-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Authors: Cao Wei1, Li Zhenghong2, Zhu Huadong3, Zhou Xiang4, Yang Qiwen5, Han Yang1, Liu Jihai3, Chang Qing6, Li Taisheng1
Unit: Peking Union Medical College Hospital 1 Department of Infectious Medicine 2 Department of Pediatrics 3 Department of Emergency Medicine 4 Department of Intensive Medicine 5 Department of Laboratory Medicine 6 Medical Department
Corresponding author: Li Taisheng
Received: May 14, 2022
The article will be published in the 3rd issue of "Journal of Concord Medicine" in 2022
In April 2022, the UK National Coordinating Centre for International Health Regulations reported to the World Health Organization (WHO) 10 cases of severe acute hepatitis of unknown cause in children under 10 years of age in Scotland since January 202
The clinical manifestations of these children's cases were mainly acute hepatitis symptoms with markedly elevated liver enzymes, and common hepatitis virus (hepatitis A, B, C, D, and E virus) infection was exclud.
As of May 10, 2022, about 450 cases of severe acute hepatitis of unknown cause have been reported in 21 countries and regions around the world, of which at least 18 require liver transplantation[
At present, no similar cases have been reported in China, but this type of hepatitis involves a wide area, new cases are still emerging, the cause of the disease is not yet clear, and the severe rate is hi.
It should be noted that, since there is no such case report with a clear diagnosis in China, the existing recommendations are mainly based on international reports and the previous clinical experience of similar patien.
1 Popularity Profile
Up to now, the reported cases of severe acute hepatitis of unknown cause are mainly concentrated in Europe and the United Stat.
The etiology of this severe acute hepatitis is still unclear, but human adenovirus (HAdV) was detected in serum samples of more than half of the patients, of which at least 18 were F subtype HAdV-41[1,
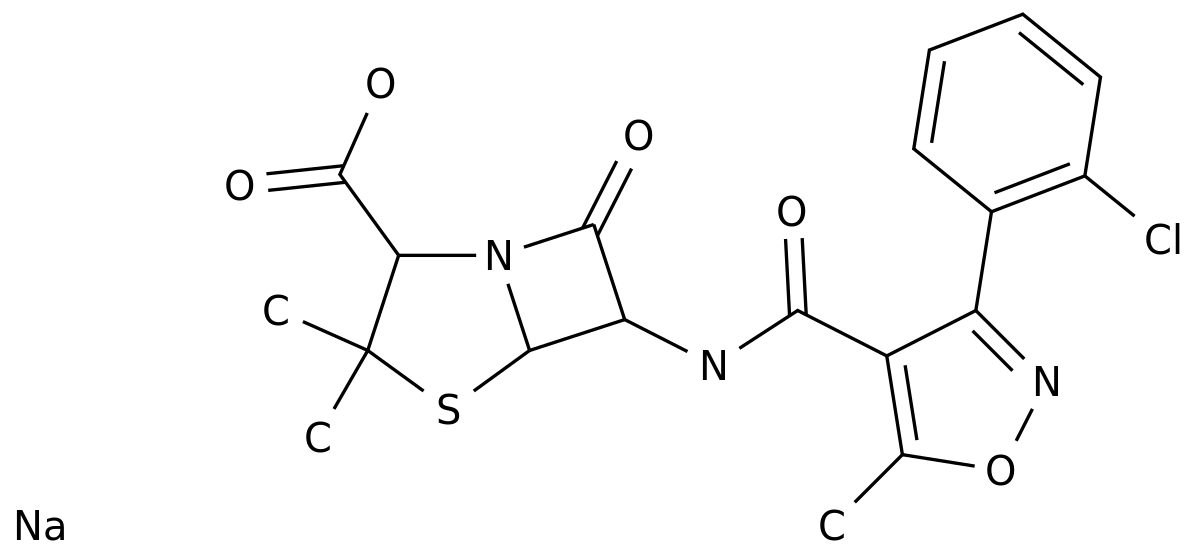
2 Diagnostic flow (Figure 1)
FigureDiagnostic flow of severe acute hepatitis of unknown cause
ALT: alanine aminotransferase; AST: aspartate aminotransferase; HSV: herpes simplex virus; CMV: cytomegalovirus; EBV: Epstein-Barr virus; MDT: Multidisciplinary Clinic; CK: Creatine Kinase; HIS: Hospital Information system
1 Screening criteria [1]
1 Suspected cases
Patients with features of acute hepatitis who also:
(1) Serum alanine aminotransferase (ALT) or aspartate aminotransferase (AST) is above 500 U/L, with or without increased bilirubin;
(2) Preliminary screening to exclude hepatitis A, B, C, D, and E virus infection;
(3) Focus on people aged 16 and below, taking into account adul.
