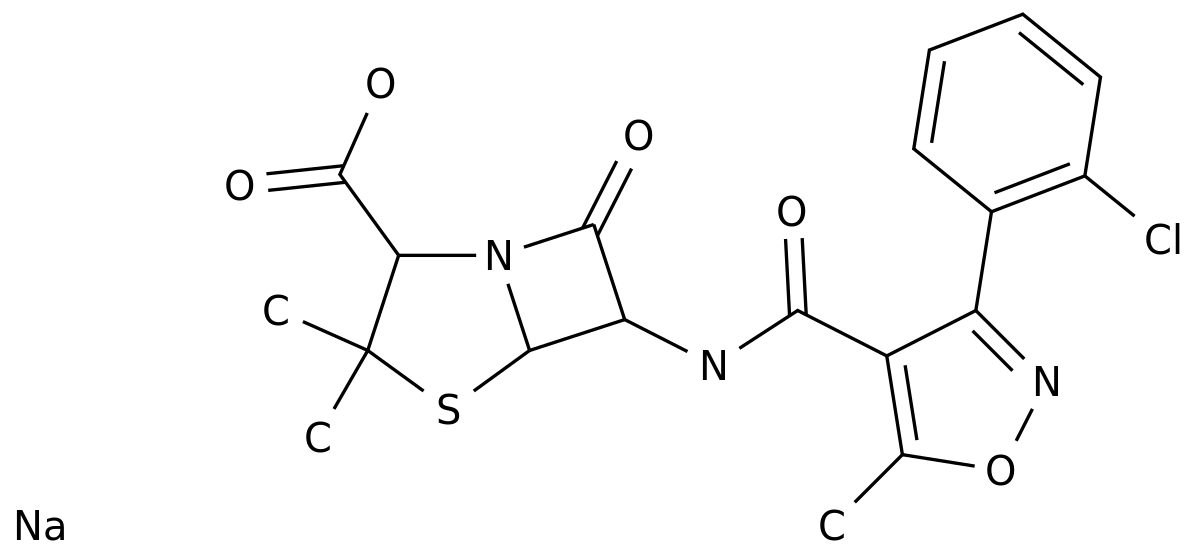
A third-generation cephalosporin-resistant Enterobacteriaceae In recent years, with the widespread clinical application of third-generation cephalosporins, extended-spectrum β-lactamase-resistant Enterobacteriaceae (3GCephRE) has emerged , 3GCephRE often has multi-drug resistance, low sensitivity to commonly used antibiotics, difficult to select therapeutic drugs
.
3Which antibiotic should be chosen for GCephRE infection? ESCMID proposed the following 8 points for antibiotic selection for 3GCephRE infection: 1) For patients with bloodstream infections (BSIs) and serious infections: carbapenems (imipenem, or meropenem) are recommended (strong recommendation, Moderate level of evidence)
.
2) Patients with bloodstream infection but no septic shock: Ertapenem is recommended, but not imipenem or meropenem (conditional recommendation, moderate-quality evidence)
.
3) Low-risk, non-severe infection patients: Piperacillin/tazobactam, amoxicillin/clavulanate or quinolones are recommended (conditional recommendation, moderate level of evidence/good practice statement)
.
For non-severe complicated urinary tract infection (cUTI), compound sulfamethoxazole tablets are recommended
.
(Statement of Good Practice)
.
4) For cUTI patients without septic shock: short-term treatment with aminoglycosides (with in vitro activity) (conditional recommendation, moderate level of evidence/good practice statement), or intravenous fosfomycin (strong recommendation, evidence high grade)
.
5) Tigecycline is not recommended (strong recommendation, very low level of evidence)
.
6) Among all 3GCephRE-infected patients, novel β-lactam/β-lactamase inhibitors (BLBLIs) are reserve antibiotics for extensively drug-resistant bacteria, so for antibiotic stewardship considerations, the use of these drugs to treat 3GCephRE-induced infections should be avoided.
infection (good practice statement, expert opinion)
.
7) Cephamycin antibiotics (such as cefoxitin, cefmetazole, fluoxetine) and cefepime are not recommended for the treatment of 3GCephRE infection (conditional recommendation, very low level of evidence)
.
8) There is insufficient evidence to support cefoperazone/sulbactam, ampicillin/sulbactam, ticarcillin/clavulanate, temoxicillin and mecillin for the treatment of patients with 3GCephRE infection (no recommendation)
.
