New Assisted Immunotherapy: Concepts and the Future in Non-Small Cell Lung Cancer.
-
Last Update: 2020-08-01
-
Source: Internet
-
Author: User
Search more information of high quality chemicals, good prices and reliable suppliers, visit
www.echemi.com
. Lung cancer is the leading cause of cancer-related deaths worldwide. Patients with removable non-small cell lung cancer (NSCLC) are usually treated with surgery and complementary chemotherapy. However, these patients still have a high risk of recurrence and death. Unfortunately, the treatment of non-small cell lung cancer, which can be removed, has made little progress over the past few decades. The new complementary treatment, which is seen as a way to improve the survival rate of patients with small cell lung cancer, is a controversial topic. A systematic review of 32 randomized trials involving 10,000 patients showed no difference in the survival rate of preoperative and postoperative chemotherapy. As a result, coupled with the inevitable concern that removable tumors progress after relatively ineffective new assisted chemotherapy, new complementary chemotherapy is no longer popular, with many clinicians preferring postoperative-assisted chemotherapy.however, in the past few years, new complementary treatments have re-emerged, as data from various ongoing trials suggest that new complementary immunotherapy may have significant efficacy and may increase the survival rate of patients with non-small cell lung cancer that can be removed. In this review, we discuss evidence of support for the role of new complementary immunotherapy in the multi-channel treatment of removable non-small cell lung cancer. We summarize the early results of ongoing clinical trials and highlight the challenges of adopting a unified definition of "therapeutic success". In order to seek regulatory approval for new complementary immunotherapy and establish it as a standard treatment, we need to overcome some obstacles.
the most famous breakthrough in the current immuno-aids therapy is certainly the CheckMate-159 trial conducted by the Johns Hopkins Medical School team, from esMO's stunning 2016 debut to ASCO's good mid-term results in 2017, to the 2018 American Association for Cancer Research (AACR) annual meeting, which appeared directly in the New England Journal of Medicine. . . .
. The main protagonist of this trial is the familiar Nivolumab. A total of 21 patients with lung cancer who were phased in Stage I-IIIA, who were able to perform root-treatment surgery, were given a new complementary treatment every two weeks before the scheduled operation and operated on two injections.
the main endpoint of the trial is significant pathological remission, in addition to the researchers also removed the tumor's genetic mutation, the patient's T-cell changes in the body, after all, the new immunotherapy has many unsolved mysteries, can get more data must be better. "We're all stunned,"
, according to study leader Drew Pardoll, director of the Institute for Oncology Immunotherapy at the Johns Hopkins School of Medicine. Of the 20 patients who surgically removed the tumor, 9 had significant pathological remission, and even two had no cancer cells at all!
.
even more amazing, after the doctor surgery to the right side of the "tumor" to take out, put under the microscope to see, found that all immune cells and other normal cells, almost no tumor cells!
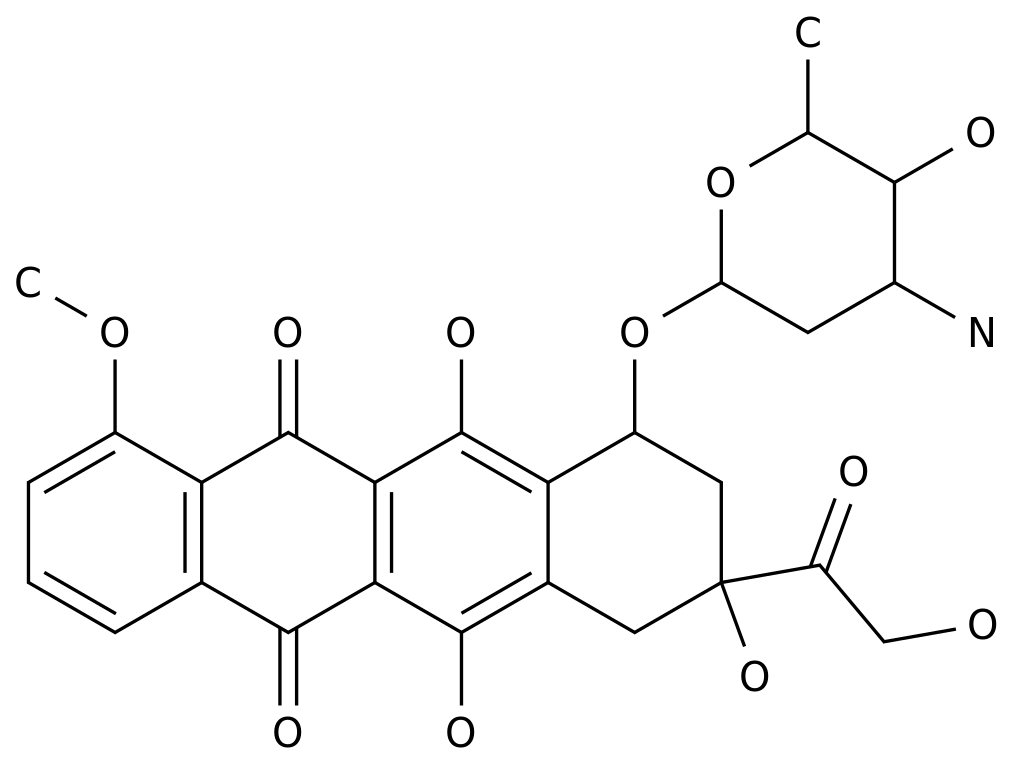
. Figure: A blue dot represents a cell nucleus. It can be seen that before immunotherapy, the microscope is seen a particularly large tumor cells, and after treatment, almost all of the small immune cells replaced.
