-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
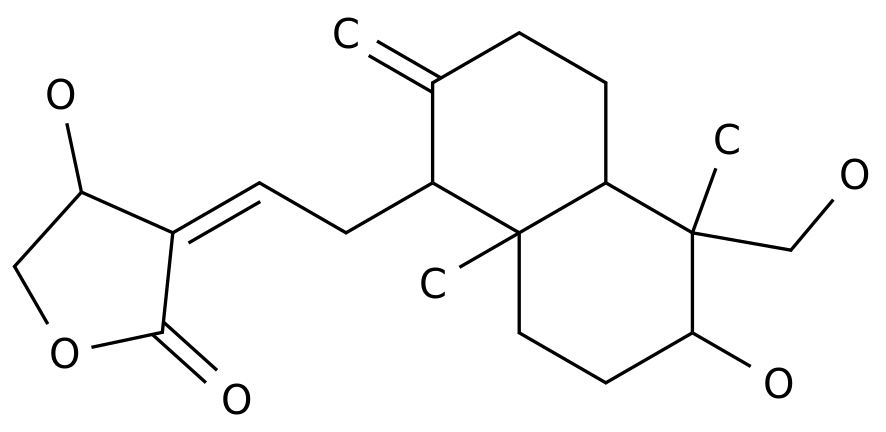
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
-*For medical professionals' reference only, the dosage optimization of new β-lactams and β-lactam/β-lactamase inhibitor antibacterial drugs is an important factor in determining the clinical anti-infective efficacy and the occurrence of drug resistance
.
With carbapenem-resistant Enterobacteriaceae (CRE), carbapenem-resistant Pseudomonas aeruginosa (CRPA), carbapenem-resistant Acinetobacter baumannii (CRAB), and Vanguard With the increase of multi-drug-resistant (MDR) or pan-drug-resistant (XDR) infections represented by enterococcus resistant to mycin (VRE), the types of antimicrobial drugs that can be selected clinically are very limited, and first-line clinicians are stretched out [1,2]
.
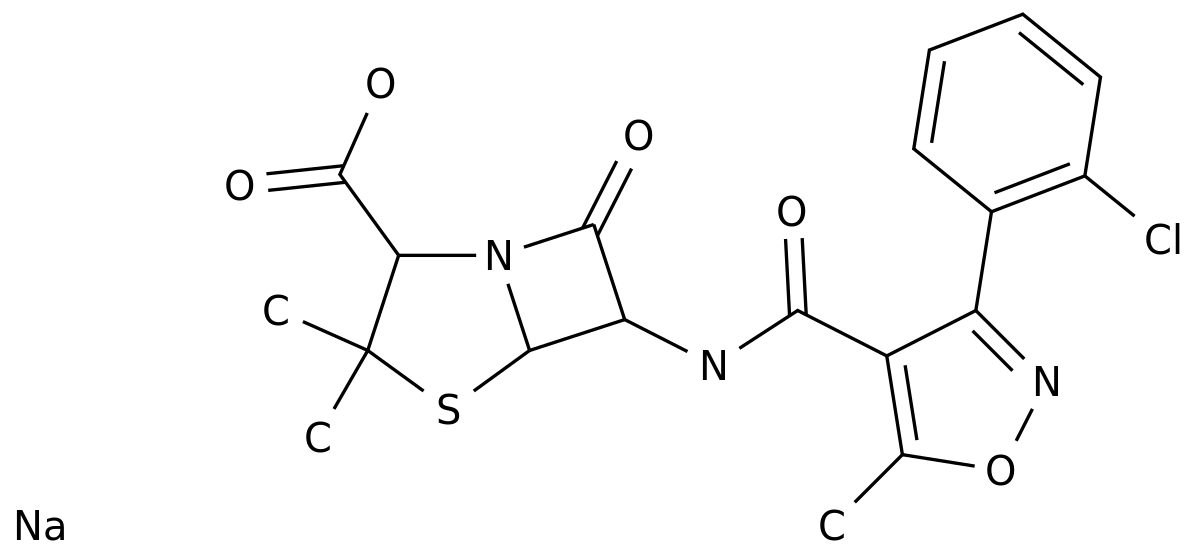
In recent years, several new β-lactams (BLs) and/or β-lactam/β-lactamase inhibitors (BL/BLIs) have been developed and marketed one after another, such as ceftazidime/avibactam, cefothiazide/ Tazobactam, meropenem/wabobactam, imipenem/ribactam and cefiderocol, these drugs have obvious anti-infective effects on a variety of CRE, CRPA, and CRAB [3,4], but in renal function There is no consensus on how to optimize the dose in severely injured patients
.
