-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
What principles should be followed in the drug treatment of hyperthyroidism? How to choose ATD drugs during pregnancy? Can methimazole be prescribed during lactation? In order to standardize the rational use of drugs for hyperthyroidism by primary-level doctors, the Chinese Medical Association, the Chinese Medical Association Branch of Clinical Pharmacy, and the Journal of the Chinese Medical Association jointly formulated the "Guidelines for the Rational Use of Primary-level Drugs for Hyperthyroidism" (the full version of the guide is attached at the end of the article) Download link)
.
The principle of drug treatment of hyperthyroidism The purpose of hyperthyroidism treatment is to control the symptoms of hyperthyroidism, reduce the serum thyroid hormone level to normal, and promote the normalization of immune monitoring
.
Antithyroid drugs (ATD) are mainly thiourea drugs, and β-blockers assist symptomatic treatment, which can quickly control symptoms
.
1.
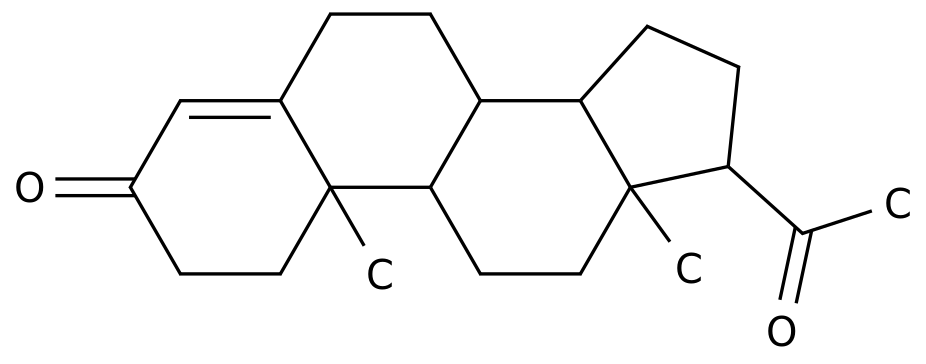
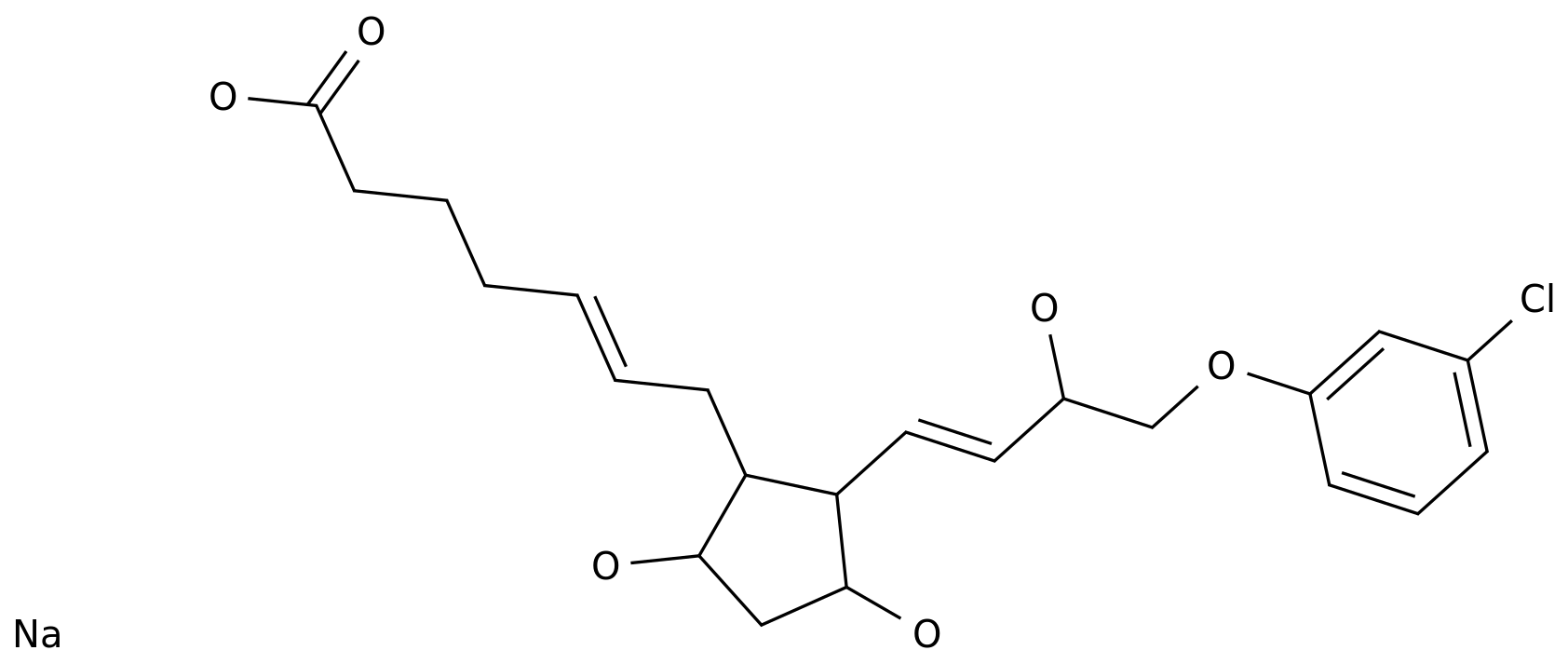
ATD-the preferred methimazole ATD is mainly imidazoles [representing the drug methimazole (MMI)] and thiouracil [representing the drug propylthiouracil (PTU)].
ATD is suitable for various types of hyperthyroidism.
Especially suitable for: ➤ patients with mild disease and mild to moderate thyroid enlargement; ➤ teenagers, children, and elderly patients; ➤ patients who relapse after thyroid surgery and are not suitable for 131I treatment; ➤pre-surgery preparation; ➤as 131I treatment Of adjuvant therapy
.
In most cases, MMIPTU is the first choice to reduce the conversion of T4 to T3 in peripheral tissues by inhibiting the activity of 5'deiodinase, but the liver toxicity is greater than MMI.
Therefore, except for severe cases, thyroid crisis, early pregnancy or those who are allergic to MMI, PTU is the preferred treatment, others Situation MMI should be listed as the drug of choice
.
Can methimazole be used during lactation? Regarding the use of ATD during lactation, this guideline did not describe in detail, so we collected relevant domestic guidelines or expert descriptions for your reference: 1.