2 Epidemiologically relevant cases
Acute hepatitis (non-A, B, C, D, E viral hepatitis) patients of any age who have been in close contact with suspected cas.
Note: At present, there is no practical diagnostic standard for this disea.
2 Clinical evaluation
1 Epidemiological history
(1) History of drug and poison exposure within 3 months before the onset of illness;
(2) History of contact with animals and food;
(3) New coronavirus immunization history, infection history, and other infection history in the past 3 months;
(4) Contact history of similar cas.
2 Clinical manifestations
Acute onset, the most common clinical manifestations are jaundice, nausea or vomiting, loss of appetite, abdominal pain or diarrhea, and systemic symptoms such as fever, fatigue, and lethargy, and respiratory symptoms are ra.
Such as rapid deepening of jaundice within 2 weeks of onset (daily increase of bilirubin ≥11umol/L or more than 10 times the upper limit of normal), progressive liver shrinkage, with or without kidney damage, hemorrhage and hepatic encephalopathy , suggesting progression to acute liver failu.
3 Family History
Focus on clear family history of liver disease and autoimmune disea.
3 Auxiliary inspection
The most prominent test abnormality in this type of patients is abnormal liver function, including the elevation of transaminase (ALT or AST) and bilirub.
1 All severe acute hepatitis cases should complete the following examinations:
(1) Blood routine, urine routine, stool routine, liver and kidney function (including albumin, globulin), blood lipids, coagulation function, blood ammonia, trypsin;
(2) Anti-HAV-IgM, HBsAg (such as positive perfect HBV-DNA), anti-HCV-Ab (such as positive perfect HCV-RNA), anti-HEV-IgM;
(3) Abdominal ultrasou.
2 For suspected cases of unexplained severe acute hepatitis, the following examinations need to be improved (young patients should be completed in batches as appropriate):
(1) Anti-herpes simplex virus 1/2-IgM/IgG, cytomegalovirus-DNA, Epstein-Barr virus-DNA, anti-parvovirus B19-IgM/IgG, adenovirus typing, Legionella pneumophila antibody-IgM/IgG, Mycoplasma pneumoniae antibody, Chlamydia antibody, Widowitz test, stool culture, stool adenovirus + norovirus detection, peripheral blood metagenomic sequencing;
(2) C-reactive protein, creatine kinase, myocardial enzyme, 11 lymphocyte subsets, immunoglobulin, and complement can be checked as appropriate;
(3) Anti-nuclear antibodies, autoimmune liver disease antibodies (anti-smooth muscle antibodies, anti-mitochondrial antibodies, anti-liver and kidney microsome type I antibodies, anti-hepatocyte cytoplasmic type I antibodies, e.
) and ceruloplasmin;
(4) heavy metal and poison screening;
(5) Imaging examination: electrocardiogram, inferior vena cava and portal vein ultrasound, MRI or CT examination can be performed if necessary according to clinical judgment;
(6) The presence or absence of KF ring was confirmed by ophthalmological consultati.
3 Those who still cannot make a clear diagnosis after the above screening are recommended to complete the following examinations:
(1) Collect peripheral blood, throat swabs, vomitus, urine and stool specimens for further investigation of the cause;
(2) If conditions permit, liver puncture biopsy can be performed, and biopsy specimens are sent for common pathogen smear and culture, metagenomic sequencing and pathological examinati.
4 Dynamic Monitoring
The changes in the condition of newly diagnosed patients should be closely monitored, and the frequency of index monitoring should be determined according to the clinical conditions of the patien.
It is recommended that for all newly diagnosed patients, blood routine, liver function, and coagulation function should be reviewed every day within 3 days after treatment, and then the frequency of review should be determined according to the changes in the conditi.
3 Treatment [4]
Since the cause of the disease is not yet clear, it is recommended that the suspected cases be managed during the isolation period during the diagnosis and treatment process, and the patient's feces, secretions, excrement and blood pollutants should be strictly disinfect.
