-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
21-hydroxylase deficiency (21-hydroxylase deficiency, 21-OHD) is the most common type of congenital adrenal hyperplasia (CAH).
It is caused by a defect in the CYP21A2 gene encoding 21-hydroxylase that leads to the adrenal glands.
Corticosteroid hormone synthesis disorder is a congenital disease that is inherited in an autosomal recessive manner.
Adrenal crisis can occur in typical patients, leading to life-threatening; hyperandrogenism makes women virilized, leading to accelerated bone age, short stature, and abnormal youth development, and affect fertility.
Etiology and Epidemiology 21-OHD is caused by mutations in the CYP21A2 gene located in the 6p21.
3 region of chromosome.
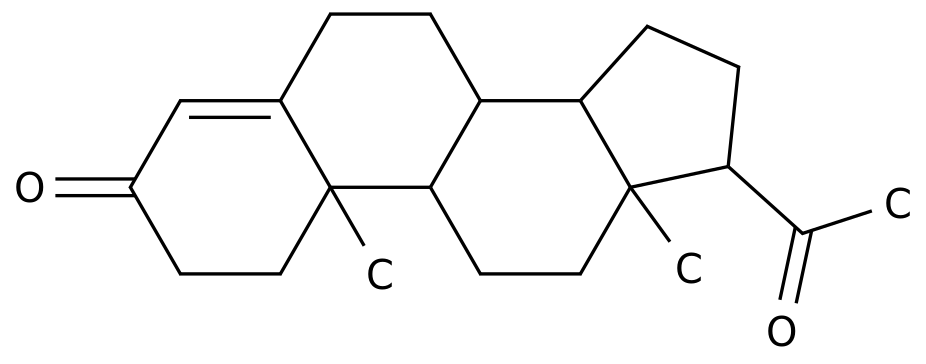
The protein it encodes is 21 hydroxylase (P450c21).
The enzyme catalyzes the conversion of 17-hydroxyprogesterone (17-OHP) to 11-deoxycortisol, and at the same time catalyzes the conversion of progesterone to 11-deoxycortisol, which are the precursors of cortisol and aldosterone, respectively.
Decreased 21 hydroxylase activity leads to impaired synthesis of cortisol and aldosterone.
The synthesis of cortisol levels decreases, and the secretion of ACTH from the pituitary increases through negative feedback, which stimulates the proliferation of adrenal cortex cells; while insufficient aldosterone secretion activates the secretion of upstream renin and angiotensin II.
At the same time, due to the accumulation of intermediate products, it is a sex hormone (in the adrenal cortex).
Mainly for androgen) synthesis provides an abnormally increased substrate, resulting in the characteristic consequence of bypass hypermetabolism-hyperandrogenemia.
The significant degree of androgen increase was androstenedione, testosterone and dehydroepiandrosterone (DHEA) in order.
There are more than one hundred mutation types of CYP21A2 gene, 80% of which are related to genotype and phenotype.
When the mutation causes the 21 hydroxylase activity to be less than 1%, it is manifested as severe salt loss, hyponatremia and hyperkalemia, and neonatal adrenal crisis.
When the residual enzyme activity is 1% to 2%, aldosterone can still be maintained in the normal range, and the tendency to lose salt is low (but it can still occur under stress).
When the enzyme activity is retained at 20% to 50%, the synthesis of cortisol is hardly impaired.
According to the relationship between genotype and clinical phenotype, the degree of aldosterone and cortisol deficiency, and the severity of high androgen, 21-OHD is divided into two major types: ①Classic 21-OHD, which is divided into salt loss type according to the degree of aldosterone deficiency (Salt wasting, SW, about 75%) and simple virilizing (SV, about 25%); ②Non-classical 21-OHD (non classical CAH, NCCAH).
CAH can be divided into multiple types according to the types of defective enzymes.
21-OHD is the most common type, accounting for 90%-95%.
