-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*Only for medical professionals to read for reference, the 22nd issue of "Respiratory Defense" is here! Non-tuberculous Mycobacteria (NTM) mainly refers to the general term for mycobacteria other than Mycobacterium tuberculosis complex and Mycobacterium leprae, with nearly 200 species of bacteria
.
In recent years, the incidence of NTM disease has been significantly increasing [1]
.
The clinical manifestations and imaging characteristics of NTM disease are heterogeneous, and the treatment is difficult and the treatment course is long, which brings great challenges to clinical diagnosis and treatment
.
The center has treated a large number of patients with NTM lung disease and has accumulated a lot of experience.
Now we select 3 cases to share with you
.
Case 1: Mycobacterium abscessus pulmonary disease [Basic information] The patient was a 40-year-old middle-aged female, an ordinary worker, and was admitted to the hospital on November 15, 2020 because of "repeated cough and sputum for more than 10 years, and aggravated by 1 month"
.
[Present disease history] 10 years ago, the patient had cough, sputum, yellow and white sputum, and it was difficult to cough up the sputum.
After the illness, he was diagnosed with bronchiectasis and infection in a nearby hospital.
The patient’s symptoms repeatedly appeared in the past 10 years and he was given resistance every time.
The infection gets better after treatment
.
In October 2020, the patient felt that the symptoms of cough and sputum were worse than before.
The sputum was yellow and purulent sputum, which was not easy to cough up, accompanied by fever.
The highest body temperature reached 38.
9℃, without chills or hemoptysis.
Right upper lung bronchiectasis, multiple small nodules and patchy shadows in both lungs, received anti-infection treatment with ceftazidime, levofloxacin and other drugs, body temperature decreased, but there was still obvious cough and sputum
.
[Past history and personal history] Deny the history of infectious diseases such as tuberculosis, and deny the history of high blood pressure and diabetes
.
Denies the history of exposure to dust and poisons
.
Deny the family history of hereditary diseases
.
No history of smoking or alcoholism
.
[Physical examination] No cyanosis of the lips, no shortness of breath in the resting state, slightly lower right upper lung breath sounds, no dry and wet rales in both lungs, heart rate 78 beats/min, regular rhythm
.
The lower limbs are not swollen, and the joints of the limbs are normal
.
[Illness analysis] The patient is a middle-aged woman with a chronic course of disease, long-term cough and sputum; lung imaging manifests as bronchiectasis, multiple small nodules under the pleura, and partial lung tissue structure destruction.
Conventional anti-infective treatment is not effective
.
Analysis of the above-mentioned characteristics of the medical history found that the patient had structural lung disease (bronchiectasis).
Considering that the infection-induced symptoms were aggravated this time.
In view of the fact that the patient has not improved significantly with conventional anti-infective treatment, there are characteristic imaging manifestations [2,3], which needs to be considered.
Infection with atypical pathogens such as mycobacteria
.
The next step in diagnosis and treatment needs to focus on pathogenic microorganisms, especially mycobacterial related tests, and further screening of patients for the cause of bronchiectasis
.
[Preliminary diagnosis] Bronchiectasis with infection, pulmonary mycobacterial disease may be possible
.
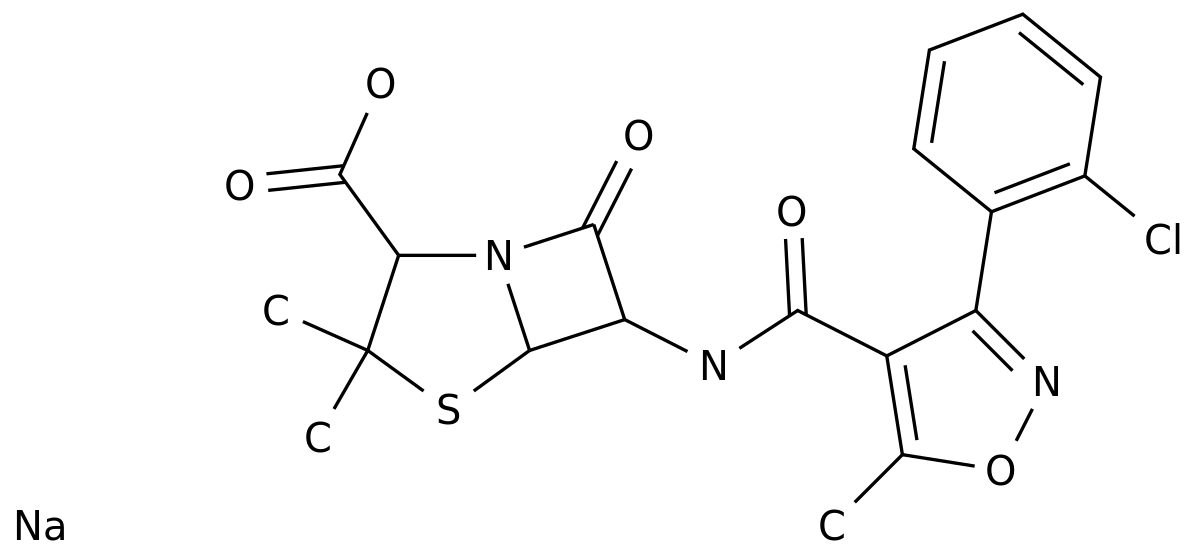
[Diagnosis and treatment] After the patient is admitted to the hospital, complete blood routine and blood biochemistry, infection-related markers, sputum pathogenic microorganisms, autoantibodies, high-resolution CT (HRCT), bronchoscopy and alveolar lavage fluid (BALF) microbiological examinations, and give Cefoperazone Sodium and Sulbactam Sodium Empirically Anti-infection, Phlegm Resolving and Symptomatic Treatment
.
▌ The auxiliary examination results are as follows: blood routine: white blood cell count 9.
03×109/L, neutrophil percentage 70.
