-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*Only for medical professionals to read for reference, lung cancer patients usher in more choices and hopes
.
On July 2-3, 2021, the Chinese Society of Clinical Oncology (CSCO) and Beijing Xisk Clinical Oncology Research Foundation co-sponsored the "2021 China Clinical Oncology Annual Progress Seminar (BOC) and Best of ASCO 2021 China "Successfully held
.
After the meeting, "Medical Oncology Channel" invites Professor Chu Qian from Tongji Hospital of Tongji Medical College of Huazhong University of Science and Technology to be a guest of "Famous Doctor Kungfu Tea" to talk about the important progress of non-small cell lung cancer (NSCLC) targeted therapy and its significance for clinical practice in China
.
What should I do if MET amplification triggers EGFR-TKI resistance? In recent years, the clinical application of EGFR tyrosine kinase inhibitors (EGFR-TKI) has brought huge breakthroughs and opened the way for precise treatment of NSCLC
.
However, patients are prone to drug resistance after receiving EGFR-TKI treatment, and MET amplification is one of the important resistance mechanisms
.
Professor Chu Qian said, “For the first, second, and third-generation EGFR-TKIs, MET amplification is one of the very important resistance mechanisms.
Among the third-generation EGFR-TKI-resistant populations, the proportion of MET amplification is even as high as 20 %~25%
.
Therefore, choosing the right MET inhibitor for the EGFR-TKI resistant population has become a problem that needs to be carefully considered in clinical practice
.
The INSIGHT study [1] published by Professor Wu Yilong’s team in 2020 shows that gefitinib Combined with the MET inhibitor Tepotinib, there is a significant effect in the treatment of patients with MET amplification
.
In the future, we can expect that the combination of EGFR-TKI and MET inhibitors will bring new survival benefits for such resistant patients
.
"However, no drugs for MET amplification have been approved for marketing in China.
For patients with MET amplification, how should the drug regimen be selected in clinical practice? In this regard, Professor Chu Qian explained, "In fact, there are two drugs to choose from, but These two drugs are currently super-indication drugs
.
The first is crizotinib, which is a multi-target TKI, and MET is also one of its targets
.
Therefore, for patients with drug resistance caused by MET amplification, we can choose EGFR-TKI combined with crizotinib
.
The second is Saivotinib.
On June 22 this year, the National Medical Products Administration (NMPA) of China approved Saivotinib as a specific targeted drug for patients with MET14 exon jumping mutations, so we can also choose to combine Use EGFR-TKI and Sevotinib
.
"" Both of these programs are effective programs, but today as more and more attention is paid to indication medication, all colleagues in the same industry must pay attention to it.
When medication is used, it is necessary to explain to patients and family members the super-indication medication.
Reason and purpose
.
"Professor Chu Qian emphasized
.
MET inhibitors open a new door to survival for patients with pulmonary sarcomatoid cancer.
In addition to MET gene amplification, MET14 exon skip mutation is also a more common form of MET gene mutation
.
MET14 exon skip mutation is A retrospective study has shown that the incidence of MET14 exon skipping mutations in Chinese patients with pulmonary sarcomatoid carcinoma is 20.
8%-22%
.
And compared with other NSCLC subtypes, Patients with pulmonary sarcomatoid carcinoma have a poor prognosis and fewer treatment options
.
Professor Chu Qian said, “Previously, the treatment options that Chinese patients with pulmonary sarcomatoid cancer can accept are very limited, and the guidelines do not specify their standard treatment options.
The effective rate of chemotherapy is relatively low, and immunotherapy and anti-angiogenesis therapy are still in place.
Initial exploration stage
.
With the launch of Sevotinib, the treatment of pulmonary sarcomatoid cancer in China has entered a new chapter
.
For patients with pulmonary sarcomatoid cancer with MET14 exon jumping mutations, Saivotinib has become the first-line treatment of choice
.
" In the pivotal registered clinical study of Syvotinib led by Professor Lu Shun [2], 70 patients with MET14 exon jumping mutations were included, of which 25 patients (35.
7%) were pulmonary sarcomatoid carcinomas and had a baseline Fifteen patients (21%) had brain metastases
.
After the patients were treated with Syvotinib, among 61 patients with evaluable tumors, the objective response rate (ORR) assessed by the Independent Evaluation Committee (IRC) was 49.
2%, and the disease control rate (DCR) reached 93.