"Guidelines for Diagnosis and Treatment of Thyroid Diseases in Pregnancy and Postpartum (2nd Edition)" (released in August 2019) In "Chinese Journal of Endocrinology and Metabolism"): Studies have shown that taking low to moderate doses of PTU and MMI is safe for breastfed infants
.
However, considering the relatively small size of the study population, the recommended maximum dose is MMI 20 mg/d or PTU 300 mg/d
.
If breastfeeding hyperthyroidism patients need to use ATD, the pros and cons of medication should be weighed
.
ATD should be taken after each breastfeeding
.
2.
Professor Liu Chao's speech (May 2021, China Medical University Thyroid Forum): ATD only enters breast milk in a small amount, so the use of low-dose PTU (<250mg/d) or MMI (<20mg/d) is considered Safe
.
It is generally recommended to take the medicine after breastfeeding, and take the medicine for more than 4 hours before the next breastfeeding to monitor the child's thyroid function
.
2.
Beta blockers Beta blockers can inhibit the increase of catecholamines by blocking the activity of sympathetic adrenergic receptors in target organs, and can improve irritability, heat resistance, hyperhidrosis, and tachycardia , Muscle tremor and other symptoms
.
In addition, it can inhibit the conversion of T4 to T3 in peripheral tissues, and block the direct effect of thyroid hormone on the myocardium
.
It is suitable for elderly patients or patients with a resting heart rate> 90 beats/min or patients with cardiovascular disease
.
Common treatment drugs for hyperthyroidism are shown in Table 1
.
Table 1 Drug treatment of hyperthyroidism Hyperthyroidism treatment drug-methimazole (MMI) 1.
Who is suitable for? ➤MMI is especially suitable for young patients and patients with or without mild thyroid enlargement (goiter); ➤for pre-surgical preparations for various types of hyperthyroidism; ➤for preparations for hyperthyroidism patients before radioactive iodine treatment, To prevent the occurrence of thyroid toxicity crisis after treatment; ➤For the intermittent treatment of hyperthyroidism after radioiodine therapy; ➤For relapse after thyroid surgery, but not suitable for radioactive 131I treatment; ➤For the treatment of Graves disease caused by pregnant women Thyrotoxicosis; ➤For the treatment of drug-induced thyrotoxicosis
.