70%, lymphocyte percentage 18.
80% ↓, eosinophil percentage 1.
00%
.
Inflammation indicators: high-sensitivity C-reactive protein (hCRP) 52.
36mg/L ↑, erythrocyte sedimentation rate (ESR) 42mm/h ↑, procalcitonin (PCT) 0.
02ng/ml
.
Autoantibodies and tumor markers are normal, 1,3-β-D glucan test (G test), galactomannan antigen test (GM test), latex agglutination test negative, tuberculosis infection T cell spot test (T -SPOT) negative
.
Sputum bacteria/fungus/tuberculosis smear + culture result was negative
.
HRCT: bronchiectasis in the upper right lung, combined with cavities and patchy shadows; multiple small nodules in both lungs, mainly under the right pleura (see Figure 1-1)
.
Figure 1-1 Under the bronchoscope, there are more purulent secretions in the bronchus of the right upper lobe.
After aspiration, the lumen is unobstructed.
Alveolar lavage is performed in each segment of the right upper lobe
.
BALF acid-fast bacilli smear 3+, Mycobacterium tuberculosis MPB64 antigen was negative
.
The patient has BALF acid-fast staining positive, BALF Mycobacterium tuberculosis MPB64 antigen is negative, blood T-SPOT is negative, and it is considered that non-tuberculous mycobacteria may be infected.
To further improve mycobacterial culture, BALF microbial second-generation sequencing
.
BALF microbial second-generation sequencing detected Mycobacterium abscessus; solid and liquid Mycobacterium cultures were positive; Mycobacterium sequencing did not detect Mycobacterium tuberculosis complex
.
▌ Final diagnosis: Mycobacterium abscessus lung disease, bronchiectasis with infection (branch expansion after infection)
.
▌ Treatment and outcome: According to domestic and foreign NTM disease diagnosis and treatment guidelines and expert consensus [1,4,5], combined with the experience of the center, formulate the following anti-infection plan
.
Initial stage: Amikacin, cefoxitin intravenously, combined with clarithromycin (500mg bid) orally, the course of treatment is 2 months
.
After treatment, the patient's body temperature continued to be normal, his cough and sputum symptoms improved, and his activity tolerance increased
.
Further drug susceptibility results are reported as follows (see Figure 1-2): Figure 1-2 drug susceptibility results indicate that conventional anti-NTM drugs are resistant, and need to be combined based on clinical experience.
The continuation phase is adjusted as follows: Linezolid (600mg qd ), moxifloxacin (400mg qd), rifapentin (450mg biw), clarithromycin (500mg bid) orally for at least 1 year
.
After treatment, the patient’s symptoms continued to improve, the NTM drug adverse reaction monitoring was not abnormal, the results of re-examination of ESR, CRP, and PCT were normal, and the re-examination of lung CT showed that the lesion was significantly improved (see Figure 1-3)
.
Figure 1-3 Case 2: Mycobacterium Kansas Pulmonary Disease [Basic Information] The patient is a 45-year-old middle-aged female, a company employee, and was admitted to the hospital on January 20th, 2021.
5.
12 due to "physical examination found shadow of the left lower lung"
.
[Present illness history] The patient’s 2021.
4.
14 physical examination showed a shadow of the left lower lung.
At that time, there was no obvious cough, sputum, low fever, night sweats, chest pain, chest tightness, and shortness of breath
.
After that, the patient came to our hospital for further diagnosis and treatment.
A CT examination of the lungs in the outpatient department of the respiratory department of our hospital on May 2021 showed multiple patchy and nodules in the lower lobe of the left lung, and was hospitalized for further diagnosis and treatment
.
[Past history and personal history] Deny the history of infectious diseases such as tuberculosis, and deny the history of high blood pressure and diabetes
.
Denies the history of exposure to dust and poisons
.
Denies the family history of hereditary diseases
.
No history of smoking or alcoholism
.
[Physical examination] No cyanosis of the lips, no shortness of breath, thick breath sounds in both lungs, no dry and wet rales, heart rate 82 beats/min, regular rhythm
.
No swelling of the lower limbs, no abnormalities in the joints of the limbs
.
[Auxiliary examination] Lung CT showed multiple nodules and patchy shadows in the dorsal and basal segments of the left lower lung, accompanied by local bronchiectasis (see Figure 2-1)
.
Figure 2-1 [Analysis of Condition] The patient is a middle-aged female with no obvious respiratory symptoms; lung imaging showed multiple nodules and patchy shadows in the dorsal and basal segments of the left lower lung, accompanied by local bronchiectasis
.
Analyzing the characteristics of the above medical history, it is found that the patient has characteristic imaging findings[2,3], and mycobacterial infection needs to be considered first.
In addition, it needs to be differentiated from slow-growing pathogens (cryptococcus, etc.
) infectious diseases, and non-infectious diseases.
Differentiate it from tumor diseases, connective tissue disease, lung involvement, idiopathic interstitial pneumonia (RB-ILD, etc.
) [6]
.
The next step in diagnosis and treatment needs to focus on pathogenic microorganisms, especially mycobacteria related tests, and further screening of the causes of lung shadows in patients is required
.
[Preliminary diagnosis] Pulmonary shadow: Pulmonary mycobacterial disease may be
.
[Diagnosis and treatment] After the patient is admitted to the hospital, complete blood routine and blood biochemistry, infection-related markers, sputum pathogenic microorganisms, autoantibodies, HRCT, BALF microorganisms and other examinations
.
▌ The auxiliary examination results are as follows: blood routine: white blood cell count 7.
12×109/L, neutrophil percentage 55%, lymphocyte percentage 23.
8%, eosinophil percentage 10.
5% ↑
.
Inflammation indicators: hCRP, ESR, PCT normal range
.
The results of autoantibodies and tumor markers were normal, and the G test, GM test, and latex agglutination test were negative
.