No combination drug therapy is recommended! Carbapenem-resistant Enterobacteriaceae (CRE) is a type of bacterial infection that has gradually increased in clinical frequency in recent years, and has even spread to become a global public health problem.
The cause of this problem is largely the abuse of antibiotics
.
Which antibiotic should be chosen for CRE infection? ESCMID put forward the following 5 points for the selection of antibiotics for CRE infection: 1) For patients with severe infection, if they have in vitro activity, meropenem-faborbactam or ceftazidime-avibactam are recommended (conditional recommendation, evidence level respectively medium or low)
.
2) Cefdil (with Conditional recommendation, low level of evidence)
.
3) For patients with non-serious infections caused by CRE, an antibiotic with in vitro activity should be selected based on the patient's individual basis and source of infection (Good Practice Statement)
.
For patients with cUTI, aminoglycosides, including prazomicin, rather than tigecycline are recommended (conditional recommendation, low-quality evidence)
.
4) Tigecycline is not recommended for the treatment of BSIs and hospital-acquired pneumonia/ventilator-associated pneumonia (HAP/VAP); if necessary, for patients with pneumonia, clinicians can use high-dose tigecycline (conditionally not recommended).
use, low level of evidence)
.
5) There is no evidence for or against the use of imipenem-relebactam and fosfomycin monotherapy for CRE
.
Are CRE Infections Using Combination Therapy? For the combined treatment regimen of CRE infection, the ESCMI guidelines propose the following 5 points: 1) For CRE infection and sensitive to ceftazidime-avibactam, meropenem-faborbactam or cefdil and receiving the above drugs, no Combination therapy is recommended (strong recommendation, low-quality evidence)
.
2) For patients with severe infection caused by metallo-beta-lactamase-producing CRE and/or resistance to novel antibiotic monotherapy, aztreonam combined with ceftazidime-avibactam is recommended (conditional recommendation, moderate evidence level)
.
3) For severe CRE infections that are only sensitive to polymyxins, aminoglycosides, tigecycline, or fosfomycin in vitro, or in the absence of novel BLBLs, the use of more than one in vitro sensitive drug (conditional) is recommended.
recommendation, moderate grade of evidence)
.
There are no specific drug combinations recommended or opposed
.
4) For CRE-infected patients, clinicians are advised to avoid the use of carbapenem-based combination therapy (conditionally not recommended, low level of evidence), unless the MIC of meropenem is ≤8 mg/L, in the absence of novel BLBLIs, High-dose prolonged infusion of meropenem may be used as part of combination therapy (conditional recommendation, low-quality evidence)
.
5) For patients with non-severe infections or at low risk of CRE infection, among older antibiotics with in vitro activity, when considering antibiotic stewardship, choose monotherapy based on the individual patient base and source of infection (good practice statement)
.
Three carbapenem Pseudomonas aeruginosa Pseudomonas aeruginosa is a non-fermenting gram-negative bacilli, major pathogens of nosocomial infections also can cause respiratory, urinary tract, bloodstream infections
.
Carbapenems are potent beta-lactam drugs for the treatment of Pseudomonas aeruginosa infections and are among the most effective
.
However, in recent years, with the widespread use of carbapenem antibiotics, carbapenem-resistant Pseudomonas aeruginosa (CRPA) has gradually increased, limiting the choice of anti-infective drugs
.
Which antibiotic should be chosen for CRPA infection? Regarding the choice of antibiotics for CRPA infection, ESCMID put forward the following 5 points this time: 1) For DTR-CRPA (Pseudomonas aeruginosa resistant to β-lactams, enzyme inhibitor compound preparations and quinolones) In patients with severe infections, we suggest treatment with ceftoloza-tazobactam (if effective in vitro) (conditional recommendation, very low-quality evidence)
.
At present, there is insufficient evidence to recommend imipenem-lelibactam, cefadilo and ceftazidime-avibactam
.
2) In non-severe or low-risk CRPA-infected patients, taking antibiotic stewardship into consideration, it is good clinical practice to select older antibiotics with in vitro activity based on individual basis and source of infection (Good Practice Statement)
.
Can combination therapy be used for CRPA infection? The ESCMI guidelines propose the following 3 points for the combined treatment of CRPA infection: 1) We cannot recommend or against the use of new BLBLIs (ceftazidime-avibactam and cefditorozin-tazobactam) or cephalosporins due to lack of evidence Dil for the treatment of CRPA infection
.