2.
Methimazole Usage and Dosage This product should be taken orally, with a meal after a meal
.
Adults: ➤Hyperthyroidism: Oral administration, the initial dose is 20-40 mg/d, divided into 1 to 2 times
.
If the condition improves within 2-6 weeks, the dose can be gradually reduced to the maintenance dose
.
The dose for the next 1-2 years is 2.
5-10 mg/d
.
If the condition requires it can be taken with thyroid hormone
.
➤Preoperative preparation for hyperthyroidism: ATD treatment is strongly recommended before hyperthyroidism.
Thyroid function should be controlled in a normal state
.
Iodine was added 10 days before the operation to fix the thyroid tissue, and the drug was stopped 1 day before the operation
.
➤Intermittent treatment before and after radioiodine treatment: Oral administration, depending on the patient's condition
.
➤Long-term anti-thyroid therapy (the condition cannot be relieved and conventional treatment measures cannot be used): Oral administration, giving the lowest possible dose, usually 2.
5-10 mg/d, with or without a small amount of thyroid hormone
.
Children: ➤The initial dose is determined according to the severity of the disease, 0.
3-0.
5 mg·kg-1·d-1; ➤The maintenance dose is 0.
2-0.
3 mg·kg-1·d-1, plus thyroid hormone therapy as needed
.
3.
Which patients are prohibited from using it? MMI is contraindicated in people who are allergic to this drug or other thiourea derivatives or its excipients, moderate to severe neutropenia, patients with cholestasis caused by non-hyperthyroidism, and agranulocytosis or agranulocytosis after receiving this drug or PTU treatment.
Severe bone marrow suppression or acute pancreatitis, and breastfeeding women
.
4.
Adverse reactions and treatment Adverse reactions: Allergic skin reactions may occur after medication, manifested as itching, rash, etc.
, most of which can be relieved by themselves
.
Treatment: If the rash is mild and scattered, consider combined antihistamine treatment.
If the treatment effect is poor or worsened, the drug should be discontinued and changed to 131I or surgical treatment
.
Other adverse reactions and treatment: joint pain (may appear after several months of treatment), decreased taste, nausea, vomiting, upper abdominal discomfort, dizziness, headache, etc.
may occur
.
It can cause systemic adverse reactions such as abnormal liver function and leukopenia.
If an intolerable adverse reaction occurs, the drug should be stopped and seek medical attention
.
If the baseline transaminase is greater than 3 to 5 times the upper limit of normal (ULN), avoid ATD treatment.
It is recommended to transfer to a higher-level hospital to further check the cause of abnormal liver function, receive corresponding treatment, and decide the next treatment plan based on the condition
.
5.
Drug interactions ➤Patients with hyperthyroidism who have received stable doses of digitalis, theophylline, and β-adrenergic receptor blockers, may increase serum digitalis levels when using MMI and returning to a normal state of thyroid function.
Need to reduce the dose of digoxigenin; ➤Insufficient iodine can increase the thyroid's responsiveness to the drug, and excessive iodine can reduce the thyroid's responsiveness to the drug; ➤Cross allergic reaction with thiourea ATD
.
Hyperthyroidism treatment drug-propylthiouracil (PTU) 1.
Who is suitable for? PTU is suitable for various types of hyperthyroidism, especially suitable for the following conditions: ➤Slight illness, mild to moderate thyroid enlargement; ➤Age<20 years old, hyperthyroidism in pregnancy, old and weak; ➤combined with severe heart, liver, Patients with kidney disease who cannot tolerate surgery, those who are not suitable for surgery or radioactive iodine treatment, and those who relapse after surgery are not suitable for radioactive iodine treatment; ➤ As an adjuvant treatment during radioactive iodine treatment
.
2.
Usage and Dosage of Propylthiouracil The daily dose of PTU should be taken orally in divided doses with the interval as even as possible
.
The dosage is adjusted at any time according to the condition
.
Adults: ➤Hyperthyroidism: The initial dose is generally 300mg/d, depending on the severity of the disease, 150-400mg/d, the maximum dose is 600mg/d, orally in 3 doses
.