T-SPOT: The actual release level of γ-interferon (TN)> 10IU/ml ↑, the specific cellular immune response of Mycobacterium tuberculosis was detected ↑
.
Sputum bacteria/fungus/tuberculosis smear + culture result was negative
.
HRCT: Multiple nodules and patchy shadows in the dorsal and basal segments of the left lower lung, accompanied by local bronchiectasis (see Figure 2-1)
.
No obvious abnormalities were found under the bronchoscope
.
Alveolar lavage was performed on the dorsal and basal segments of the lower lobe of the left lung .
The BALF acid-fast bacilli smear was negative, and the Mycobacterium tuberculosis MPB64 antigen was negative
.
The patient's blood was T-SPOT positive, but BALF acid-fast staining was negative, and BALF Mycobacterium tuberculosis MPB64 antigen was negative.
Considering the possibility of non-tuberculous mycobacterial infection, the mycobacterial culture was further improved, and BALF microbial second-generation sequencing
.
BALF microbial second-generation sequencing detected Mycobacterium Kansas; solid and liquid Mycobacterium cultures were positive; Mycobacterium sequencing did not detect Mycobacterium tuberculosis complex
.
▌ Final diagnosis: Mycobacterium kansas lung disease
.
▌ Treatment and outcome: Mycobacterium kansas is mostly sensitive to rifampicin, and is the core treatment drug for mycobacterium kansas lung disease.
According to domestic and foreign NTM disease diagnosis and treatment guidelines and expert consensus [1,4,5], combined with the experience of our center , Formulate the following anti-infection plan
.
Treatment plan: isoniazid (300mg qd), rifampicin (450mg qd), ethambutol (750mg qd), clarithromycin (500mg bid) orally, and the course of treatment is at least 1 year
.
After treatment, the patient has no obvious discomfort and well tolerated.
The NTM drug adverse reaction monitoring has no obvious abnormalities.
The recent reexamination of lung CT revealed obvious absorption of the lesion (see Figure 2-2)
.
Figure 2-2 Case 3: Mycobacterium avium pulmonary disease [Basic information] The patient is a middle-aged and elderly woman, a retired worker, and was admitted to the hospital on March 29, 2020 because of "the shadow of both lungs was found for more than 2 months"
.
[Present illness history] In January 2021, the patient swallowed shrimp shells and caused sore throat.
The laryngoscopy at the otolaryngology department of the outside hospital showed no obvious abnormalities.
Perfect chest CT revealed multiple nodules in both lungs and lungs.
Then in January On the 19th, I went to the outpatient department of the Respiratory Department of our hospital.
A CT scan of the chest showed multiple patchy and speckled shadows in both lungs, and the right lung was the main one
.
The outpatient department perfected blood T-SPOT, sputum tuberculosis smear, sputum tuberculosis culture, bacterial typing, DNA sequencing and other examinations, and no abnormalities were found
.
During the period, the patient had no cough and sputum, no low-grade fever and night sweats, no chest tightness, shortness of breath, no hemoptysis and other discomforts.
He was admitted to the hospital for further diagnosis and treatment
.
Since the onset of the illness, the patient has been mentally well, appetite, sleep, and normal urine and feces, no significant decrease in physical strength, and no significant decrease in weight
.
[Past history and personal history] Deny the history of infectious diseases such as tuberculosis, and deny the history of high blood pressure and diabetes
.
Denies the history of exposure to dust and poisons
.
Deny the family history of hereditary diseases
.
No history of smoking or alcoholism
.
[Physical examination] No cyanosis of the lips, no shortness of breath, thick breath sounds in both lungs, no dry and wet rales, heart rate 85 beats/min, regular rhythm
.
The lower limbs are not swollen, and the joints of the limbs are normal
.
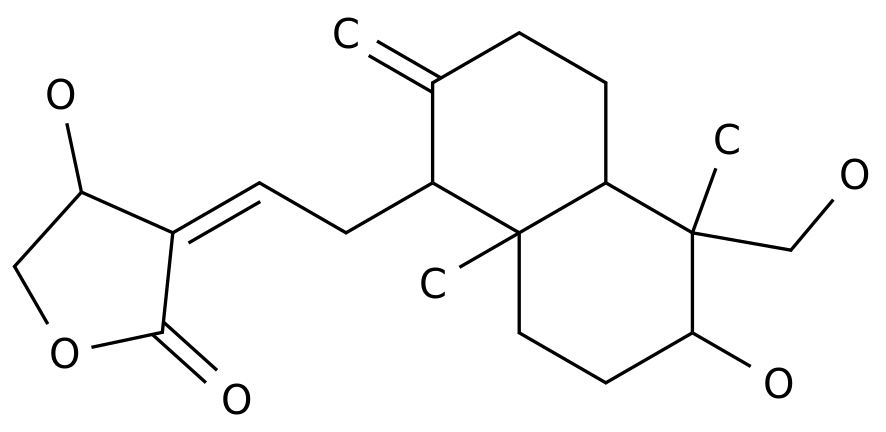
[Auxiliary examination] CT of the lungs showed multiple patchy and speckled shadows in both lungs, with the right lung predominantly (see Figure 3-1)
.
Figure 3-1 [Analysis of the condition] The patient is a middle-aged and elderly woman with no obvious respiratory symptoms; lung imaging showed multiple patchy and speckled shadows in both lungs, mainly in the right lung
.
Analysis of the above-mentioned characteristics of the medical history found that the patient has characteristic imaging findings[2,3], and mycobacterial infection must be considered first, the sputum microbiological test result is negative, and the blood T-SOPT result is negative, so consider the possibility of NTM infection
.
The next step in diagnosis and treatment needs to improve bronchoscopy and BALF microbiological examination, focusing on pathogenic microorganisms, especially NTM-related testing, and further screening of patients with other causes of lung shadows
.
[Preliminary diagnosis] Lung shadow: non-tuberculous mycobacterial lung disease may be possible
.