Most studies at home and abroad suggest that the incidence of newborn screening is 1/20000~1/10000.
Clinical manifestations The clinical manifestations of 21-OHD include varying degrees of salt loss and hyperandrogenemia.
Neonatal-onset children have manifestations of varying degrees of adrenal cortex dysfunction, such as weakness, nausea, vomiting, feeding difficulties, diarrhea, chronic dehydration, skin pigmentation, and growth retardation.
Adrenal crisis is often the first manifestation of 21-OHD SW in the neonatal period.
It is manifested as severe hyponatremia, hyperkalemia, hypovolemic shock, and may be accompanied by hypoglycemia, induced by stress.
Severe hyponatremia can cause central nervous system manifestations such as convulsions, and severe hyperkalemia can cause fatal arrhythmias.
Hyperandrogenemia manifests differently at different ages.
Female children with typical 21-OHD have different degrees of virilization in their external genitalia at birth.
Mild cases show isolated clitoral hypertrophy.
In severe cases, the external genitalia can be close to men, the labia majora is scrotal-like, the clitoris is hypospadias-like penis, and it has a common urethral vagina.
However, the gonads cannot be touched in the labia majora, and there is a completely normal female internal genital structure (ovaries and uterus).
Males may have no external genital abnormalities such as penis enlargement during neonatal and infancy, which is a common reason for delayed diagnosis.
In early childhood, both sexes will show peripheral precocious puberty.
Boys have enlarged penis with or without premature appearance of pubic hair; female children have heterosexual precocious puberty.
Long-term high levels of sex hormones stimulate hypothalamic gonadotropin releasing hormone (GnRH) neurons to develop central precocious puberty.
Women may also have secondary sexual characteristics dysplasia and primary amenorrhea or oligomenorrhea.
The non-classical 21-OHD is only diagnosed as 21-OHD when it is suspected of being diagnosed as polycystic ovary syndrome in adolescence or adulthood.
Both sexes begin to grow linearly and accelerate the growth of bone age in their infancy, which impairs lifelong height.
Other manifestations include darkening of the skin and mucous membranes, with the areola and vulva as the main manifestations.
Some children may have no such changes.
NCCAH has clinical manifestations of different degrees of hyperandrogenism in childhood, adolescence and even adulthood, and only manifests as growth acceleration and rapid progress in bone age.
Auxiliary examination 1.
Elevated serum 17-OHP 17-OHP is a specific diagnostic index and main treatment monitoring index for 21-OHD.
Generally speaking, the higher the 17-OHP increase, the more severe the degree of enzyme deficiency.
However, 17-OHP and ACTH are both stress hormones.
Therefore, when there is stress, or when the child draws blood and crying severely, it can be significantly higher than the actual level.
This should be considered when interpreting the results.
factor.
2.
Basic serum cortisol and ACTH The serum cortisol of typical patients decreases with ACTH increase.
There are also 21-OHD patients with cortisol in the normal range, while ACTH is elevated, which requires a comprehensive judgment in conjunction with other indicators.
The two hormones of 21-OHD non-classical patients are basically in the normal range.
3.
Androgen The measured value of each androgen should be judged according to the normal reference value established by sex, age and puberty.
Androstenedione has a good correlation with 17-OHP, and the diagnostic and monitoring significance is the best.
DHEAS can also be elevated in polycystic ovary syndrome.
4.
Plasma renin concentration or renin activity, angiotensin II and aldosterone.
Renin is elevated in the 21-OHD SW type, but the diagnostic specificity is not high.
Renin can also be elevated in some patients with non-salt-loss type, and renin is an important monitoring indicator in mineralocorticoid replacement therapy.
Low aldosterone supports the diagnosis of salt loss, but serum aldosterone can be normal in a quarter of children.
5.
Chromosomes Chromosomes are mainly used to exclude 46, XY sexual dysplasia diseases.
6.