2) When using polymyxins, aminoglycosides, or fosfomycin to treat severe infections caused by CRPA, we recommend treatment with two in vitro sensitive drugs (conditional recommendation, low-quality evidence)
.
Can't offer advice for or against a particular combination
.
3) In patients with non-severe infections or low-risk CRPA infections, it is good clinical practice to select antibiotic monotherapy with in vitro activity based on individual basis and source of infection, taking into account antibiotic stewardship (Good Practice Statement)
.
Four carbapenem-resistant Acinetobacter baumannii Acinetobacter baumannii is a non-fermenting gram-negative bacillus, an important pathogen of nosocomial infection, which can cause pneumonia, bacteremia, urinary tract infection and other diseases
.
Carbapenem antibacterial drugs are the main drugs for the treatment of Acinetobacter baumannii, but the application of antibacterial drugs has gradually increased in recent years, resulting in carbapenem-resistant Acinetobacter baumannii (CRAB)
.
Which antibiotic should be chosen for CRAB infection? 1) For HAP/VAP patients with sulbactam-sensitive CRAB, ampicillin-sulbactam is recommended (conditional recommendation, low level of evidence)
.
2) In sulbactam-resistant CRAB patients, polymyxin or high-dose tigecycline can be used if it is effective in vitro
.
The preferred antibiotic cannot be recommended due to lack of evidence
.
3) Cefdil is not recommended for the treatment of infections caused by CRAB (conditional not recommended, low level of evidence)
.
Is Combination Therapy Used for CRAB Infections? 1) For all CRAB-infected patients, we do not recommend polymyxin-meropenem combination therapy (strong recommendation against use; high certainty evidence) or polymyxin-rifampicin combination therapy (strong recommendation against use, moderate level of evidence )
.
2) For patients with severe and high-risk CRAB infection, we recommend a combination therapy that includes two in vitro active antibiotics in the available antibiotics (polymyxin, aminoglycoside, tigecycline, sulbactam combination) (conditional recommended, very low level of evidence)
.
3) For CRAB-infected patients with meropenem MIC < 8 mg/L, a high-dose, extended infusion carbapenem regimen may be considered (good practice statement)
.
Finally, the recommended drug use regimen for Fever (50th edition) recommended drug use regimen for Fever (50th edition) recommended drug use regimen for imipenem/cilastatin: 1.
0 g (0.
5g+0.
5g) iv q6h; for Pseudomonas aeruginosa 2.
0g q8h-q6h meropenem: 0.
5-1.
0g iv q8h, for meningitis it can be increased to 2.
0g iv q8h Ertapenem: 1.
0g iv Or im q24h piperacillin/tazobactam: recommended extended infusion regimen: inject 4.
5g within 30min as a loading dose; after 4h, 3.
375g iv infusion for more than 4h q8h, with intravenous access remaining for more than 12h per day Ming: 960mg po bid; levofloxacin: 250-750mg po/iv qd, for most adaptations, 750mg is the best dose; ciprofloxacin: 400mg iv q12h; uncomplicated urethritis/cystitis, 250mg po bid; Mikacin: 15mg/kg qd; fosfomycin: osteomyelitis, complicated urinary tract infection, hospital-acquired pneumonia, 12-24g IV daily, divided q8-12h; meningitis, 16-24g divided daily q6~8h; Meropenem-Fabronbactam: 4g (2g+2g) iv q8h infusion for 3h; Ceftazidime-avibactam: 2.
5g (2g+0.
5g) iv q8h infusion for 2h; Cefdil: 2g iv q8h infusion for 3h; amikacin: 15mg/kg iv qd; high-dose tigecycline: 200mg for the first time, 100mg iv q12h; aztreonam: 1g-2g iv q6h-q8h; high-dose extended infusion of meropenem : If CrCl ≥50ml/min: 2g q8h (infusion over 3h); if CrCl 30~49ml/min: 1g q8h (infusion over 3h); if CrCl 10~29ml/min: 1g q12h (infusion over 3h) Cefoloza-tazobactam: 1.
5g iv q8h infusion over 1h; Ampicillin/Sulbactam: for the treatment of resistant Acinetobacter, Ampicillin 8g/sulbactam 4g iv q8h infusion over 4h; Polymyxa Primer: Dosage is based on actual body weight, loading dose: 2.