After the condition is controlled, the dose is gradually reduced, and the drug is reduced once every 2 to 4 weeks, and the maintenance dose is 50 to 100 mg/d
.
Levothyroxine or thyroid tablets may be added as appropriate when hypothyroidism or thyroid enlargement occurs during treatment
.
➤Thyroid crisis: 400-800mg/d, divided into 3 to 4 times, the course of treatment generally does not exceed 1 week
.
➤Preoperative preparation for hyperthyroidism: 100mg/time, 3~4 times/d, to restore thyroid function to normal or close to normal, and then take iodine for 2 weeks before surgery
.
Children: The starting dose is 4 mg·kg-1·d-1 according to body weight, divided orally, and the maintenance dose should be reduced
.
3.
Which patients are prohibited from using it? It is contraindicated in those with severe liver damage, those with severe white blood cell deficiency, and those who are allergic to thiourea drugs
.
4.
Adverse reactions and treatment PTU-related adverse reactions mostly occurred in the first 2 months of initial medication
.
Headache, dizziness, joint pain, swollen salivary glands and lymph nodes, and gastrointestinal reactions are common
.
There will also be allergic reactions such as skin rashes and drug fever.
Be wary of individual patients who can develop exfoliative dermatitis, jaundice and toxic hepatitis
.
The number of white blood cells in the peripheral blood decreases.
If agranulocytosis occurs and the neutrophil count is less than 1.
5×10^9/L, the drug should be stopped immediately, and the risk of adverse blood reactions in elderly patients increases
.
5.
Drug interactions ➤Combined use with oral anticoagulants can increase the anticoagulant effect; ➤sulfonamides, p-aminosalicylic acid, phenylbutazone, barbiturates, phentolamine, tolazoline, vitamin B12 , Sulfonylureas, etc.
, have the effect of inhibiting thyroid function and causing goiter, so pay attention when using them together; ➤The intake of high-iodine foods or drugs can aggravate the hyperthyroidism, so avoid taking iodine before taking this product.
Agent
.
Adjuvant treatment of hyperthyroidism-propranolol 1.
Who is suitable for? Propranolol is a non-selective beta blocker
.
It can improve the symptoms of tachycardia, palpitations, irritability and hyperhidrosis, and reduce the transition from T4 to T3 in peripheral tissues
.
Mainly used for: ➤ Thyroid crisis or aura of crisis; ➤ Preoperative preparation for subtotal thyroidectomy; ➤ For patients with severe hyperthyroidism, it is used to control symptoms before antithyroid drugs or radioactive iodine treatment has not yet taken effect
.
2.
Propranolol usage and dosage ➤Hyperthyroidism: 10-20mg/time, 3 times/d
.
➤Thyroid crisis: 60~80mg/time, 1 time/4h
.
➤Pre-operative preparation for hyperthyroidism: Orally, 20-40mg/time, 1 time/6 h, increase the amount if necessary, until the symptoms of hyperthyroidism are controlled and the heart rate drops to the normal range
.
You need to take the medicine once in the morning on the day of the operation, and continue to take it for a few days after the operation; the dosage will be gradually reduced according to the condition.
If the condition is stable, the medicine can be stopped after 1 week.
.
Note that orthostatic hypotension may occur when the dose is large
.
3.
Which patients are prohibited from using it? It is contraindicated in bronchial asthma, cardiogenic shock, sinus bradycardia, second and third degree atrioventricular block, acute heart failure, unless the heart failure is caused by propranolol treatable arrhythmia
.
4.
Adverse reactions and treatment Most of the adverse reactions are mild and short in duration, and do not need to be stopped
.
Central nervous system adverse reactions such as dizziness, confusion (especially in the elderly), depression, and unresponsiveness may occur; dizziness (due to hypotension); bradycardia (<50 beats/min); less common Bronchial spasm and dyspnea, congestive heart failure; less common are fever and sore throat (agranulocytosis), skin rash (allergic reaction), bleeding tendency (thrombocytopenia)
.
When adverse reactions persist, be extra vigilant against Raynaud’s sign like cold limbs, diarrhea, fatigue, dry eyes or skin, nausea, numbness of the fingers and toes, and abnormal fatigue
.
5.