Imaging The B-ultrasound and CT imaging examinations of the adrenal glands are helpful for the identification of adrenal tumors or other adrenal (dysplasia) lesions.
Women should complete the uterus, double-attachment B-ultrasound, and check the bone age from the age of 2 years.
7.
Genetic Diagnosis The genetic diagnosis of 21-OHD is very important for the differential diagnosis with clear or unclear biochemical diagnosis, and it is also very important for genetic counseling to be able to diagnose heterozygous carriers.
Diagnosis 21-OHD diagnosis requires comprehensive clinical manifestations, including 17-OHP and the concentration of each relevant hormone to be judged, genetic testing can further confirm the diagnosis.
At present, 21-OHD neonatal screening has been carried out in many areas in China.
For those who are positive for 17-OHP in heel blood screening, they need to follow the screening consensus.
Serum cortisol in NCCAH patients is normal or at the lower limit of normal.
ACTH is normal or critically high.
Diagnosis with 17-OHP basic value is uncertain, and genetic testing is extremely important.
Differential diagnosis The common diseases that need to be differentiated from 21-OHD include: 1.
11β-hydroxylase deficiency (CYP11B1 gene mutation) and hyperandrogenism, very few manifestations of salt loss at birth, and common mineralocorticoids such as water and sodium.
Retention, hypokalemia and hypertension, etc.
, low renin-angiotensin levels, elevated progesterone and 17-OHP.
However, blood pressure in some patients can be normal, and genetic testing and 21-OHD identification are required if necessary.
2.
17α-hydroxylase deficiency (CYP17A1 gene mutation) This enzyme also has 17,20-lyase activity, and its clinical manifestations are symptoms of increased mineralocorticoids, such as hypokalemia, hypertension, and insufficient sex hormones.
, Such as lack of female youth development, male feminization.
Progesterone is elevated, 17-OHP is reduced or normal.
3.
Congenital hereditary adrenal dysplasia is due to the NR0B1 gene or SF1 gene mutations caused congenital adrenal hypofunction, which can be combined with hypogonadism, and its imaging is mostly manifested as adrenal dysplasia.
4.
Adrenocortical tumors Adrenal cortical tumors (especially in children) often start with the clinical manifestations of hyperandrogenemia, with or without hypercortisolism, and even a significant increase in 17-OHP, but a significantly lower ACTH is the main point of differentiation .
Imaging confirmed the space-occupying lesions.
5.
Polycystic ovary syndrome.
For female patients who see a doctor due to menstrual disorders or hyperandrogenism in adolescence or adulthood, the performance of NCCAH can overlap with that of polycystic ovary syndrome, and polycystic ovary syndrome can also cause DHEAS.
Elevated, can be identified by the medium-dose dexamethasone inhibition test, if necessary, CYP21A2 gene testing to confirm the diagnosis.
Treatment 1.
Treatment goals Develop treatment goals according to different types of 21-OHD.
The treatment goals include replacing the physiological requirements of glucocorticoids, while reasonably inhibiting hyperandrogenism, restoring the trajectory of normal growth and development as much as possible, achieving the ideal lifelong height, and improving long-term reproductive health.
2.
Glucocorticoid therapy Hydrocortisone is the basic medication and requires lifelong replacement therapy. It is recommended to formulate a plan according to the patient's still growing and reaching adult height.
For those who have not stopped growing, it is recommended to use hydrocortisone instead.
After reaching adult height, drugs with a relatively long half-life, such as prednisone or dexamethasone, can be given.
Hydrocortisone replacement therapy programs need to establish an individualized program based on the principles of pharmacokinetics.
The dose is set according to age, administered in divided doses, and the dose is adjusted according to monitoring.
The dosage and schedule of alternative treatment should be individually set according to age and developmental period, and should be controlled at the lowest effective dosage as much as possible to avoid excessive growth inhibition and the occurrence of iatrogenic Cushing’s syndrome.
The dosage of glucocorticoids needs to be adjusted during stress and disease.