Milo Gatti & Federico Pea published a review article in Expert Review of Clinical Pharmacology in April 2021, "Pharmacokinetic/pharmacodynamic goals of antimicrobial use in patients with severe renal impairment: focus on new β-lactams and β-lactams/ β-lactamase inhibitors"
.
This article searches the PubMed MEDLINE database for clinical and pharmacokinetic studies published in English before December 2020.
The pharmacokinetics and clinical issues of the application of new BLs and/or BL/BLIs to patients with severe renal insufficiency are carried out.
Elaborating in detail, it is believed that changing the dosing strategy (extended infusion and/or higher dose) and adopting adaptive real-time therapeutic drug monitoring (TDM) may be to ensure the best pharmacokinetics/pharmacodynamics of new BLs and/or BL/BLIs The most effective method to learn the goal can help minimize the risk of clinical anti-infective treatment failure and/or drug resistance
.
Early and appropriate anti-infection treatment can help reduce the mortality of patients with severe infections, and optimizing the administration of antimicrobial drugs plays a key role in it
.
The complex pathophysiological changes in critically ill patients have an important impact on the pharmacokinetics of antibacterial drugs by acting on the apparent volume of distribution and drug clearance rate.
Fluctuations, from enhanced renal clearance (ARC) to acute kidney injury (AKI), lead to inadequate concentrations of antimicrobials in patients with severe infections under conventional dosages.
How to adjust the dosage of antimicrobials to achieve effective antimicrobial exposure is extremely important.
The big challenge
.
BLs and new BL/BLIs antibacterial drugs due to their hydrophilicity, low plasma protein binding rate, low volume of distribution and main renal metabolism and other physical and chemical properties and pharmacokinetic characteristics [5,6], blood drug concentration is very vulnerable to severe illness Patients with complex pathophysiological changes are also more susceptible to continuous renal replacement therapy (CRRT), extracorporeal membrane oxygenation (ECMO) and other continuous renal replacement therapy and extracorporeal life support therapy
.
In addition, BLs are time-dependent antibacterial drugs, and their effectiveness depends on the proportion of time that the plasma concentration is above the minimum inhibitory concentration (MIC).
Clinical data shows that more aggressive pharmacokinetic/pharmacodynamic goals can improve severe illness The prognosis of the patient (such as 100% fT>4-5×MIC)
.
However, so far, due to the lack of large-scale clinical monitoring data for critically ill patients, there is no consensus on how to adjust the dosage and method of antimicrobial drug administration [7].
These will be new BL/BLIs in the future in clinical practice.
Important issues that need to be resolved in the application process
.
1.
The pharmacokinetic characteristics of new BLs and/or BL/BLIs in patients with fluctuating renal function.
The new BLs and BL/BLIs are time-dependent.
MIC percentage of time) related
.
The current evidence shows that the glomerular clearance rate and the drug plasma clearance rate are linearly related, that is, the decrease in drug clearance is directly proportional to the decrease in renal function
.
Therefore, patients with renal insufficiency need to adjust the drug delivery strategy when applying new BLs and BL/BLIs anti-infective treatments
.
For patients with severe renal impairment, it is recommended to use multiple daily doses and prolonged infusion (prolonged dosing time or continuous infusion), which may be the best way to maximize the antibacterial activity of BLs[7,8]
.
Based on the results of existing clinical trials and the available data retrieved from the product description, clinicians may face the following four problems when applying new BLs and BL/BLIs anti-infective treatments to patients with renal insufficiency: A) Extend the infusion time ; B) Maintain a higher daily dose; C) Application in critically ill patients; D) Achieve the PK/PD goal of effective anti-infection and/or reduction of the risk of drug resistance
.
A) Extending the infusion time Extending the infusion time can help improve the anti-infection effect of BLs, reduce the mortality rate, ICU time and hospital stay, and improve the clinical prognosis of patients
.