Drug interactions ➤Combined use with reserpine, monoamine oxidase inhibitors, and haloperidol can cause hypotension; ➤Combined use with epinephrine, phenylephrine or sympathomimetic amines can cause significant hypertension and bradycardia Atrioventricular block may also occur; ➤When combined with digitalis and calcium antagonists, be very vigilant against the inhibition of the myocardium and conduction system; ➤Combined with isoproterenol or xanthine, the latter can weaken the efficacy of the latter; ➤Aluminum hydroxide and alcohol can reduce the absorption of propranolol; ➤Phenytoin, phenobarbital and rifampicin can accelerate the clearance of propranolol, antipyrine, theophylline, cimetidine, chlorine Promazine and lidocaine can reduce the clearance rate of propranolol; ➤ combined with thyroxine can cause a decrease in T3 concentration; ➤ can affect blood sugar levels, so when using together with hypoglycemic drugs, the dose of the latter needs to be adjusted
.
Adjuvant treatment of hyperthyroidism-Metoprolol 1.
Who is suitable for? Metoprolol is a selective β1 receptor blocker
.
Patients with bronchial asthma or wheezing bronchitis can choose metoprolol when propranolol is contraindicated, and the indications are the same as propranolol
.
2.
The usage and dosage of metoprolol are taken orally, 25-50 mg/time, 2-3 times/d, or 100 mg/time, 2 times/d
.
3.
Which patients are prohibited from using it? Contraindicated in cardiogenic shock, sick sinus syndrome, second and third degree atrioventricular block, unstable and decompensated heart failure (pulmonary edema, hypoperfusion or hypotension), symptomatic hypercardiac Metoprolol should not be used for patients with suspected acute myocardial infarction, that is, patients with heart rate <45 beats/min, PQ interval> 0.
24 s, or systolic blood pressure <100 mmHg (1 mmHg=0.
133 kPa).
Patients with severe peripheral vascular disease who are at risk of gangrene, and those who are allergic to any of the ingredients in this product or other β-blockers
.
4.
Adverse reactions and treatment Adverse reactions are often related to dosage
.
Common adverse reactions include fatigue, headache, dizziness, chills, bradycardia, palpitations, abdominal pain, nausea, vomiting, diarrhea, and constipation
.
Rare adverse reactions include chest pain, weight gain, temporary worsening of heart failure, sleep disturbance, paresthesia, shortness of breath, bronchial asthma, or bronchospasm in those with asthma symptoms
.
If serious adverse reactions or untolerable adverse reactions occur, the drug should be discontinued and seek medical attention
.
5.
Drug interactions ➤ Drugs that inhibit CYP2D6 (such as quinidine, terbinafine, paroxetine, fluoxetine, sertraline, celecoxib, propafenone, and diphenhydramine) can affect metoprolol For the plasma concentration of Lolol, the dose of metoprolol should be reduced when starting the above-mentioned drug treatment; ➤If combined with cimetidine or hydralazine, the plasma concentration of metoprolol will increase; ➤Metoprolol should be Avoid combined use with barbiturates, propafenone, and verapamil; ➤with amiodarone, class I antiarrhythmic drugs, non-steroidal anti-inflammatory/anti-rheumatic drugs (NSAID), diphenhydramine Dose adjustment may be required when drugs such as diltiazem, epinephrine, quinidine, and clonidine are used in combination; ➤ Note that patients receiving β-blocker therapy should readjust the dose of oral hypoglycemic drugs
.
Download link of the full version of the guide: http://guide.
medlive.
cn/guideline/23504 The above content is extracted from: Chinese Medical Association, Chinese Medical Association Clinical Pharmacy Branch, Chinese Medical Association Journal, etc.
Guidelines for rational use of drugs for hyperthyroidism [J].
Chinese Journal of General Practitioners, 2021,20(5):515-519.
DOI: 10.
3760/cma.
j.
cn114798-20210317-00249.
.
The principle of drug treatment of hyperthyroidism The purpose of hyperthyroidism treatment is to control the symptoms of hyperthyroidism, reduce the serum thyroid hormone level to normal, and promote the normalization of immune monitoring
.
Antithyroid drugs (ATD) are mainly thiourea drugs, and β-blockers assist symptomatic treatment, which can quickly control symptoms
.