The general dosage of hydrocortisone for children is 10-15mg/m^2, 3 times a day; for adults, 15-25mg/d, 2~3 times a day.
3.
Mineralocorticoid treatment It is necessary to adjust the dosage in time to avoid the occurrence of iatrogenic hypertension by paying attention to the age change law of salt hormone sensitivity while preventing salt loss crisis.
21-OHD salt-loss type combined with mineralocorticoids on the basis of glucocorticoids can reduce the total amount of glucocorticoids and long-term adverse reactions.
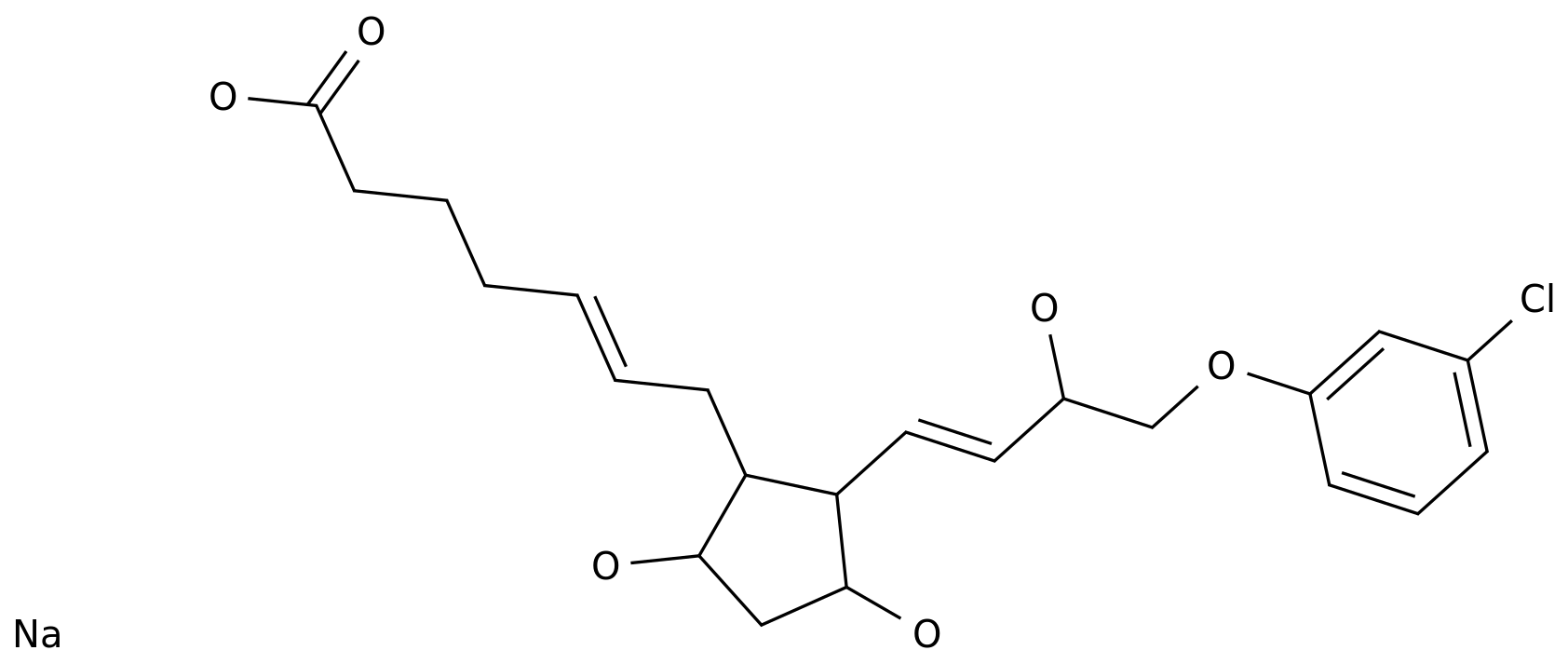
Fludrocortisone is currently the only mineralocorticoid preparation, which can be taken 1 to 2 times a day.