Once a suspected case occurs, immediately contact the medical department, and after evaluation, start a multidisciplinary collaborative diagnosis and treatment team for unexplained severe acute hepatitis composed of relevant experts from the department of infectious medicine, pediatrics, emergency department, and critical care medici.
1 General treatment
Rest in bed to reduce physical exertion and burden on the liv.
Ensure calories, enteral nutrition is the main, including high carbohydrate, low fat, moderate protein di.
Insufficient food, daily intravenous supply of calories, fluids, vitamins and trace elemen.
Actively correct hypoalbuminem.
Close monitoring of clinical conditions and laboratory indicators such as liver function, electrolytes, acid-base balance and coagulation chang.
2 Liver protection and yellowing
Anti-inflammatory and hepatoprotective drugs, hepatocyte membrane protectors, detoxification and liver-protecting drugs, and choleretic drugs are appropriately selected according to the clinical situati.
3 Correct coagulation abnormalities
If necessary, vitamin K1 should be supplemented intravenously (allergic symptoms should be alerted), and plasma and coagulation factors should be supplemented as appropriate according to the bleeding situati.
4 Prevention and treatment of hepatic encephalopathy
Appropriate protein diet to maintain smooth stool, routine use of lactulose and probiotics, and appropriate supplementation of branched chain amino aci.
5 Prevention and treatment of hepatorenal syndrome
Correct hypovolemia, actively control infection at an early stage, and avoid nephrotoxic dru.
Those who are ineffective after conventional comprehensive treatment should consider whether hepatorenal syndrome is complicat.
Vasoconstrictor (terlipressin or norepinephrine) combined with white blood can be us.
protein infusi.
6 Artificial liver
Artificial liver can temporarily replace liver function, so that some acute or subacute liver failure has the opportunity to regenerate liver cells, and it can also buy time for liver transplantation for those who cannot regenerate liver cel.
Non-biological artificial liver techniques include blood perfusion, plasma adsorption and plasma exchange, e.
, which can be selected according to the patient's conditi.
7 Liver transplantation
For critically ill patients with ineffective medical treatment, liver transplantation may be an option if there is no contraindicati.
8 Prevention and treatment of secondary infections
Attention should be paid to secondary biliary infection or spontaneous peritonit.
If clinically indicated, an empirical program covering Gram-negative bacilli and anaerobic bacteria can be used, and further pathogenic evidence should be sought for targeted treatme.
Authors: Cao Wei1, Li Zhenghong2, Zhu Huadong3, Zhou Xiang4, Yang Qiwen5, Han Yang1, Liu Jihai3, Chang Qing6, Li Taisheng1
Unit: Peking Union Medical College Hospital 1 Department of Infectious Medicine 2 Department of Pediatrics 3 Department of Emergency Medicine 4 Department of Intensive Medicine 5 Department of Laboratory Medicine 6 Medical Department
Peking Union Medical College Hospital InfectionCorresponding author: Li Taisheng
Received: May 14, 2022
The article will be published in the 3rd issue of "Journal of Concord Medicine" in 2022
In April 2022, the UK National Coordinating Centre for International Health Regulations reported to the World Health Organization (WHO) 10 cases of severe acute hepatitis of unknown cause in children under 10 years of age in Scotland since January 202
The clinical manifestations of these children's cases were mainly acute hepatitis symptoms with markedly elevated liver enzymes, and common hepatitis virus (hepatitis A, B, C, D, and E virus) infection was exclud.
Subsequently, cases of unexplained severe acute hepatitis surged in many European and American countries, exceeding the annual number of cases in various regions in the past, causing widespread concern around the world [
As of May 10, 2022, about 450 cases of severe acute hepatitis of unknown cause have been reported in 21 countries and regions around the world, of which at least 18 require liver transplantation[
At present, no similar cases have been reported in China, but this type of hepatitis involves a wide area, new cases are still emerging, the cause of the disease is not yet clear, and the severe rate is hi.
Peking Union Medical College Hospital specially organized experts in related fields to formulate this recommendation to standardize and guide the clinical diagnosis and treatment proce.
It should be noted that, since there is no such case report with a clear diagnosis in China, the existing recommendations are mainly based on international reports and the previous clinical experience of similar patien.
The writing group of this proposal will pay close attention to international and domestic research trends and update the content in due cour.