[Diagnosis and treatment] After the patient is admitted to the hospital, complete blood routine and blood biochemistry, infection-related markers, sputum pathogenic microorganisms, autoantibodies, HRCT, BALF microorganisms and other examinations
.
▌ The auxiliary examination results are as follows: blood routine: white blood cell count 6.
06×109/L, neutrophil percentage 66%, lymphocyte percentage 24.
4%, eosinophil percentage 2.
3%
.
Inflammation indicators: hCRP, ESR, PCT normal range
.
The results of autoantibodies and tumor markers were normal, and the G test, GM test, and latex agglutination test were negative
.
T-SPOT: negative
.
Sputum bacteria/fungus/tuberculosis smear + culture result was negative
.
HRCT: There are multiple patchy and speckled shadows in both lungs, with the right lung predominantly (see Figure 3-1)
.
A small amount of purulent secretions in the middle lobe of the right lung was seen under the bronchoscope
.
After aspiration, the lumen was unobstructed, and bronchoalveolar lavage was performed in the lateral segment of the middle lobe of the right lung .
BALF acid-fast bacilli smear 4+, Mycobacterium tuberculosis MPB64 antigen was negative
.
The patient had BALF acid-fast staining positive, blood T-SPOT negative, and BALF Mycobacterium tuberculosis MPB64 antigen negative.
Considering the possibility of non-tuberculous mycobacterial infection, the mycobacterial culture should be further improved, and BALF microbial second-generation sequencing
.
BALF microbial second-generation sequencing detected Mycobacterium avium complex; solid and liquid Mycobacterium cultures were positive; Mycobacterium sequencing did not detect Mycobacterium tuberculosis complex
.
▌ Final diagnosis: Mycobacterium avium lung disease
.
▌ Treatment and outcome: Mycobacterium avium is one of the subspecies of MAC.
Studies have shown that the efficacy and safety of treatments containing macrolides are good
.
The BALF acid-fast staining of this patient is strongly positive.
According to domestic and foreign NTM disease diagnosis and treatment guidelines and expert consensus [1,4,5], combined with the experience of the center, the following anti-infection plan was formulated
.
Treatment plan: Azithromycin (500mg qd), isoniazid (300mg qd), rifampicin (450mg qd), ethambutol (750mg qd) orally, the course of treatment is at least 1 year
.
The patient had no obvious discomfort in the initial treatment stage.
After 1 month of treatment, the patient developed anorexia and belching.
In 2021.
5.
11, due to increased diarrhea, anorexia, and fatigue, he re-visited the doctor, improved sputum microbiology, lung CT and other examinations, and provided stomach protection and symptomatic treatment
.
The results of the examination indicated sputum acid-fast staining (+), lung CT indicated earlier absorption of lung lesions (see Figure 3-2), and gastroscopy indicated chronic gastritis and mild reflux esophagitis
.
Figure 3-2 Condition analysis: The patient’s imaging and other examination results indicate that the treatment is effective, but there are obvious adverse reactions of anti-NTM drugs.
In view of the positive staining of sputum acid-fast, it is necessary to continue anti-NTM treatment.
The treatment plan is adjusted as follows
.
Anti-NTM regimen: clarithromycin (500mg bid), isoniazid (300mg qd), rifapentine (600mg biw), ethambutol (750mg qd) orally
.
Treatment of adverse gastrointestinal reactions: gastric mucosal protective agents and acid inhibitors, gastrointestinal motility drugs
.
After adjusting the treatment plan, the patient has no obvious discomfort, and the NTM drug adverse reaction monitoring has no obvious abnormality.
Currently, he is closely followed up
.
★Comments from experts: Dr.
Zhang Peng, Department of Respiratory and Critical Care Medicine, Shanghai Public Health Clinical Center, NTM lung disease is the most common type of NTM disease, and the incidence in China has been significantly increasing in recent years
.
Early identification and correct diagnosis are essential to reduce transmission, increase cure rate, and reduce resistance rate
.
The clinical manifestations of patients with NTM lung disease are multifaceted, and some patients have no obvious symptoms at the onset of the disease
.
Of the 3 cases shared this time, 2 cases were asymptomatic patients and were healthy people before the onset; the other case was a secondary infection based on the original structural lung disease
.
Therefore, early identification and health management of NTM high-risk factors and high-risk groups are important links in the early diagnosis of NTM disease
.
At present, it is believed that the high-risk factors of NTM disease include host factors, drug factors, and environmental factors
.
Host factors mainly refer to people with underlying lung diseases and immunodeficiency.
In addition, studies have shown that rheumatoid arthritis, gastroesophageal reflux, malnutrition, and vitamin D deficiency are also risk factors for NTM disease
.
Drug factors mainly refer to patients who use glucocorticoids and immunosuppressive agents
.
Environmental factors include indoor aerosols and soil dust
.
The characteristic lung CT findings are important clues for the diagnosis of NTM lung disease
.
The domestic research team believes that the characteristic lung CT manifestations mainly include three types: bronchiectasis and nodules-based, cavitation-based, and actualized-to-major [3,5]
.
The first type of lung lesions are mainly bronchiectasis with central nodules in the surrounding lobules, which can be combined with patchy shadows, fibrous striae, cavities and other signs
.
The second type of lung lesions are mainly cavities, which can be combined with patchy shadows, fiber streaks, bronchiectasis, and central lobular nodules
.
The third type is mainly plaque shadows in the lungs and bronchial dissemination foci, which can be combined with signs of bronchiectasis and cavitation
.
The positive results of pathogenic microorganism culture and molecular biology strain identification of respiratory tract or lung tissue specimens are necessary conditions for the diagnosis of NTM lung disease
.
Combining solid culture and liquid culture can help increase the positive rate of NTM culture
.
Different NTM subspecies have different treatment options, so the identification of NTM strains is a guarantee for precise treatment
.