the safety of the new complementary treatment is also very good and does not delay surgery because of side effects. From the follow-up after surgery, only 3 of the 20 patients had relapses, and at 18 months of follow-up, the overall PFS rate of patients was 73%, which is much better than the recurrence rate of 50% of historical data.
and the use of O-drug before surgery did mobilize T-cells in the patient's body into an anti-tumor immunity state, and pathological slices confirmed that a large number of T cells and macrophages were immersed in the tumor. The patient's tumor mutation load (TMB) is expected to be a biomarker for estimating efficacy.
. Basically presented is a linear relationship, the mutation multi-effect is good
O drug with the existing new auxiliary chemotherapy program, the effect will be even higher.
early tumors can benefit from immunotherapy, because even early tumors are certainly accompanied by an imbalance in the immune system that, by reversing immunosuppression, may help clear the tumor and prevent recurrence.
compared to the use of surgery, pre-surgery use of PD-1 immunotherapy, theoretically has a great advantage, that is, the tumor itself before surgery is still!
. For the new immuno-aids treatment, the new antigen of large tumor is the target ah
tumor is still important?
because it provides more targets needed to train immune cells!
train immune cells as if they were soldiers, first of all, to let them know who the enemy is. In this way the soldiers trained can clear the goal, to achieve targeted.
more cancer cells before surgery, and when the immune system is activated, it may train more immune cells to kill cancer cells. In this way, even if cancer cells that remain invisible to the naked eye after surgery, they are likely to be killed by these trained immune cells!
, on the contrary, if you do surgery first, there are very few residual cancer cells, then the training of immune cells may be significantly compromised.
immunotherapy can also take advantage of the large pre-surgery tumor size, new antigen sized characteristics, fully enhance the activity of the body anti-tumor immuno-T cells, let them spread throughout the body, remove the tiny cancer metastasis, which is better than the use of auxiliary treatment, the advantages have been confirmed in preclinical animal trials. If you wait until after surgery to do immunotherapy, these benefits may diminish as the immune environment changes.
from a scientific point of view, the new immuno-assistance treatment after surgery, but also the surgical removal of tumor tissue, as a further anti-cancer research material. Having immunotherapy take on the role of new complementary therapy, and surgery, can be said to be a strong combination, has a successful precedent in the treatment of breast cancer and melanoma.
, if the use of combination therapy such as immuno-chemotherapy, pre-surgery use has another advantage, that is, the patient is in better physical condition, more resistant to side effects, the probability of successful completion of treatment is higher.
in Phase II control trials (codenamed NEOSTAR), 44 patients with non-small cell lung cancer in the early stages (I to III.A, surgical) received immunotherapy prior to surgery. Of these, 23 were treated with O drugs alone, and 21 were treated with the combination of O drug and CTLA4 inhibitor Ipitzumab. preliminary data
prove that new complementary immunotherapy is promising.
. 1: Overall, the side effects of the new auxiliary treatment are controllable. Importantly, before surgery, immunotherapy was added and did not cause the operation to be postponed.
2: The before and after the use of immunotherapy, it was found that after treatment, the number of immune cells entering the tumor increased.
3: Overall, 25% of patients achieved "major pathological remission (MPR)" after using immunotherapy. This means that cancer cells account for no more than 10% of the tumor or lymph that has been surgically cut off. There were even 8 patients with "tumors" cut off and found no cancer cells at all! This condition is known as "complete pathological remission (pCR).
4: Combination therapy looks better. The main pathological remission (MPR) rate of o drug single drug group was 19%, while the combined treatment group reached 44%.
more exciting data from another study of O-drug drugs (codenamed NADIM).
the study of 46 patients, the new complementary therapy was a combination of "O-drugs and chemotherapy." The results were striking, with up to 85% of patients with surgical stage III.A non-small cell lung cancer receiving "major pathological remission", 71% of which were "complete pathological remission".