The dosage is set according to the age change rule of sensitivity to mineralocorticoid, and the dosage is adjusted according to monitoring.
As there is no single hormone for judging the curative effect and the "gold standard" for a fixed cut point, it is recommended to combine hormones and clinical indicators to monitor comprehensive judgments to achieve the most ideal goal of individualized treatment.
The general dosage of fludrocortisone for children is 0.
05-0.
2mg/d, 1 to 2 times a day; for adults, the dosage is 0.
05-0.
2mg/d, orally once a day.
4.
Growth hormone and gonadotropin-releasing hormone analogues For those with severe precocious puberty, significantly advanced bone age, and predicted adult height loss, growth hormone therapy may be considered. For patients who have developed central precocious puberty, gonadotropin-releasing hormone analogs can be combined.
However, the improvement of life-long height of these drugs is related to the control of the patient's primary disease, the treatment response to the drug, the degree of advancement of the bone age, and the genetic height of the parents.
Therefore, the treatment effect varies greatly among individuals.
Complication monitoring needs to ask patients about their symptoms regularly during treatment, including symptoms of insufficient replacement of glucocorticoids and mineralocorticoids, such as anorexia, fatigue, dizziness, etc.
, whether there is any recent stress and adrenal crisis.
Ask if there are symptoms of excessive replacement, such as bulimia, weight gain, weakness, etc.
Monitor blood pressure, electrolytes, blood sugar, ACTH, 17-OHP, testosterone, androstenedione, renin concentration or renin activity, angiotensin II, LH, FSH, etc.
to evaluate the control of primary disease, adjust glucocorticoids and salts The dose of corticosteroids.
In addition, it is also necessary to pay attention to the adverse effects of long-term treatment with glucocorticoids such as glucose and lipid metabolism and bone density.
For male patients, the testicular residual adrenal tumors (TARTs) should be regularly monitored for patients over 8 years of age.
TARTs have a greater impact on the spermatogenesis of 21-OHD male patients.
Figure 1 21-hydroxylase deficiency diagnosis and treatment process The above content is extracted from: The National Health Commission of the People's Republic of China.
Guidelines for the diagnosis and treatment of rare diseases (2019 edition) [J].
The official website of the National Health Commission of the People's Republic of China.
It is caused by a defect in the CYP21A2 gene encoding 21-hydroxylase that leads to the adrenal glands.
Corticosteroid hormone synthesis disorder is a congenital disease that is inherited in an autosomal recessive manner.
Adrenal crisis can occur in typical patients, leading to life-threatening; hyperandrogenism makes women virilized, leading to accelerated bone age, short stature, and abnormal youth development, and affect fertility.
Etiology and Epidemiology 21-OHD is caused by mutations in the CYP21A2 gene located in the 6p21.
3 region of chromosome.
The protein it encodes is 21 hydroxylase (P450c21).
The enzyme catalyzes the conversion of 17-hydroxyprogesterone (17-OHP) to 11-deoxycortisol, and at the same time catalyzes the conversion of progesterone to 11-deoxycortisol, which are the precursors of cortisol and aldosterone, respectively.
Decreased 21 hydroxylase activity leads to impaired synthesis of cortisol and aldosterone.
The synthesis of cortisol levels decreases, and the secretion of ACTH from the pituitary increases through negative feedback, which stimulates the proliferation of adrenal cortex cells; while insufficient aldosterone secretion activates the secretion of upstream renin and angiotensin II.
At the same time, due to the accumulation of intermediate products, it is a sex hormone (in the adrenal cortex).
Mainly for androgen) synthesis provides an abnormally increased substrate, resulting in the characteristic consequence of bypass hypermetabolism-hyperandrogenemia.
The significant degree of androgen increase was androstenedione, testosterone and dehydroepiandrosterone (DHEA) in order.