Before starting treatment for NTM disease, its treatment risks, treatment benefits and treatment goals should be fully evaluated
.
During treatment, the efficacy and adverse reactions of anti-NTM drugs need to be closely monitored
.
Among the cases shared this time, one patient adjusted the plan due to drug resistance during the follow-up, and the other changed the plan due to obvious adverse reactions
.
Reference materials: [1] Guidelines for the diagnosis and treatment of non-tuberculous mycobacterial diseases (2020 edition).
Chinese Journal of Tuberculosis and Respiratory Diseases.
2020.
43 (11): 918-946.
[2] Kwak N, Lee CH, Lee HJ, et al .
Non-tuberculous mycobacterial lung disease: diagnosis based on computed tomography of the chest.
Eur Radiol.
2016.
26(12):4449-4456.
[3]Yao Lan, Hao Xiaohui, Tang Shenjie, Liu Yidian, Fang Yuanyuan, Lu Yan.
Analysis of imaging characteristics of 144 cases of nontuberculous mycobacterial lung disease.
Chinese Journal of Tuberculosis and Respiratory Disease.
2012.
35(8):615-616.
[4] Daley CL, Iaccarino JM, Lange C, et al.
Treatment of nontuberculous mycobacterial pulmonary disease :an official ATS/ERS/ESCMID/IDSA clinical practice guideline.
Eur Respir J.
2020.
56 (1).
[5] Chu Naihui, Zhou Wenqiang, Sha Wei.
Expert consensus on the use of drugs for non-tuberculous mycobacterial diseases.
Chinese Journal of Tuberculosis.
2020.
42 (08): 769-787.
[6] Consensus expert group on the differential diagnosis of fever with lung shadow.
Expert consensus on the differential diagnosis of fever with lung shadow.
Chinese Journal of Tuberculosis and Respiration.
2016.
(3): 169-176.
.
In recent years, the incidence of NTM disease has been significantly increasing [1]
.
The clinical manifestations and imaging characteristics of NTM disease are heterogeneous, and the treatment is difficult and the treatment course is long, which brings great challenges to clinical diagnosis and treatment
.
The center has treated a large number of patients with NTM lung disease and has accumulated a lot of experience.
Now we select 3 cases to share with you
.
Case 1: Mycobacterium abscessus pulmonary disease [Basic information] The patient was a 40-year-old middle-aged female, an ordinary worker, and was admitted to the hospital on November 15, 2020 because of "repeated cough and sputum for more than 10 years, and aggravated by 1 month"
.
[Present disease history] 10 years ago, the patient had cough, sputum, yellow and white sputum, and it was difficult to cough up the sputum.
After the illness, he was diagnosed with bronchiectasis and infection in a nearby hospital.
The patient’s symptoms repeatedly appeared in the past 10 years and he was given resistance every time.
The infection gets better after treatment
.
In October 2020, the patient felt that the symptoms of cough and sputum were worse than before.
The sputum was yellow and purulent sputum, which was not easy to cough up, accompanied by fever.
The highest body temperature reached 38.
9℃, without chills or hemoptysis.
Right upper lung bronchiectasis, multiple small nodules and patchy shadows in both lungs, received anti-infection treatment with ceftazidime, levofloxacin and other drugs, body temperature decreased, but there was still obvious cough and sputum
.
[Past history and personal history] Deny the history of infectious diseases such as tuberculosis, and deny the history of high blood pressure and diabetes
.
Denies the history of exposure to dust and poisons
.
Deny the family history of hereditary diseases
.
No history of smoking or alcoholism
.
[Physical examination] No cyanosis of the lips, no shortness of breath in the resting state, slightly lower right upper lung breath sounds, no dry and wet rales in both lungs, heart rate 78 beats/min, regular rhythm
.
The lower limbs are not swollen, and the joints of the limbs are normal
.
[Illness analysis] The patient is a middle-aged woman with a chronic course of disease, long-term cough and sputum; lung imaging manifests as bronchiectasis, multiple small nodules under the pleura, and partial lung tissue structure destruction.
Conventional anti-infective treatment is not effective
.
Analysis of the above-mentioned characteristics of the medical history found that the patient had structural lung disease (bronchiectasis).
Considering that the infection-induced symptoms were aggravated this time.
In view of the fact that the patient has not improved significantly with conventional anti-infective treatment, there are characteristic imaging manifestations [2,3], which needs to be considered.
Infection with atypical pathogens such as mycobacteria
.
The next step in diagnosis and treatment needs to focus on pathogenic microorganisms, especially mycobacterial related tests, and further screening of patients for the cause of bronchiectasis
.
[Preliminary diagnosis] Bronchiectasis with infection, pulmonary mycobacterial disease may be possible
.
[Diagnosis and treatment] After the patient is admitted to the hospital, complete blood routine and blood biochemistry, infection-related markers, sputum pathogenic microorganisms, autoantibodies, high-resolution CT (HRCT), bronchoscopy and alveolar lavage fluid (BALF) microbiological examinations, and give Cefoperazone Sodium and Sulbactam Sodium Empirically Anti-infection, Phlegm Resolving and Symptomatic Treatment
.
▌ The auxiliary examination results are as follows: blood routine: white blood cell count 9.
03×109/L, neutrophil percentage 70.
70%, lymphocyte percentage 18.
80% ↓, eosinophil percentage 1.
00%
.
Inflammation indicators: high-sensitivity C-reactive protein (hCRP) 52.
36mg/L ↑, erythrocyte sedimentation rate (ESR) 42mm/h ↑, procalcitonin (PCT) 0.
02ng/ml
.
Autoantibodies and tumor markers are normal, 1,3-β-D glucan test (G test), galactomannan antigen test (GM test), latex agglutination test negative, tuberculosis infection T cell spot test (T -SPOT) negative
.
Sputum bacteria/fungus/tuberculosis smear + culture result was negative
.