4%; Among patients with pulmonary sarcomatoid carcinoma, the ORR assessed by IRC was 40%, the median time to remission was 17.
9 months, and the median progression-free survival (PFS) was 5.
5 months
.
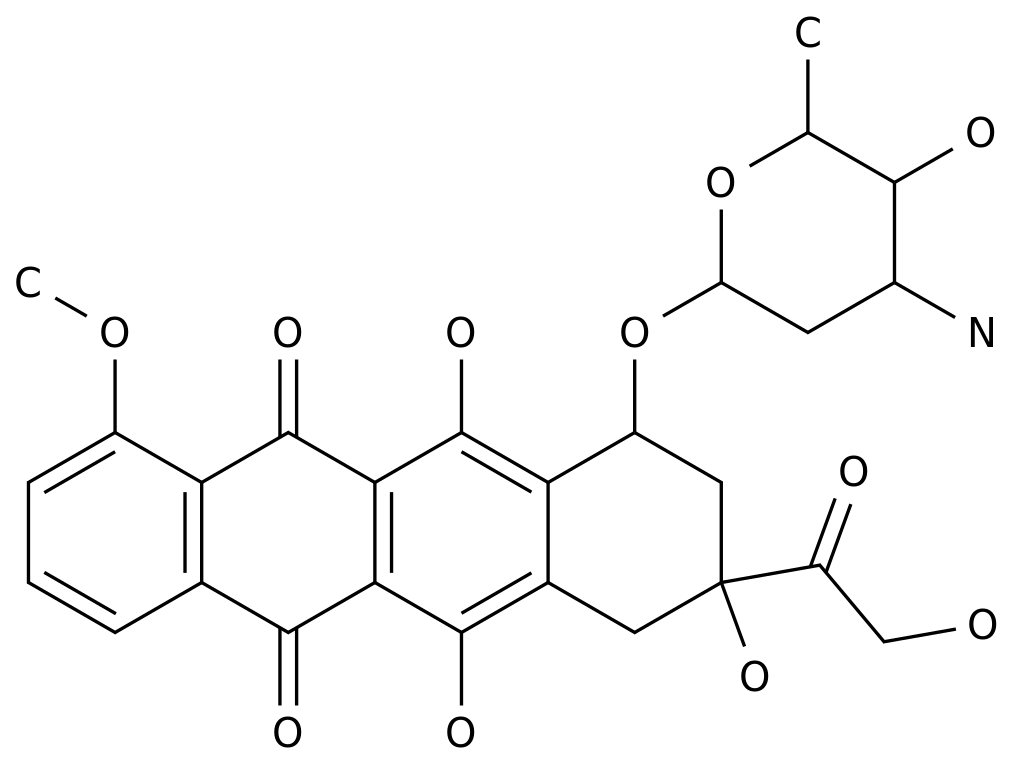
Figure 1: The efficacy results of the Phase II study of Syvotinib "This is the most eye-catching data for the treatment of pulmonary sarcomatoid cancer
.
" Professor Chu Qian said happily
.
"In addition, if we look at the overall population of MET14 exon skip mutations, Tepotinib and camatinib also perform well
.
Therefore, MET inhibitors open a new door to survival for patients with MET14 exon skip mutations.
.
one of the common causes of "ALK positive treatment of brain metastases with new tactics, a variety of ALK-TKI offers a rich selection of clinical lung cancer brain metastases clinical more common, but also lung cancer treatment failure
.
Compared with patients with positive driver genes, ALK-positive NSCLC patients have a higher chance of brain metastasis
.
In recent years, there have been frequent hot spots in the treatment of ALK-positive NSCLC, and a variety of new drugs and treatment options have emerged
.
So, for ALK-positive NSCLC patients with brain metastases, what are the current effective treatment options? Professor Chu Qian shared, “This problem can be explained from two levels
.
First, for patients with brain metastases at baseline, there are 4 drugs that can be selected for first-line treatment
.
The
first is aletinib, the ALEX study, The J-ALEX study and the Chinese real-world study data just released this year both show that aletinib has a very good control effect on intracranial lesions
.
The second is ceritinib
.
The
ASCEND-4 study shows that there is brain at baseline After receiving ceritinib treatment, patients with metastases have a median PFS of 10.
7 months, which is significantly longer than crizotinib
.
The
third type is brigatinib
.