There are more than one hundred mutation types of CYP21A2 gene, 80% of which are related to genotype and phenotype.
When the mutation causes the 21 hydroxylase activity to be less than 1%, it is manifested as severe salt loss, hyponatremia and hyperkalemia, and neonatal adrenal crisis.
When the residual enzyme activity is 1% to 2%, aldosterone can still be maintained in the normal range, and the tendency to lose salt is low (but it can still occur under stress).
When the enzyme activity is retained at 20% to 50%, the synthesis of cortisol is hardly impaired.
According to the relationship between genotype and clinical phenotype, the degree of aldosterone and cortisol deficiency, and the severity of high androgen, 21-OHD is divided into two major types: ①Classic 21-OHD, which is divided into salt loss type according to the degree of aldosterone deficiency (Salt wasting, SW, about 75%) and simple virilizing (SV, about 25%); ②Non-classical 21-OHD (non classical CAH, NCCAH).
CAH can be divided into multiple types according to the types of defective enzymes.
21-OHD is the most common type, accounting for 90%-95%.
Most studies at home and abroad suggest that the incidence of newborn screening is 1/20000~1/10000.
Clinical manifestations The clinical manifestations of 21-OHD include varying degrees of salt loss and hyperandrogenemia.
Neonatal-onset children have manifestations of varying degrees of adrenal cortex dysfunction, such as weakness, nausea, vomiting, feeding difficulties, diarrhea, chronic dehydration, skin pigmentation, and growth retardation.
Adrenal crisis is often the first manifestation of 21-OHD SW in the neonatal period.
It is manifested as severe hyponatremia, hyperkalemia, hypovolemic shock, and may be accompanied by hypoglycemia, induced by stress.
Severe hyponatremia can cause central nervous system manifestations such as convulsions, and severe hyperkalemia can cause fatal arrhythmias.
Hyperandrogenemia manifests differently at different ages.
Female children with typical 21-OHD have different degrees of virilization in their external genitalia at birth.
Mild cases show isolated clitoral hypertrophy.
In severe cases, the external genitalia can be close to men, the labia majora is scrotal-like, the clitoris is hypospadias-like penis, and it has a common urethral vagina.
However, the gonads cannot be touched in the labia majora, and there is a completely normal female internal genital structure (ovaries and uterus).
Males may have no external genital abnormalities such as penis enlargement during neonatal and infancy, which is a common reason for delayed diagnosis.
In early childhood, both sexes will show peripheral precocious puberty.
Boys have enlarged penis with or without premature appearance of pubic hair; female children have heterosexual precocious puberty.
Long-term high levels of sex hormones stimulate hypothalamic gonadotropin releasing hormone (GnRH) neurons to develop central precocious puberty.
Women may also have secondary sexual characteristics dysplasia and primary amenorrhea or oligomenorrhea.
The non-classical 21-OHD is only diagnosed as 21-OHD when it is suspected of being diagnosed as polycystic ovary syndrome in adolescence or adulthood.
Both sexes begin to grow linearly and accelerate the growth of bone age in their infancy, which impairs lifelong height.
Other manifestations include darkening of the skin and mucous membranes, with the areola and vulva as the main manifestations.
Some children may have no such changes.
NCCAH has clinical manifestations of different degrees of hyperandrogenism in childhood, adolescence and even adulthood, and only manifests as growth acceleration and rapid progress in bone age.
Auxiliary examination 1.
Elevated serum 17-OHP 17-OHP is a specific diagnostic index and main treatment monitoring index for 21-OHD.
Generally speaking, the higher the 17-OHP increase, the more severe the degree of enzyme deficiency.
However, 17-OHP and ACTH are both stress hormones.
Therefore, when there is stress, or when the child draws blood and crying severely, it can be significantly higher than the actual level.
This should be considered when interpreting the results.
factor.
2.
Basic serum cortisol and ACTH The serum cortisol of typical patients decreases with ACTH increase.