HRCT: bronchiectasis in the upper right lung, combined with cavities and patchy shadows; multiple small nodules in both lungs, mainly under the right pleura (see Figure 1-1)
.
Figure 1-1 Under the bronchoscope, there are more purulent secretions in the bronchus of the right upper lobe.
After aspiration, the lumen is unobstructed.
Alveolar lavage is performed in each segment of the right upper lobe
.
BALF acid-fast bacilli smear 3+, Mycobacterium tuberculosis MPB64 antigen was negative
.
The patient has BALF acid-fast staining positive, BALF Mycobacterium tuberculosis MPB64 antigen is negative, blood T-SPOT is negative, and it is considered that non-tuberculous mycobacteria may be infected.
To further improve mycobacterial culture, BALF microbial second-generation sequencing
.
BALF microbial second-generation sequencing detected Mycobacterium abscessus; solid and liquid Mycobacterium cultures were positive; Mycobacterium sequencing did not detect Mycobacterium tuberculosis complex
.
▌ Final diagnosis: Mycobacterium abscessus lung disease, bronchiectasis with infection (branch expansion after infection)
.
▌ Treatment and outcome: According to domestic and foreign NTM disease diagnosis and treatment guidelines and expert consensus [1,4,5], combined with the experience of the center, formulate the following anti-infection plan
.
Initial stage: Amikacin, cefoxitin intravenously, combined with clarithromycin (500mg bid) orally, the course of treatment is 2 months
.
After treatment, the patient's body temperature continued to be normal, his cough and sputum symptoms improved, and his activity tolerance increased
.
Further drug susceptibility results are reported as follows (see Figure 1-2): Figure 1-2 drug susceptibility results indicate that conventional anti-NTM drugs are resistant, and need to be combined based on clinical experience.
The continuation phase is adjusted as follows: Linezolid (600mg qd ), moxifloxacin (400mg qd), rifapentin (450mg biw), clarithromycin (500mg bid) orally for at least 1 year
.
After treatment, the patient’s symptoms continued to improve, the NTM drug adverse reaction monitoring was not abnormal, the results of re-examination of ESR, CRP, and PCT were normal, and the re-examination of lung CT showed that the lesion was significantly improved (see Figure 1-3)
.
Figure 1-3 Case 2: Mycobacterium Kansas Pulmonary Disease [Basic Information] The patient is a 45-year-old middle-aged female, a company employee, and was admitted to the hospital on January 20th, 2021.
5.
12 due to "physical examination found shadow of the left lower lung"
.
[Present illness history] The patient’s 2021.
4.
14 physical examination showed a shadow of the left lower lung.
At that time, there was no obvious cough, sputum, low fever, night sweats, chest pain, chest tightness, and shortness of breath
.
After that, the patient came to our hospital for further diagnosis and treatment.
A CT examination of the lungs in the outpatient department of the respiratory department of our hospital on May 2021 showed multiple patchy and nodules in the lower lobe of the left lung, and was hospitalized for further diagnosis and treatment
.
[Past history and personal history] Deny the history of infectious diseases such as tuberculosis, and deny the history of high blood pressure and diabetes
.
Denies the history of exposure to dust and poisons
.
Denies the family history of hereditary diseases
.
No history of smoking or alcoholism
.
[Physical examination] No cyanosis of the lips, no shortness of breath, thick breath sounds in both lungs, no dry and wet rales, heart rate 82 beats/min, regular rhythm
.
No swelling of the lower limbs, no abnormalities in the joints of the limbs
.
[Auxiliary examination] Lung CT showed multiple nodules and patchy shadows in the dorsal and basal segments of the left lower lung, accompanied by local bronchiectasis (see Figure 2-1)
.
Figure 2-1 [Analysis of Condition] The patient is a middle-aged female with no obvious respiratory symptoms; lung imaging showed multiple nodules and patchy shadows in the dorsal and basal segments of the left lower lung, accompanied by local bronchiectasis
.
Analyzing the characteristics of the above medical history, it is found that the patient has characteristic imaging findings[2,3], and mycobacterial infection needs to be considered first.
In addition, it needs to be differentiated from slow-growing pathogens (cryptococcus, etc.
) infectious diseases, and non-infectious diseases.
Differentiate it from tumor diseases, connective tissue disease, lung involvement, idiopathic interstitial pneumonia (RB-ILD, etc.
) [6]
.
The next step in diagnosis and treatment needs to focus on pathogenic microorganisms, especially mycobacteria related tests, and further screening of the causes of lung shadows in patients is required
.
[Preliminary diagnosis] Pulmonary shadow: Pulmonary mycobacterial disease may be
.
[Diagnosis and treatment] After the patient is admitted to the hospital, complete blood routine and blood biochemistry, infection-related markers, sputum pathogenic microorganisms, autoantibodies, HRCT, BALF microorganisms and other examinations
.
▌ The auxiliary examination results are as follows: blood routine: white blood cell count 7.
12×109/L, neutrophil percentage 55%, lymphocyte percentage 23.
8%, eosinophil percentage 10.
5% ↑
.
Inflammation indicators: hCRP, ESR, PCT normal range
.
The results of autoantibodies and tumor markers were normal, and the G test, GM test, and latex agglutination test were negative
.
T-SPOT: The actual release level of γ-interferon (TN)> 10IU/ml ↑, the specific cellular immune response of Mycobacterium tuberculosis was detected ↑
.
Sputum bacteria/fungus/tuberculosis smear + culture result was negative
.
HRCT: Multiple nodules and patchy shadows in the dorsal and basal segments of the left lower lung, accompanied by local bronchiectasis (see Figure 2-1)
.
No obvious abnormalities were found under the bronchoscope
.
Alveolar lavage was performed on the dorsal and basal segments of the lower lobe of the left lung .