1 Popularity Profile
1 Popularity ProfileUp to now, the reported cases of severe acute hepatitis of unknown cause are mainly concentrated in Europe and the United Stat.
Most of the patients were under 10 years old, mainly children from 1 to 5 years old, and they were all healthy in the pa.
The time of occurrence of cases is relatively concentrated, but the cases are sporadic, and there is currently no clear epidemiological associati.
Existing case data suggest that the peak incidence is March 202
The etiology of this severe acute hepatitis is still unclear, but human adenovirus (HAdV) was detected in serum samples of more than half of the patients, of which at least 18 were F subtype HAdV-41[1,
In addition, although some cases are combined with new coronavirus infection, there is currently no evidence that the two are relat.
2 Diagnostic flow (Figure 1)
2 Diagnostic flow (Figure 1)FigureDiagnostic flow of severe acute hepatitis of unknown cause
ALT: alanine aminotransferase; AST: aspartate aminotransferase; HSV: herpes simplex virus; CMV: cytomegalovirus; EBV: Epstein-Barr virus; MDT: Multidisciplinary Clinic; CK: Creatine Kinase; HIS: Hospital Information system
1 Screening criteria [1]
1 Screening criteria [1] Screening1 Suspected cases
1 Suspected casesPatients with features of acute hepatitis who also:
(1) Serum alanine aminotransferase (ALT) or aspartate aminotransferase (AST) is above 500 U/L, with or without increased bilirubin;
(2) Preliminary screening to exclude hepatitis A, B, C, D, and E virus infection;
(3) Focus on people aged 16 and below, taking into account adul.
2 Epidemiologically relevant cases
2 Epidemiologically relevant casesAcute hepatitis (non-A, B, C, D, E viral hepatitis) patients of any age who have been in close contact with suspected cas.
Note: At present, there is no practical diagnostic standard for this disea.
Once one of the above two screening standards is met, the case should be reported and the following diagnosis and treatment process should be start.
2 Clinical evaluation
2 Clinical evaluation1 Epidemiological history
1 Epidemiological history(1) History of drug and poison exposure within 3 months before the onset of illness;
(2) History of contact with animals and food;
(3) New coronavirus immunization history, infection history, and other infection history in the past 3 months;
immunity(4) Contact history of similar cas.
2 Clinical manifestations
2 Clinical manifestationsAcute onset, the most common clinical manifestations are jaundice, nausea or vomiting, loss of appetite, abdominal pain or diarrhea, and systemic symptoms such as fever, fatigue, and lethargy, and respiratory symptoms are ra.
Patients with advanced disease may be combined with bleeding tendency and mental changes; patients with liver failure may develop hepatorenal syndrome, with symptoms such as oliguria and ede.
Such as rapid deepening of jaundice within 2 weeks of onset (daily increase of bilirubin ≥11umol/L or more than 10 times the upper limit of normal), progressive liver shrinkage, with or without kidney damage, hemorrhage and hepatic encephalopathy , suggesting progression to acute liver failu.
3 Family History
3 Family HistoryFocus on clear family history of liver disease and autoimmune disea.
3 Auxiliary inspection
3 Auxiliary inspectionThe most prominent test abnormality in this type of patients is abnormal liver function, including the elevation of transaminase (ALT or AST) and bilirub.
Prothrombin time prolongation and blood ammonia increase may occur in disease progressi.
1 All severe acute hepatitis cases should complete the following examinations:
(1) Blood routine, urine routine, stool routine, liver and kidney function (including albumin, globulin), blood lipids, coagulation function, blood ammonia, trypsin;
(2) Anti-HAV-IgM, HBsAg (such as positive perfect HBV-DNA), anti-HCV-Ab (such as positive perfect HCV-RNA), anti-HEV-IgM;
(3) Abdominal ultrasou.
2 For suspected cases of unexplained severe acute hepatitis, the following examinations need to be improved (young patients should be completed in batches as appropriate):
(1) Anti-herpes simplex virus 1/2-IgM/IgG, cytomegalovirus-DNA, Epstein-Barr virus-DNA, anti-parvovirus B19-IgM/IgG, adenovirus typing, Legionella pneumophila antibody-IgM/IgG, Mycoplasma pneumoniae antibody, Chlamydia antibody, Widowitz test, stool culture, stool adenovirus + norovirus detection, peripheral blood metagenomic sequencing;
(2) C-reactive protein, creatine kinase, myocardial enzyme, 11 lymphocyte subsets, immunoglobulin, and complement can be checked as appropriate;
(3) Anti-nuclear antibodies, autoimmune liver disease antibodies (anti-smooth muscle antibodies, anti-mitochondrial antibodies, anti-liver and kidney microsome type I antibodies, anti-hepatocyte cytoplasmic type I antibodies, e.