. Figure: Pathological remission results in NADIM clinical trials
this data, which is much better than using chemotherapy alone or immunotherapy alone, suggesting that combination therapy has the potential to achieve the goal of 1 plus 2.if subsequent phase III clinical trials can repeat this data, especially if it is shown to reduce the recurrence rate and allow patients to live longer, the new complementary treatment of "immune-chemotherapy" will revolutionize the treatment options for some surgical lung cancer patients.
major pathological remission or objective response rate?
mentioned an important concept in a new complementary therapy:
"major pathological remission"
. A lot of people are not familiar with it, explain here.many people may be more familiar with another criterion: "objective response rate (ORR)." It describes the proportion of patients whose tumors significantly decreased after taking the drug. For chemotherapy drugs and targeted drugs, ORR is a good standard, because these drugs function directly to kill cancer cells, the general effect of the tumor will quickly shrink.but in immunotherapy, it's a bit of a problem just to see if the tumor shrinks. Because immunotherapy is effective, it is usually accompanied by a large number of immune cells entering the tumor. Although there are fewer tumor cells, there are more immune cells.
seeing the CT image at this time, the "tumor" may not shrink, and sometimes even become larger, which may lead to miscalculation. As in the first picture of this article, the immune cells have actually killed almost all cancer cells, but there is still something to see on CT.
new assisted immunotherapy, the radiological assessment of the treatment response with a computed tomography (CT) may not be accurate. The most common post-treatment CT is the symptom-indicated stable disease or 'pseudo-progress', which is associated with T-cell immersion and peritoneal inflammation in the early stages of treatment. As a result, some patients can benefit clinically from immunotherapy without shrinking the initial radiological tumor. This process occurs because immune cells are immersed in the tumor, rather than actually growing the tumor. As supported by the Preclinical Institute, the new auxiliary PD-L1 blocking may enhance the systemic primers of anti-tumor T cells, potentially eliminating micrometatic cancer, which could otherwise lead to recurrence after surgery.
when deciding the timing of chemotherapy, consider whether the patient is fit for surgery at the time of diagnosis. Differences in congenital and adaptive immune responses between men and women can explain the different rates and mortality rates of autoimmune and infectious diseases, as well as multiple types of cancer. Therefore, it is best to test immunotherapy in-group and design for male and female patients separately, and to plan the appropriate sample size.
. NEOSTAR's clinical data also bear this out. Of the patients who achieved "primary pathology remission", only 60% of the patients appeared to have a "significant lysa size" on the image.
therefore, the use of "objective response rates" may underestimate the effectiveness of immunodrugs as new complementary treatments.that's why the
has adopted "primary pathological remission" rather than "objective response rate" as the primary criterion in multiple immunotherapy trials for new complementary therapy.
the "major pathology remission" indicator, can it be widely used in clinical, but also need to see whether it can predict the total survival of patients, that is, to achieve "major pathological remission" of patients, is not more than did not achieve the live?
there is data to prove this in types such as breast and prostate cancer, but lung cancer data still needs to wait. It is believed that with more and more research, the application of "major pathology mitigation" will become more and more extensive.
further published LCMC3, NEOSTAR and NADIM studies at ASCO in 2019, are impressive as representatives of new complementary immunotherapy for early and local advanced lung cancer.
.
. LCMC3 Study
LCMC3 study aims to assess the efficacy and safety of
Atzhu monotomotic
for new auxiliary treatments in Patients with I.B-III A NSCLC.
the main study endpoint is MPR (MajorPathological Response, a significant pathological remission defined as a surviving tumor cell in a removal specimen of 10%).
secondary studies included safety, correlation between PD-L1 expression levels and efficacy, tumor mutation load (TMB), and gene expression characteristics.
results showed that
MPR was 19% and pCR was 5%
, and in terms of safety, only 6 of the 101 patients had treatment-related adverse reactions of 3 to 4 levels.
in addition, subgroup analysis found that pathological remission and MPR efficacy were not related to PD-L1 expression and TMB.
.
although MPR is only 19%, the overall safety of the new adjunct drug at artethria is good. It's just that the MPR rate doesn't seem to have any obvious correlation with PD-L1 expression and TMB.
comprehensive LCMC3, NEOSTAR and NADIM studies, due to the small sample size of the above study, immunotherapy should be used for what kind of program, how to combine and other problems to solve and determine, still need a higher level of evidence-based medical evidence for further demonstration (such as Checkmate-861 Phase III clinical study, Impower030 Phase III clinical study, etc.).in addition, MPR as the main research endpoint of the new auxiliary immunotherapy of lung cancer, as pD-L1 expression of the test, there are different standards, different levels of subjective judgment and other issues, so it also puts a higher challenge to pathologists.
This article is an English version of an article which is originally in the Chinese language on echemi.com and is provided for information purposes only.
This website makes no representation or warranty of any kind, either expressed or implied, as to the accuracy, completeness ownership or reliability of
the article or any translations thereof. If you have any concerns or complaints relating to the article, please send an email, providing a detailed
description of the concern or complaint, to
service@echemi.com. A staff member will contact you within 5 working days. Once verified, infringing content
will be removed immediately.