5mg/kg iv (infusion over 2h), maintenance dose: 1.
5mg/kg iv after 12h (infusion over 1h), and then repeat every 12h
.
No dose adjustment is required in patients with renal insufficiency
.
Did this article help you? Please forward it so that more people can see it~ Reference: [1] Paul M, Carrara E, Retamar P, et al.
European Society of clinical microbiology and infectious diseases (ESCMID) guidelines for the treatment of infections caused by Multidrug-resistant Gram-negative bacilli (endorsed by ESICM -European Society of intensive care Medicine).
Clin Microbiol Infect.
2021 Dec 16:S1198-743X(21)00679-0.
doi: 10.
1016/j.
cmi.
2021.
11.
025.
[2] Sanford Guidelines for Antimicrobial Treatment of Fever (50th Edition)
.
In clinical practice, how to select effective antibiotics to treat drug-resistant pathogen infections is still a challenging topic
.
Recently, the European Society for Clinical Microbiology and Infectious Diseases (ESCMID) proposed new guidelines for the treatment of third-generation cephalosporin-resistant Enterobacteriaceae (3GCephRE) and carbapenem-resistant Gram-negative bacteria (CRE).
Recommendations, focusing on the effectiveness of antibiotic combination therapy versus monotherapy
.
Jie Xiaoyao will analyze and interpret the guide with you.
The article is highly professional and full of dry goods.
It is recommended to read it after collection
.
A third-generation cephalosporin-resistant Enterobacteriaceae In recent years, with the widespread clinical application of third-generation cephalosporins, extended-spectrum β-lactamase-resistant Enterobacteriaceae (3GCephRE) has emerged , 3GCephRE often has multi-drug resistance, low sensitivity to commonly used antibiotics, difficult to select therapeutic drugs
.
3Which antibiotic should be chosen for GCephRE infection? ESCMID proposed the following 8 points for antibiotic selection for 3GCephRE infection: 1) For patients with bloodstream infections (BSIs) and serious infections: carbapenems (imipenem, or meropenem) are recommended (strong recommendation, Moderate level of evidence)
.
2) Patients with bloodstream infection but no septic shock: Ertapenem is recommended, but not imipenem or meropenem (conditional recommendation, moderate-quality evidence)
.
3) Low-risk, non-severe infection patients: Piperacillin/tazobactam, amoxicillin/clavulanate or quinolones are recommended (conditional recommendation, moderate level of evidence/good practice statement)
.
For non-severe complicated urinary tract infection (cUTI), compound sulfamethoxazole tablets are recommended
.
(Statement of Good Practice)
.
4) For cUTI patients without septic shock: short-term treatment with aminoglycosides (with in vitro activity) (conditional recommendation, moderate level of evidence/good practice statement), or intravenous fosfomycin (strong recommendation, evidence high grade)
.
5) Tigecycline is not recommended (strong recommendation, very low level of evidence)
.
6) Among all 3GCephRE-infected patients, novel β-lactam/β-lactamase inhibitors (BLBLIs) are reserve antibiotics for extensively drug-resistant bacteria, so for antibiotic stewardship considerations, the use of these drugs to treat 3GCephRE-induced infections should be avoided.
infection (good practice statement, expert opinion)
.
7) Cephamycin antibiotics (such as cefoxitin, cefmetazole, fluoxetine) and cefepime are not recommended for the treatment of 3GCephRE infection (conditional recommendation, very low level of evidence)
.
8) There is insufficient evidence to support cefoperazone/sulbactam, ampicillin/sulbactam, ticarcillin/clavulanate, temoxicillin and mecillin for the treatment of patients with 3GCephRE infection (no recommendation)
.
No combination drug therapy is recommended! Carbapenem-resistant Enterobacteriaceae (CRE) is a type of bacterial infection that has gradually increased in clinical frequency in recent years, and has even spread to become a global public health problem.
The cause of this problem is largely the abuse of antibiotics
.
Which antibiotic should be chosen for CRE infection? ESCMID put forward the following 5 points for the selection of antibiotics for CRE infection: 1) For patients with severe infection, if they have in vitro activity, meropenem-faborbactam or ceftazidime-avibactam are recommended (conditional recommendation, evidence level respectively medium or low)
.
2) Cefdil (with Conditional recommendation, low level of evidence)
.
3) For patients with non-serious infections caused by CRE, an antibiotic with in vitro activity should be selected based on the patient's individual basis and source of infection (Good Practice Statement)
.