The BALF acid-fast bacilli smear was negative, and the Mycobacterium tuberculosis MPB64 antigen was negative
.
The patient's blood was T-SPOT positive, but BALF acid-fast staining was negative, and BALF Mycobacterium tuberculosis MPB64 antigen was negative.
Considering the possibility of non-tuberculous mycobacterial infection, the mycobacterial culture was further improved, and BALF microbial second-generation sequencing
.
BALF microbial second-generation sequencing detected Mycobacterium Kansas; solid and liquid Mycobacterium cultures were positive; Mycobacterium sequencing did not detect Mycobacterium tuberculosis complex
.
▌ Final diagnosis: Mycobacterium kansas lung disease
.
▌ Treatment and outcome: Mycobacterium kansas is mostly sensitive to rifampicin, and is the core treatment drug for mycobacterium kansas lung disease.
According to domestic and foreign NTM disease diagnosis and treatment guidelines and expert consensus [1,4,5], combined with the experience of our center , Formulate the following anti-infection plan
.
Treatment plan: isoniazid (300mg qd), rifampicin (450mg qd), ethambutol (750mg qd), clarithromycin (500mg bid) orally, and the course of treatment is at least 1 year
.
After treatment, the patient has no obvious discomfort and well tolerated.
The NTM drug adverse reaction monitoring has no obvious abnormalities.
The recent reexamination of lung CT revealed obvious absorption of the lesion (see Figure 2-2)
.
Figure 2-2 Case 3: Mycobacterium avium pulmonary disease [Basic information] The patient is a middle-aged and elderly woman, a retired worker, and was admitted to the hospital on March 29, 2020 because of "the shadow of both lungs was found for more than 2 months"
.
[Present illness history] In January 2021, the patient swallowed shrimp shells and caused sore throat.
The laryngoscopy at the otolaryngology department of the outside hospital showed no obvious abnormalities.
Perfect chest CT revealed multiple nodules in both lungs and lungs.
Then in January On the 19th, I went to the outpatient department of the Respiratory Department of our hospital.
A CT scan of the chest showed multiple patchy and speckled shadows in both lungs, and the right lung was the main one
.
The outpatient department perfected blood T-SPOT, sputum tuberculosis smear, sputum tuberculosis culture, bacterial typing, DNA sequencing and other examinations, and no abnormalities were found
.
During the period, the patient had no cough and sputum, no low-grade fever and night sweats, no chest tightness, shortness of breath, no hemoptysis and other discomforts.
He was admitted to the hospital for further diagnosis and treatment
.
Since the onset of the illness, the patient has been mentally well, appetite, sleep, and normal urine and feces, no significant decrease in physical strength, and no significant decrease in weight
.
[Past history and personal history] Deny the history of infectious diseases such as tuberculosis, and deny the history of high blood pressure and diabetes
.
Denies the history of exposure to dust and poisons
.
Deny the family history of hereditary diseases
.
No history of smoking or alcoholism
.
[Physical examination] No cyanosis of the lips, no shortness of breath, thick breath sounds in both lungs, no dry and wet rales, heart rate 85 beats/min, regular rhythm
.
The lower limbs are not swollen, and the joints of the limbs are normal
.
[Auxiliary examination] CT of the lungs showed multiple patchy and speckled shadows in both lungs, with the right lung predominantly (see Figure 3-1)
.
Figure 3-1 [Analysis of the condition] The patient is a middle-aged and elderly woman with no obvious respiratory symptoms; lung imaging showed multiple patchy and speckled shadows in both lungs, mainly in the right lung
.
Analysis of the above-mentioned characteristics of the medical history found that the patient has characteristic imaging findings[2,3], and mycobacterial infection must be considered first, the sputum microbiological test result is negative, and the blood T-SOPT result is negative, so consider the possibility of NTM infection
.
The next step in diagnosis and treatment needs to improve bronchoscopy and BALF microbiological examination, focusing on pathogenic microorganisms, especially NTM-related testing, and further screening of patients with other causes of lung shadows
.
[Preliminary diagnosis] Lung shadow: non-tuberculous mycobacterial lung disease may be possible
.
[Diagnosis and treatment] After the patient is admitted to the hospital, complete blood routine and blood biochemistry, infection-related markers, sputum pathogenic microorganisms, autoantibodies, HRCT, BALF microorganisms and other examinations
.
▌ The auxiliary examination results are as follows: blood routine: white blood cell count 6.
06×109/L, neutrophil percentage 66%, lymphocyte percentage 24.
4%, eosinophil percentage 2.
3%
.
Inflammation indicators: hCRP, ESR, PCT normal range
.
The results of autoantibodies and tumor markers were normal, and the G test, GM test, and latex agglutination test were negative
.
T-SPOT: negative
.
Sputum bacteria/fungus/tuberculosis smear + culture result was negative
.
HRCT: There are multiple patchy and speckled shadows in both lungs, with the right lung predominantly (see Figure 3-1)
.
A small amount of purulent secretions in the middle lobe of the right lung was seen under the bronchoscope
.
After aspiration, the lumen was unobstructed, and bronchoalveolar lavage was performed in the lateral segment of the middle lobe of the right lung .
BALF acid-fast bacilli smear 4+, Mycobacterium tuberculosis MPB64 antigen was negative
.
The patient had BALF acid-fast staining positive, blood T-SPOT negative, and BALF Mycobacterium tuberculosis MPB64 antigen negative.
Considering the possibility of non-tuberculous mycobacterial infection, the mycobacterial culture should be further improved, and BALF microbial second-generation sequencing
.
BALF microbial second-generation sequencing detected Mycobacterium avium complex; solid and liquid Mycobacterium cultures were positive; Mycobacterium sequencing did not detect Mycobacterium tuberculosis complex
.
▌ Final diagnosis: Mycobacterium avium lung disease
.
▌ Treatment and outcome: Mycobacterium avium is one of the subspecies of MAC.