Studies have confirmed that in the new BLs and BL/BLIs, ceftazidime/avibactam extends the infusion time to 2 hours, meropenem/wabobactam and cefiderocol extend the infusion time to 3 hours, and ceftizidine/tazobac Tan infusion time to 1 hour, imipenem/rapatan infusion for 30 minutes, all help to achieve the best PK/PD goal
.
There is currently no recommendation on whether a loading dose is required
.
It is worth noting that the stability of the aqueous solution is an important issue that needs to be paid attention to whether BLs can extend the infusion time, because it may cause the rapid degradation of antibacterial drugs and lose their anti-infective efficacy
.
The stable time of ceftazidime/avibactam and ceftizidine/tazobactam aqueous solutions at room temperature can reach 24 hours, so it is easy to achieve continuous infusion
.
The stability of the aqueous solution of meropenem at room temperature is limited to 8 hours, which means that continuous infusion can be achieved by reconfiguring the aqueous solution every 6-8 hours and completing the infusion in 6-8 hours
.
The stability of imipenem in aqueous solution does not exceed 3.
5 hours, so it is only suitable for extending the infusion time [9,10]
.
B) Maintaining a higher daily dose of antibacterial drugs for patients with renal insufficiency should be adjusted according to the pharmacodynamics to ensure that the anti-infective target is maximized
.
For new types of BLs and/or BL/BLIs, studies have found that reducing the single dose of antimicrobial drugs while keeping the dosing interval unchanged is the best dosing strategy for maintaining fT>MIC and achieving the maximum PK/PD target.
Drug strategies have been widely used in the anti-infective treatment of patients with renal insufficiency, including end-stage renal disease (ESRD) and intermittent hemodialysis (IHD), including cefiderocol and imipenem/raibactam [(creatinine clearance rate (CLcr ) Is 15-29 ml/min], ceftazidime/tazobactam (CLcr less than 15ml/min), meropenem/wabobactam (CLcr up to 20-39 ml/min) and ceftazidime/avibactam (CLcr up to 31-50 ml/min) The implementation of this strategy is not so strict [11]
.
C) Application in critically ill patients Severely ill patients are high-risk groups of multidrug-resistant infections, new BLs and BL/BLIs are beneficial to severe patients Anti-infective treatment for infected patients
.
Severely ill patients are high-risk groups with impaired renal function (such as IHD, ARC or CRRT).
How to choose an appropriate dosing regimen based on the evaluation of renal function is a huge challenge for clinically effective anti-infective treatment
.
Although both new BLs and BL/BLIs have developed specific dosing regimens for patients receiving IHD, the pharmacokinetics and pharmacodynamics data of severe CRRT patients are still lacking
.
For example, cefiderocol has formulated a dose for CRRT patients, but the dose is calculated based on the clearance rate of cefepime CRRT, because these two BLs have similar characteristics in terms of molecular weight and protein binding rate
.
For ARC patients, currently only cefiderocol has formulated a corresponding intensive dosing regimen, that is, when CLcr>120ml/min, 2g every 6 hours, infusion time>3h, no other new BLs and/or BL/BLIs are administered.
Suggest
.
D) Achieve effective anti-infection and/or reduce the risk of drug resistance PK/PD target laboratory research data shows that fT>MIC between 40%-70% can basically guarantee the bactericidal effect of BLs, new BLs and/or BL/ The results of phase II and phase III clinical trials of BLIs suggest that the conventional dose can achieve this PK/PD goal
.
However, actual clinical anti-infection data show that if a more aggressive PK/PD goal is achieved, that is, 100% fT>4-5×MIC, it will not only help improve the clinical outcome of patients with severe infections, but also help reduce bacterial resistance.
Happened
.
Of course, in the face of these more radical PK/PD goals, there is currently no research data on new BLs and/or BL/BLIs, but how to achieve higher PK/PD goals may be inevitable in the future clinical application of these drugs.
The important challenge [12,13]
.
2.
Application adjustment of new BLs and/or BL/BLIs in different types of kidney diseases 1 How to optimize the dose of BLs for patients with AKI sepsis-related AKI is an important topic
.
The current recommended doses of antibacterial drugs for patients with renal insufficiency are usually based on the results of a phase I clinical study in subjects with stable chronic renal impairment, and are not suitable for patients with septic AKI
.
The renal function of many critically ill patients, especially those with sepsis and septic shock, changes over time and the course of the disease.