For patients with cUTI, aminoglycosides, including prazomicin, rather than tigecycline are recommended (conditional recommendation, low-quality evidence)
.
4) Tigecycline is not recommended for the treatment of BSIs and hospital-acquired pneumonia/ventilator-associated pneumonia (HAP/VAP); if necessary, for patients with pneumonia, clinicians can use high-dose tigecycline (conditionally not recommended).
use, low level of evidence)
.
5) There is no evidence for or against the use of imipenem-relebactam and fosfomycin monotherapy for CRE
.
Are CRE Infections Using Combination Therapy? For the combined treatment regimen of CRE infection, the ESCMI guidelines propose the following 5 points: 1) For CRE infection and sensitive to ceftazidime-avibactam, meropenem-faborbactam or cefdil and receiving the above drugs, no Combination therapy is recommended (strong recommendation, low-quality evidence)
.
2) For patients with severe infection caused by metallo-beta-lactamase-producing CRE and/or resistance to novel antibiotic monotherapy, aztreonam combined with ceftazidime-avibactam is recommended (conditional recommendation, moderate evidence level)
.
3) For severe CRE infections that are only sensitive to polymyxins, aminoglycosides, tigecycline, or fosfomycin in vitro, or in the absence of novel BLBLs, the use of more than one in vitro sensitive drug (conditional) is recommended.
recommendation, moderate grade of evidence)
.
There are no specific drug combinations recommended or opposed
.
4) For CRE-infected patients, clinicians are advised to avoid the use of carbapenem-based combination therapy (conditionally not recommended, low level of evidence), unless the MIC of meropenem is ≤8 mg/L, in the absence of novel BLBLIs, High-dose prolonged infusion of meropenem may be used as part of combination therapy (conditional recommendation, low-quality evidence)
.
5) For patients with non-severe infections or at low risk of CRE infection, among older antibiotics with in vitro activity, when considering antibiotic stewardship, choose monotherapy based on the individual patient base and source of infection (good practice statement)
.
Three carbapenem Pseudomonas aeruginosa Pseudomonas aeruginosa is a non-fermenting gram-negative bacilli, major pathogens of nosocomial infections also can cause respiratory, urinary tract, bloodstream infections
.
Carbapenems are potent beta-lactam drugs for the treatment of Pseudomonas aeruginosa infections and are among the most effective
.
However, in recent years, with the widespread use of carbapenem antibiotics, carbapenem-resistant Pseudomonas aeruginosa (CRPA) has gradually increased, limiting the choice of anti-infective drugs
.
Which antibiotic should be chosen for CRPA infection? Regarding the choice of antibiotics for CRPA infection, ESCMID put forward the following 5 points this time: 1) For DTR-CRPA (Pseudomonas aeruginosa resistant to β-lactams, enzyme inhibitor compound preparations and quinolones) In patients with severe infections, we suggest treatment with ceftoloza-tazobactam (if effective in vitro) (conditional recommendation, very low-quality evidence)
.
At present, there is insufficient evidence to recommend imipenem-lelibactam, cefadilo and ceftazidime-avibactam
.
2) In non-severe or low-risk CRPA-infected patients, taking antibiotic stewardship into consideration, it is good clinical practice to select older antibiotics with in vitro activity based on individual basis and source of infection (Good Practice Statement)
.
Can combination therapy be used for CRPA infection? The ESCMI guidelines propose the following 3 points for the combined treatment of CRPA infection: 1) We cannot recommend or against the use of new BLBLIs (ceftazidime-avibactam and cefditorozin-tazobactam) or cephalosporins due to lack of evidence Dil for the treatment of CRPA infection
.
2) When using polymyxins, aminoglycosides, or fosfomycin to treat severe infections caused by CRPA, we recommend treatment with two in vitro sensitive drugs (conditional recommendation, low-quality evidence)
.
Can't offer advice for or against a particular combination
.
3) In patients with non-severe infections or low-risk CRPA infections, it is good clinical practice to select antibiotic monotherapy with in vitro activity based on individual basis and source of infection, taking into account antibiotic stewardship (Good Practice Statement)
.
Four carbapenem-resistant Acinetobacter baumannii Acinetobacter baumannii is a non-fermenting gram-negative bacillus, an important pathogen of nosocomial infection, which can cause pneumonia, bacteremia, urinary tract infection and other diseases
.