There are also 21-OHD patients with cortisol in the normal range, while ACTH is elevated, which requires a comprehensive judgment in conjunction with other indicators.
The two hormones of 21-OHD non-classical patients are basically in the normal range.
3.
Androgen The measured value of each androgen should be judged according to the normal reference value established by sex, age and puberty.
Androstenedione has a good correlation with 17-OHP, and the diagnostic and monitoring significance is the best.
DHEAS can also be elevated in polycystic ovary syndrome.
4.
Plasma renin concentration or renin activity, angiotensin II and aldosterone.
Renin is elevated in the 21-OHD SW type, but the diagnostic specificity is not high.
Renin can also be elevated in some patients with non-salt-loss type, and renin is an important monitoring indicator in mineralocorticoid replacement therapy.
Low aldosterone supports the diagnosis of salt loss, but serum aldosterone can be normal in a quarter of children.
5.
Chromosomes Chromosomes are mainly used to exclude 46, XY sexual dysplasia diseases.
6.
Imaging The B-ultrasound and CT imaging examinations of the adrenal glands are helpful for the identification of adrenal tumors or other adrenal (dysplasia) lesions.
Women should complete the uterus, double-attachment B-ultrasound, and check the bone age from the age of 2 years.
7.
Genetic Diagnosis The genetic diagnosis of 21-OHD is very important for the differential diagnosis with clear or unclear biochemical diagnosis, and it is also very important for genetic counseling to be able to diagnose heterozygous carriers.
Diagnosis 21-OHD diagnosis requires comprehensive clinical manifestations, including 17-OHP and the concentration of each relevant hormone to be judged, genetic testing can further confirm the diagnosis.
At present, 21-OHD neonatal screening has been carried out in many areas in China.
For those who are positive for 17-OHP in heel blood screening, they need to follow the screening consensus.
Serum cortisol in NCCAH patients is normal or at the lower limit of normal.
ACTH is normal or critically high.
Diagnosis with 17-OHP basic value is uncertain, and genetic testing is extremely important.
Differential diagnosis The common diseases that need to be differentiated from 21-OHD include: 1.
11β-hydroxylase deficiency (CYP11B1 gene mutation) and hyperandrogenism, very few manifestations of salt loss at birth, and common mineralocorticoids such as water and sodium.
Retention, hypokalemia and hypertension, etc.
, low renin-angiotensin levels, elevated progesterone and 17-OHP.
However, blood pressure in some patients can be normal, and genetic testing and 21-OHD identification are required if necessary.
2.
17α-hydroxylase deficiency (CYP17A1 gene mutation) This enzyme also has 17,20-lyase activity, and its clinical manifestations are symptoms of increased mineralocorticoids, such as hypokalemia, hypertension, and insufficient sex hormones.
, Such as lack of female youth development, male feminization.
Progesterone is elevated, 17-OHP is reduced or normal.
3.
Congenital hereditary adrenal dysplasia is due to the NR0B1 gene or SF1 gene mutations caused congenital adrenal hypofunction, which can be combined with hypogonadism, and its imaging is mostly manifested as adrenal dysplasia.
4.
Adrenocortical tumors Adrenal cortical tumors (especially in children) often start with the clinical manifestations of hyperandrogenemia, with or without hypercortisolism, and even a significant increase in 17-OHP, but a significantly lower ACTH is the main point of differentiation .
Imaging confirmed the space-occupying lesions.
5.
Polycystic ovary syndrome.
For female patients who see a doctor due to menstrual disorders or hyperandrogenism in adolescence or adulthood, the performance of NCCAH can overlap with that of polycystic ovary syndrome, and polycystic ovary syndrome can also cause DHEAS.
Elevated, can be identified by the medium-dose dexamethasone inhibition test, if necessary, CYP21A2 gene testing to confirm the diagnosis.
Treatment 1.
Treatment goals Develop treatment goals according to different types of 21-OHD.