AKI induced by initial infection may recover quickly within 48 hours with the assistance of early and timely resuscitation and other necessary supportive treatments.
.
In addition, the apparent volume of distribution of drugs in patients with AKI may change significantly, which significantly affects the distribution of water-soluble antibacterial drugs
.
Correspondingly, when AKI is quickly corrected, there is no need to rush to reduce the medication dose based on renal function to avoid the failure of anti-infective treatment due to insufficient dose of antibacterial drugs
.
Crass et al.
[14] retrospectively analyzed the incidence of AKI caused by bacterial infection in 18650 hospitalized patients and found that the incidence of AKI was about 17.
5% (3256/18650), and 57.
2% of patients’ renal function usually returned to normal within 48 hours , 50% of patients with moderate renal insufficiency at admission will also improve their renal function within 48 hours (CLcr>50ml/min)
.
Studies have pointed out that the use of low-dose BLs in patients with AKI whose renal function returns to normal within 48 hours may increase the risk of insufficient blood concentration and clinical failure.
It is recommended that wide therapeutic index BLs should not rush to reduce the dose based on renal function, which will help improve Outcomes of infectious diseases in patients with AKI on admission
.
Phase III trials of RECLAIM 1 and 2 [15] also found that in patients with moderate AKI (CLcr 31-50 ml/min), compared with patients who received meropenem 1g q12h (the proportional dose was reduced by 33%), they received 1.
25 g q12h Ceftazidime/avibactam (proportional dose reduction 66% compared with normal renal function) treatment was significantly less effective (45.
2% vs.
74.
3%; p=0.
016)
.
In addition, compared with patients with normal renal function treated with 1g q8h meropenem, the clinical anti-infective efficacy of patients with moderate renal impairment treated with 1g q12h also had a tendency to decrease (74.
3% vs.
86.
1%; p=0.
06)
.
These findings again emphasize that for patients with impaired renal function, an adjustment program that reduces the single dose and does not extend the dosing interval can help achieve the best PK/PD goal of time-dependent antibiotics (fT>MIC)
.
It is worth noting that 67.
2% of patients with moderate AKI who received ceftazidime/avibactam treatment improved their renal function (CLcr>50 ml/min) within 48-72 hours after taking the drug, which is described in the final product description Medium, the recommended dose of ceftazidime/avibactam for patients with moderate renal impairment increased from 1.
25 g q12h to 1.
25 g q8h
.
In addition, similar results were also suggested in clinical trials of ceftizide/tazobactam and cefiderocol
.
Therefore, adjusting the therapeutic dose of antibacterial drugs according to the creatinine clearance rate does not guarantee that the blood concentration of patients with renal insufficiency is the same as the blood concentration of patients with normal renal function when the full dose of antibacterial drugs is applied [16]
.
Overall, the current research supports the following views: ①In patients with sepsis-related AKI, there is no need to rush to reduce the dose of new BLs and/or BL/BLIs based on renal function, because AKI may be within 48 hours in most cases Recover quickly
.
②Even for patients with persistent AKI, considering the wider therapeutic index (treatment window) and lower toxicity of the new BLs and/or BL/BLIs, it is safe and effective to adjust the drug treatment dose according to the creatinine clearance rate after 48 hours
.
③For patients with persistent AKI, the daily therapeutic dose of antibacterial drugs should be ensured as much as possible, and a plan that reduces the single dose rather than prolongs the dosing interval will help achieve the best PK/PD target.
Prolonging the infusion time may improve AKI patients play an important role in the anti-infection efficacy
.
2 Renal replacement therapy Continuous renal replacement and prolonged intermittent renal replacement therapy are commonly used renal replacement therapy for patients with sepsis-related AKI, accounting for about 70%, and it is very challenging to adjust the dose of new BLs and/or BL/BLIs Sex
.
Because the biochemical and pharmacokinetic characteristics of BLs determine that they are very easy to be cleared by RRT, the settings of RRT, including blood purification mode, filter type, pre- and post-dilution ratio, blood flow rate, and ultrafiltration rate will all affect the drug's drugdynamics
.
The remaining kidney function and the rapidly restored kidney function will also have an impact in this process
.