Clinical studies have shown that patients with brain metastases at baseline received After treatment with brigatinib, the median intracranial progression-free survival (iPFS) can reach two years, which is the brightest data available for brain metastases among all ALK-TKIs
.
The
fourth type is lauratide .
Nepal
.
CROWN baseline study on patients with brain metastases were iPFS determination, as of now, azole grams of imatinib group has a clear data, and Laura imatinib set of data is not yet mature, from the trend, the study will It is a positive outcome
.
In addition, for patients with brain metastases after chemotherapy or crizotinib treatment, the main drugs that have achieved good results in the current posterior treatment are ceritinib, aletinib and loratinib
.
For patients with brain metastases after crizotinib treatment, the ORRs of ceritinib, aletinib and loratinib were 35%, 47.
8% and 87% in second-line treatment, especially loratinib.
The curative effect of its intracranial control rate is amazing
.
"Therefore, for patients with ALK-positive and brain metastases, there are already very rich clinical options for first-line and second-line treatments.
The drugs that can be selected are mainly concentrated on the second and third generation ALK-TKIs
.
"Professor Chu Qian concluded
.
A
new generation of detection technology helps RET gene fusion detection and precision treatment.
Among the rare types of NSCLC gene mutations, RET gene fusion has attracted much attention
.
In the
past two years, there have been successive targets for RET gene fusion at home and abroad .
approved drugs on the market and the effect is significant, bringing new hope for patients
.
patients with NSCLC RET fusion of relatively low incidence, but the population at Chinese patients with lung cancer, it is the real world RET fusion positive number of patients with lung cancer are still many
.
for This part of patients needs to be screened out and targeted for treatment
.
So, what are the currently recommended RET gene fusion testing standards and methods? Professor Chu Qian introduced, "The current clinical methods for detecting RET gene fusion mainly include reversal Record polymerase chain reaction (RT-PCR), fluorescence in situ hybridization (FISH) and next-generation gene sequencing (NGS)
.
RT-PCR has good specificity, but it can only detect the fusion of known sites, and is not capable of detecting new sites, so it is rarely used in clinical practice
.
FISH is the gold standard for RET fusion testing, but FISH testing is more expensive and requires interpretation by pathologists, so it is not suitable for all institutions
.
NGS can detect the fusion of unknown sites, and also has very high sensitivity and specificity for small specimens, so it has a wide range of clinical applications
.
But NGS also has certain limitations.
First, NGS testing is expensive; second, how to correctly interpret NGS reports is still a difficult problem faced by testing companies or hospital testing platforms
.
"We need to work hard to promote FISH and NGS in the clinic, and choose appropriate drugs for patients based on the test results
.
"Professor Chu Qian further added
.
Click to watch the wonderful video of BOC/BOA on-site expert profile.
Prof.
Qian Chu, Deputy Director, Department of Thoracic Oncology, Tongji Hospital Affiliated to Tongji Medical College, Huazhong University of Science and Technology, Professor, Chief Physician, Doctoral Supervisor, Member of the Chinese Society of Clinical Oncology Expert Committee on Non-small Cell Lung Cancer, Chinese Clinical Oncology Member of the Standing Committee of the Society of Immunotherapy Experts Committee Deputy Secretary-General of the Patient Education Expert Committee of the Chinese Society of Clinical Oncology Standing Director of the China Healthcare International Exchange Promotion Association Chairman of the Youth Expert Committee of the Hubei Society of Clinical Oncology Chairman of the Committee of Immunotherapy Experts of the Hubei Provincial Society of Clinical Oncology Hubei Reference materials for the appointed chairman of the Provincial Committee of Tumor Precision Therapy of the Provincial Society of Immunology: [1] Wu YL, Cheng Y, Zhou J, et al.
Tepotinib plus gefitinib in patients with EGFR-mutant non-small-cell lung cancer with MET overexpression or MET amplification and acquired resistance to previous EGFR inhibitor (INSIGHT study): an open-label, phase 1b/2, multicentre, randomised trial.
Lancet Respir Med.
2020;8(11):1132-1143.
[2]Lu S, Fang J, Li X, et al.
Once-daily savolitinib in Chinese patients with pulmonary sarcomatoid carcinomas and other non-small-cell lung cancers harbouring MET exon 14 skipping alterations: a multicentre, single-arm, open-label, phase 2 study .
Lancet Respir Med.
2021; S2213-2600(21)00084-9.