Carbapenem antibacterial drugs are the main drugs for the treatment of Acinetobacter baumannii, but the application of antibacterial drugs has gradually increased in recent years, resulting in carbapenem-resistant Acinetobacter baumannii (CRAB)
.
Which antibiotic should be chosen for CRAB infection? 1) For HAP/VAP patients with sulbactam-sensitive CRAB, ampicillin-sulbactam is recommended (conditional recommendation, low level of evidence)
.
2) In sulbactam-resistant CRAB patients, polymyxin or high-dose tigecycline can be used if it is effective in vitro
.
The preferred antibiotic cannot be recommended due to lack of evidence
.
3) Cefdil is not recommended for the treatment of infections caused by CRAB (conditional not recommended, low level of evidence)
.
Is Combination Therapy Used for CRAB Infections? 1) For all CRAB-infected patients, we do not recommend polymyxin-meropenem combination therapy (strong recommendation against use; high certainty evidence) or polymyxin-rifampicin combination therapy (strong recommendation against use, moderate level of evidence )
.
2) For patients with severe and high-risk CRAB infection, we recommend a combination therapy that includes two in vitro active antibiotics in the available antibiotics (polymyxin, aminoglycoside, tigecycline, sulbactam combination) (conditional recommended, very low level of evidence)
.
3) For CRAB-infected patients with meropenem MIC < 8 mg/L, a high-dose, extended infusion carbapenem regimen may be considered (good practice statement)
.
Finally, the recommended drug use regimen for Fever (50th edition) recommended drug use regimen for Fever (50th edition) recommended drug use regimen for imipenem/cilastatin: 1.
0 g (0.
5g+0.
5g) iv q6h; for Pseudomonas aeruginosa 2.
0g q8h-q6h meropenem: 0.
5-1.
0g iv q8h, for meningitis it can be increased to 2.
0g iv q8h Ertapenem: 1.
0g iv Or im q24h piperacillin/tazobactam: recommended extended infusion regimen: inject 4.
5g within 30min as a loading dose; after 4h, 3.
375g iv infusion for more than 4h q8h, with intravenous access remaining for more than 12h per day Ming: 960mg po bid; levofloxacin: 250-750mg po/iv qd, for most adaptations, 750mg is the best dose; ciprofloxacin: 400mg iv q12h; uncomplicated urethritis/cystitis, 250mg po bid; Mikacin: 15mg/kg qd; fosfomycin: osteomyelitis, complicated urinary tract infection, hospital-acquired pneumonia, 12-24g IV daily, divided q8-12h; meningitis, 16-24g divided daily q6~8h; Meropenem-Fabronbactam: 4g (2g+2g) iv q8h infusion for 3h; Ceftazidime-avibactam: 2.
5g (2g+0.
5g) iv q8h infusion for 2h; Cefdil: 2g iv q8h infusion for 3h; amikacin: 15mg/kg iv qd; high-dose tigecycline: 200mg for the first time, 100mg iv q12h; aztreonam: 1g-2g iv q6h-q8h; high-dose extended infusion of meropenem : If CrCl ≥50ml/min: 2g q8h (infusion over 3h); if CrCl 30~49ml/min: 1g q8h (infusion over 3h); if CrCl 10~29ml/min: 1g q12h (infusion over 3h) Cefoloza-tazobactam: 1.
5g iv q8h infusion over 1h; Ampicillin/Sulbactam: for the treatment of resistant Acinetobacter, Ampicillin 8g/sulbactam 4g iv q8h infusion over 4h; Polymyxa Primer: Dosage is based on actual body weight, loading dose: 2.
5mg/kg iv (infusion over 2h), maintenance dose: 1.
5mg/kg iv after 12h (infusion over 1h), and then repeat every 12h
.
No dose adjustment is required in patients with renal insufficiency
.
Did this article help you? Please forward it so that more people can see it~ Reference: [1] Paul M, Carrara E, Retamar P, et al.
European Society of clinical microbiology and infectious diseases (ESCMID) guidelines for the treatment of infections caused by Multidrug-resistant Gram-negative bacilli (endorsed by ESICM -European Society of intensive care Medicine).
Clin Microbiol Infect.
2021 Dec 16:S1198-743X(21)00679-0.
doi: 10.
1016/j.
cmi.
2021.
11.
025.
[2] Sanford Guidelines for Antimicrobial Treatment of Fever (50th Edition)