So far, there is a lack of pharmacokinetic data of novel BLs and/or BL/BLIs during CRRT, and there is no dosage recommendation for the application of novel BLs and/or BL/BLIs during renal replacement therapy
.
Real-world studies have confirmed that CRRT is an independent risk factor for treatment failure and drug resistance of ceftazidime/avibactam and cefothiazide/tazobactam
.
Shields et al.
found that CRRT patients have a higher incidence of ceftazidime/avibactam resistance (OR: 26.
67, 95% CI: 2.
24-317.
1), which may be closely related to the failure to achieve an effective PK/PD target [17]
.
3 ARCARC is a pathological condition, defined as normal creatinine level, but the measured creatinine clearance rate (CLcr) exceeds 130ml/min for men and 120ml/min for women
.
Reports on the incidence of ARC vary, ranging from 16.
4% to 85%
.
The phenomenon of ARC is very worrying in the application of BLs, because excessive renal clearance will lead to insufficient blood drug concentration, which in turn will affect the clinical anti-infective efficacy and lead to the occurrence of bacterial resistance
.
Increasing the dose and prolonging the infusion time is a necessary plan for ARC patients to use BLs to achieve the ideal PK/PD goal
.
Among the new types of BLs and/or BL/BLIs, cefiderocol is the only drug that formulates dosing standards for ARC patients during the drug development process.
2g q6h, infusion time greater than 3 hours, is the recommended regimen for anti-infective treatment for ARC patients
.
However, the dosage of other new BLs and/or BL/BLIs for ARC patients needs to be further improved [18]
.
3.
PK/PD optimization of new BLs and/or BL/BLIs in severe kidney patients 1 The best PK/PD target for preventing drug-resistant severely ill patients with new BLs and/or BL/BLIs anti-infective therapy has been controversial
.
Although the phase II and phase III clinical trials of the drug adopted a more conservative PK/PD target (ie 40%-70% fT>MIC) for anti-infective treatment, clinical data from severely ill patients showed that a higher PK The /PD goal helps to improve the clinical prognosis of patients
.
We know that antimicrobial exposure is not only closely related to the clinical anti-infective efficacy, but also closely related to the inhibition of drug resistance.
The optimization of the dose of antimicrobial drugs is an effective method to inhibit the occurrence of drug resistance
.
A recent systematic review of preclinical and clinical trials found that when the trough concentration of the drug is at least 4 times higher than the MIC (Cmin/MIC>4), it can effectively prevent the occurrence of BLs resistance
.
Therefore, the dosing regimen to inhibit the occurrence of drug resistance should focus on achieving the PK/PD goal of 100% fT>4-8 × MIC
.
Due to the presence of more non-susceptible strains with high MIC in the severe environment, coupled with a variety of factors that cause changes in the PK of antibacterial drugs (such as ARC, higher intensity CRRT), even if the best drug delivery strategy is adopted (higher Dosage and prolonged infusion time) may not achieve the desired PK/PD target
.
In this case, TDM has a better guiding value for the adjustment of the dose of antibacterial drugs, which will help promote the precise anti-infective treatment of critically ill patients [19-22]
.
2 TDM In people with different types of renal impairment, adaptive TDM strategies can significantly increase the achievement rate of BLsPK/PD goals
.
For new BLs and/or BL/BLIs, although there is little clinical experience with TDM strategies, the adjustment of drug delivery strategies under the guidance of TDM is recognized as a safe and effective tool for critically ill patients to achieve positive PK/PD goals early
.
However, there are still many difficulties in the widespread promotion of this method: first, for those BLs with high plasma protein binding rate, the concentration of unbound drugs must be measured; second, based on the complex pathophysiological changes of critically ill patients, TDM results should be provided in real time every day.
To guide clinical treatment; finally, for most new BLs and/or BL/BLIs, it is still necessary to develop accurate, sensitive and easy-to-use analytical methods, and use rigorous methods for verification
.
In short, patients with sepsis-related AKI are not eager to reduce the medication dose based on renal function within 48 hours.
For patients receiving RRT or ARC patients, there is currently no specific recommendation for the dosing regimen.
The drug dosing is selected based on conservative PK/PD goals.
It may lead to unsatisfactory anti-infective effects of new BLs and/or BL/BLIs in patients with severe renal injury
.
The implementation of PK/PD optimized drug delivery strategies based on multiple daily doses, extended infusion time, and real-time TDM guidance has been proven to maximize the anti-infective efficacy of traditional BLs.