The treatment goals include replacing the physiological requirements of glucocorticoids, while reasonably inhibiting hyperandrogenism, restoring the trajectory of normal growth and development as much as possible, achieving the ideal lifelong height, and improving long-term reproductive health.
2.
Glucocorticoid therapy Hydrocortisone is the basic medication and requires lifelong replacement therapy. It is recommended to formulate a plan according to the patient's still growing and reaching adult height.
For those who have not stopped growing, it is recommended to use hydrocortisone instead.
After reaching adult height, drugs with a relatively long half-life, such as prednisone or dexamethasone, can be given.
Hydrocortisone replacement therapy programs need to establish an individualized program based on the principles of pharmacokinetics.
The dose is set according to age, administered in divided doses, and the dose is adjusted according to monitoring.
The dosage and schedule of alternative treatment should be individually set according to age and developmental period, and should be controlled at the lowest effective dosage as much as possible to avoid excessive growth inhibition and the occurrence of iatrogenic Cushing’s syndrome.
The dosage of glucocorticoids needs to be adjusted during stress and disease.
The general dosage of hydrocortisone for children is 10-15mg/m^2, 3 times a day; for adults, 15-25mg/d, 2~3 times a day.
3.
Mineralocorticoid treatment It is necessary to adjust the dosage in time to avoid the occurrence of iatrogenic hypertension by paying attention to the age change law of salt hormone sensitivity while preventing salt loss crisis.
21-OHD salt-loss type combined with mineralocorticoids on the basis of glucocorticoids can reduce the total amount of glucocorticoids and long-term adverse reactions.
Fludrocortisone is currently the only mineralocorticoid preparation, which can be taken 1 to 2 times a day.
The dosage is set according to the age change rule of sensitivity to mineralocorticoid, and the dosage is adjusted according to monitoring.
As there is no single hormone for judging the curative effect and the "gold standard" for a fixed cut point, it is recommended to combine hormones and clinical indicators to monitor comprehensive judgments to achieve the most ideal goal of individualized treatment.
The general dosage of fludrocortisone for children is 0.
05-0.
2mg/d, 1 to 2 times a day; for adults, the dosage is 0.
05-0.
2mg/d, orally once a day.
4.
Growth hormone and gonadotropin-releasing hormone analogues For those with severe precocious puberty, significantly advanced bone age, and predicted adult height loss, growth hormone therapy may be considered. For patients who have developed central precocious puberty, gonadotropin-releasing hormone analogs can be combined.
However, the improvement of life-long height of these drugs is related to the control of the patient's primary disease, the treatment response to the drug, the degree of advancement of the bone age, and the genetic height of the parents.
Therefore, the treatment effect varies greatly among individuals.
Complication monitoring needs to ask patients about their symptoms regularly during treatment, including symptoms of insufficient replacement of glucocorticoids and mineralocorticoids, such as anorexia, fatigue, dizziness, etc.
, whether there is any recent stress and adrenal crisis.
Ask if there are symptoms of excessive replacement, such as bulimia, weight gain, weakness, etc.
Monitor blood pressure, electrolytes, blood sugar, ACTH, 17-OHP, testosterone, androstenedione, renin concentration or renin activity, angiotensin II, LH, FSH, etc.
to evaluate the control of primary disease, adjust glucocorticoids and salts The dose of corticosteroids.
In addition, it is also necessary to pay attention to the adverse effects of long-term treatment with glucocorticoids such as glucose and lipid metabolism and bone density.
For male patients, the testicular residual adrenal tumors (TARTs) should be regularly monitored for patients over 8 years of age.
TARTs have a greater impact on the spermatogenesis of 21-OHD male patients.
Figure 1 21-hydroxylase deficiency diagnosis and treatment process The above content is extracted from: The National Health Commission of the People's Republic of China.
Guidelines for the diagnosis and treatment of rare diseases (2019 edition) [J].
The official website of the National Health Commission of the People's Republic of China.