Studies have shown that the efficacy and safety of treatments containing macrolides are good
.
The BALF acid-fast staining of this patient is strongly positive.
According to domestic and foreign NTM disease diagnosis and treatment guidelines and expert consensus [1,4,5], combined with the experience of the center, the following anti-infection plan was formulated
.
Treatment plan: Azithromycin (500mg qd), isoniazid (300mg qd), rifampicin (450mg qd), ethambutol (750mg qd) orally, the course of treatment is at least 1 year
.
The patient had no obvious discomfort in the initial treatment stage.
After 1 month of treatment, the patient developed anorexia and belching.
In 2021.
5.
11, due to increased diarrhea, anorexia, and fatigue, he re-visited the doctor, improved sputum microbiology, lung CT and other examinations, and provided stomach protection and symptomatic treatment
.
The results of the examination indicated sputum acid-fast staining (+), lung CT indicated earlier absorption of lung lesions (see Figure 3-2), and gastroscopy indicated chronic gastritis and mild reflux esophagitis
.
Figure 3-2 Condition analysis: The patient’s imaging and other examination results indicate that the treatment is effective, but there are obvious adverse reactions of anti-NTM drugs.
In view of the positive staining of sputum acid-fast, it is necessary to continue anti-NTM treatment.
The treatment plan is adjusted as follows
.
Anti-NTM regimen: clarithromycin (500mg bid), isoniazid (300mg qd), rifapentine (600mg biw), ethambutol (750mg qd) orally
.
Treatment of adverse gastrointestinal reactions: gastric mucosal protective agents and acid inhibitors, gastrointestinal motility drugs
.
After adjusting the treatment plan, the patient has no obvious discomfort, and the NTM drug adverse reaction monitoring has no obvious abnormality.
Currently, he is closely followed up
.
★Comments from experts: Dr.
Zhang Peng, Department of Respiratory and Critical Care Medicine, Shanghai Public Health Clinical Center, NTM lung disease is the most common type of NTM disease, and the incidence in China has been significantly increasing in recent years
.
Early identification and correct diagnosis are essential to reduce transmission, increase cure rate, and reduce resistance rate
.
The clinical manifestations of patients with NTM lung disease are multifaceted, and some patients have no obvious symptoms at the onset of the disease
.
Of the 3 cases shared this time, 2 cases were asymptomatic patients and were healthy people before the onset; the other case was a secondary infection based on the original structural lung disease
.
Therefore, early identification and health management of NTM high-risk factors and high-risk groups are important links in the early diagnosis of NTM disease
.
At present, it is believed that the high-risk factors of NTM disease include host factors, drug factors, and environmental factors
.
Host factors mainly refer to people with underlying lung diseases and immunodeficiency.
In addition, studies have shown that rheumatoid arthritis, gastroesophageal reflux, malnutrition, and vitamin D deficiency are also risk factors for NTM disease
.
Drug factors mainly refer to patients who use glucocorticoids and immunosuppressive agents
.
Environmental factors include indoor aerosols and soil dust
.
The characteristic lung CT findings are important clues for the diagnosis of NTM lung disease
.
The domestic research team believes that the characteristic lung CT manifestations mainly include three types: bronchiectasis and nodules-based, cavitation-based, and actualized-to-major [3,5]
.
The first type of lung lesions are mainly bronchiectasis with central nodules in the surrounding lobules, which can be combined with patchy shadows, fibrous striae, cavities and other signs
.
The second type of lung lesions are mainly cavities, which can be combined with patchy shadows, fiber streaks, bronchiectasis, and central lobular nodules
.
The third type is mainly plaque shadows in the lungs and bronchial dissemination foci, which can be combined with signs of bronchiectasis and cavitation
.
The positive results of pathogenic microorganism culture and molecular biology strain identification of respiratory tract or lung tissue specimens are necessary conditions for the diagnosis of NTM lung disease
.
Combining solid culture and liquid culture can help increase the positive rate of NTM culture
.
Different NTM subspecies have different treatment options, so the identification of NTM strains is a guarantee for precise treatment
.
Before starting treatment for NTM disease, its treatment risks, treatment benefits and treatment goals should be fully evaluated
.
During treatment, the efficacy and adverse reactions of anti-NTM drugs need to be closely monitored
.
Among the cases shared this time, one patient adjusted the plan due to drug resistance during the follow-up, and the other changed the plan due to obvious adverse reactions
.
Reference materials: [1] Guidelines for the diagnosis and treatment of non-tuberculous mycobacterial diseases (2020 edition).
Chinese Journal of Tuberculosis and Respiratory Diseases.
2020.
43 (11): 918-946.
[2] Kwak N, Lee CH, Lee HJ, et al .
Non-tuberculous mycobacterial lung disease: diagnosis based on computed tomography of the chest.
Eur Radiol.
2016.
26(12):4449-4456.
[3]Yao Lan, Hao Xiaohui, Tang Shenjie, Liu Yidian, Fang Yuanyuan, Lu Yan.
Analysis of imaging characteristics of 144 cases of nontuberculous mycobacterial lung disease.
Chinese Journal of Tuberculosis and Respiratory Disease.
2012.
35(8):615-616.
[4] Daley CL, Iaccarino JM, Lange C, et al.
Treatment of nontuberculous mycobacterial pulmonary disease :an official ATS/ERS/ESCMID/IDSA clinical practice guideline.
Eur Respir J.
2020.
56 (1).
[5] Chu Naihui, Zhou Wenqiang, Sha Wei.
Expert consensus on the use of drugs for non-tuberculous mycobacterial diseases.
Chinese Journal of Tuberculosis.
2020.
42 (08): 769-787.
[6] Consensus expert group on the differential diagnosis of fever with lung shadow.
Expert consensus on the differential diagnosis of fever with lung shadow.
Chinese Journal of Tuberculosis and Respiration.
2016.
(3): 169-176.