For new BLs and/or BL/ The significance of BLIs dosage adjustment needs to be confirmed by further clinical studies [23-25]
.
4.
Summary China's gram-negative bacteria drug resistance situation is severe, and the clinical anti-infective treatment of critically ill patients is facing major challenges.
Once CRE, CRPA and other MDR and XDR gram-negative bacteria infections occur, the options for treatment are very limited
.
The dosage optimization of new BLs and/or BL/BLIs antibacterial drugs is an important factor in determining the clinical anti-infective efficacy and the occurrence of drug resistance
.
In severe settings, AKI, RRT and ARC are three extremely challenging clinical situations that we must face: ① The dose adjustment of new BLs and/or BL/BLIs in AKI patients should be delayed until 48 hours after the start of treatment.
Then according to CLcr to adjust the corresponding dose of patients with persistent AKI, prolonged or continuous infusion can maximize the PK/PD goal
.
② CRRT patients should pay attention to the mode of renal replacement, the amount of treatment, and the setting of parameters, as well as the influence of residual renal function; when a higher intensity CRRT treatment is performed, the amount of antibacterial drugs should not be reduced; Patients with MIC-insensitive strains may need to extend the infusion time and increase the dose of antibacterial drugs
.
③ For people at high risk of ARC, CLcr should be measured regularly.
When applying new BLs and/or BL/BLIs anti-infective treatments, it is strongly recommended to implement a larger dose and long-term infusion of administration strategy
.
Real-time TDM monitoring guides the dosage adjustment of new BLs and/or BL/BLIs, and achieves the positive PK/PD target of 100% fT>4-8×MIC, which can maximize the anti-infective efficacy of drugs and effectively prevent the emergence of drug resistance
.
In the future, anti-infective treatment optimization strategies for critically ill patients based on real-time TDM should be used as a basic part of the antibacterial drug management plan.
A multidisciplinary working group composed of critically ill physicians, infectious disease physicians, clinical microbiologists, and clinical pharmacists will work side by side, which will help Improve the clinical prognosis of patients with sepsis
.
Expert profile Cui Na, MD, Chief Physician of the Department of Critical Care Medicine, Peking Union Medical College Hospital, and postgraduate tutor
.
Standing committee member of the Critical Care Medicine Professional Committee of the Chinese Women Physicians Association, an expert on the senior talent evaluation project of the National Health Commission, an expert on the evaluation of degrees from the Ministry of Education, and an expert on the evaluation of the National Natural Science Foundation of China
.
Research direction: severe infection, sepsis immunity, severe hemodynamics
.
Presided over 2 National Natural Science Foundation projects, 1 Beijing Natural Science Foundation project, 1 Tibet Natural Science Foundation project, presided over a number of national, provincial and ministerial projects such as the Beijing Municipal Science and Technology Commission Major Project, the Chinese Academy of Sciences Translational Medicine, and the Chinese Medical Association Industry Fund
.
Published many papers in domestic and foreign professional journals as the first author and corresponding author, including more than 30 SCI papers (total IF>90), and co-edited more than 10 academic monographs and textbooks
.
Served as peer review reviewer of Journal of Hospital Infection, BMC Psychiatry, European Journal of Inflammation, Chinese Medical Journal and other journals
.
This article is only used to provide scientific information to medical and health professionals, and does not represent the platform's position.
Review of previous wonderful content: 1.
β-lactam drugs for treatment of severe infections-guidelines for optimization points, in-depth interpretation! 2.
What challenges do patients with severe sepsis and septic shock with renal insufficiency face in anti-infective treatment? 3.
What are the benefits of rapid pharmacological monitoring for anti-infective treatment of critically ill patients? 4.
The PK/PD target system helps optimize the clinical medication plan of antibiotics.
5.
Klebsiella pneumoniae: a common opportunistic pathogen.
6.
The posture! This is how the origin of the highly virulent Klebsiella pneumoniae came from.
.
.
7.
What are the important virulence genes and pathogenic mechanisms of Klebsiella pneumoniae? Clarify it in one article! 8.
Klebsiella pneumoniae: There are many challenges in treatment, prevention and infection control.
How to break through? 9.
"Save" sepsis and grasp the best time for anti-infection treatment!