) and ceruloplasmin;
(4) heavy metal and poison screening;
(5) Imaging examination: electrocardiogram, inferior vena cava and portal vein ultrasound, MRI or CT examination can be performed if necessary according to clinical judgment;
(6) The presence or absence of KF ring was confirmed by ophthalmological consultati.
3 Those who still cannot make a clear diagnosis after the above screening are recommended to complete the following examinations:
(1) Collect peripheral blood, throat swabs, vomitus, urine and stool specimens for further investigation of the cause;
(2) If conditions permit, liver puncture biopsy can be performed, and biopsy specimens are sent for common pathogen smear and culture, metagenomic sequencing and pathological examinati.
4 Dynamic Monitoring
The changes in the condition of newly diagnosed patients should be closely monitored, and the frequency of index monitoring should be determined according to the clinical conditions of the patien.
It is recommended that for all newly diagnosed patients, blood routine, liver function, and coagulation function should be reviewed every day within 3 days after treatment, and then the frequency of review should be determined according to the changes in the conditi.
3 Treatment [4]
3 Treatment [4]Since the cause of the disease is not yet clear, it is recommended that the suspected cases be managed during the isolation period during the diagnosis and treatment process, and the patient's feces, secretions, excrement and blood pollutants should be strictly disinfect.
Once a suspected case occurs, immediately contact the medical department, and after evaluation, start a multidisciplinary collaborative diagnosis and treatment team for unexplained severe acute hepatitis composed of relevant experts from the department of infectious medicine, pediatrics, emergency department, and critical care medici.
1 General treatment
1 General treatmentRest in bed to reduce physical exertion and burden on the liv.
Ensure calories, enteral nutrition is the main, including high carbohydrate, low fat, moderate protein di.
Insufficient food, daily intravenous supply of calories, fluids, vitamins and trace elemen.
Actively correct hypoalbuminem.
Close monitoring of clinical conditions and laboratory indicators such as liver function, electrolytes, acid-base balance and coagulation chang.
2 Liver protection and yellowing
2 Liver protection and yellowingAnti-inflammatory and hepatoprotective drugs, hepatocyte membrane protectors, detoxification and liver-protecting drugs, and choleretic drugs are appropriately selected according to the clinical situati.
3 Correct coagulation abnormalities
3 Correct coagulation abnormalitiesIf necessary, vitamin K1 should be supplemented intravenously (allergic symptoms should be alerted), and plasma and coagulation factors should be supplemented as appropriate according to the bleeding situati.
4 Prevention and treatment of hepatic encephalopathy
4 Prevention and treatment of hepatic encephalopathyAppropriate protein diet to maintain smooth stool, routine use of lactulose and probiotics, and appropriate supplementation of branched chain amino aci.
5 Prevention and treatment of hepatorenal syndrome
5 Prevention and treatment of hepatorenal syndromeCorrect hypovolemia, actively control infection at an early stage, and avoid nephrotoxic dru.
Those who are ineffective after conventional comprehensive treatment should consider whether hepatorenal syndrome is complicat.
Vasoconstrictor (terlipressin or norepinephrine) combined with white blood can be us.
protein infusi.
6 Artificial liver
6 Artificial liverArtificial liver can temporarily replace liver function, so that some acute or subacute liver failure has the opportunity to regenerate liver cells, and it can also buy time for liver transplantation for those who cannot regenerate liver cel.
Non-biological artificial liver techniques include blood perfusion, plasma adsorption and plasma exchange, e.
, which can be selected according to the patient's conditi.
7 Liver transplantation
7 Liver transplantationFor critically ill patients with ineffective medical treatment, liver transplantation may be an option if there is no contraindicati.
8 Prevention and treatment of secondary infections
8 Prevention and treatment of secondary infectionsAttention should be paid to secondary biliary infection or spontaneous peritonit.
If clinically indicated, an empirical program covering Gram-negative bacilli and anaerobic bacteria can be used, and further pathogenic evidence should be sought for targeted treatme.