1.
ATD-the preferred methimazole ATD is mainly imidazoles [representing the drug methimazole (MMI)] and thiouracil [representing the drug propylthiouracil (PTU)].
ATD is suitable for various types of hyperthyroidism.
Especially suitable for: ➤ patients with mild disease and mild to moderate thyroid enlargement; ➤ teenagers, children, and elderly patients; ➤ patients who relapse after thyroid surgery and are not suitable for 131I treatment; ➤pre-surgery preparation; ➤as 131I treatment Of adjuvant therapy
.
In most cases, MMIPTU is the first choice to reduce the conversion of T4 to T3 in peripheral tissues by inhibiting the activity of 5'deiodinase, but the liver toxicity is greater than MMI.
Therefore, except for severe cases, thyroid crisis, early pregnancy or those who are allergic to MMI, PTU is the preferred treatment, others Situation MMI should be listed as the drug of choice
.
Can methimazole be used during lactation? Regarding the use of ATD during lactation, this guideline did not describe in detail, so we collected relevant domestic guidelines or expert descriptions for your reference: 1.
"Guidelines for Diagnosis and Treatment of Thyroid Diseases in Pregnancy and Postpartum (2nd Edition)" (released in August 2019) In "Chinese Journal of Endocrinology and Metabolism"): Studies have shown that taking low to moderate doses of PTU and MMI is safe for breastfed infants
.
However, considering the relatively small size of the study population, the recommended maximum dose is MMI 20 mg/d or PTU 300 mg/d
.
If breastfeeding hyperthyroidism patients need to use ATD, the pros and cons of medication should be weighed
.
ATD should be taken after each breastfeeding
.
2.
Professor Liu Chao's speech (May 2021, China Medical University Thyroid Forum): ATD only enters breast milk in a small amount, so the use of low-dose PTU (<250mg/d) or MMI (<20mg/d) is considered Safe
.
It is generally recommended to take the medicine after breastfeeding, and take the medicine for more than 4 hours before the next breastfeeding to monitor the child's thyroid function
.
2.
Beta blockers Beta blockers can inhibit the increase of catecholamines by blocking the activity of sympathetic adrenergic receptors in target organs, and can improve irritability, heat resistance, hyperhidrosis, and tachycardia , Muscle tremor and other symptoms
.
In addition, it can inhibit the conversion of T4 to T3 in peripheral tissues, and block the direct effect of thyroid hormone on the myocardium
.
It is suitable for elderly patients or patients with a resting heart rate> 90 beats/min or patients with cardiovascular disease
.
Common treatment drugs for hyperthyroidism are shown in Table 1
.
Table 1 Drug treatment of hyperthyroidism Hyperthyroidism treatment drug-methimazole (MMI) 1.
Who is suitable for? ➤MMI is especially suitable for young patients and patients with or without mild thyroid enlargement (goiter); ➤for pre-surgical preparations for various types of hyperthyroidism; ➤for preparations for hyperthyroidism patients before radioactive iodine treatment, To prevent the occurrence of thyroid toxicity crisis after treatment; ➤For the intermittent treatment of hyperthyroidism after radioiodine therapy; ➤For relapse after thyroid surgery, but not suitable for radioactive 131I treatment; ➤For the treatment of Graves disease caused by pregnant women Thyrotoxicosis; ➤For the treatment of drug-induced thyrotoxicosis
.
2.
Methimazole Usage and Dosage This product should be taken orally, with a meal after a meal
.
Adults: ➤Hyperthyroidism: Oral administration, the initial dose is 20-40 mg/d, divided into 1 to 2 times
.
If the condition improves within 2-6 weeks, the dose can be gradually reduced to the maintenance dose
.
The dose for the next 1-2 years is 2.
5-10 mg/d
.
If the condition requires it can be taken with thyroid hormone
.
➤Preoperative preparation for hyperthyroidism: ATD treatment is strongly recommended before hyperthyroidism.
Thyroid function should be controlled in a normal state
.
Iodine was added 10 days before the operation to fix the thyroid tissue, and the drug was stopped 1 day before the operation
.
➤Intermittent treatment before and after radioiodine treatment: Oral administration, depending on the patient's condition
.
➤Long-term anti-thyroid therapy (the condition cannot be relieved and conventional treatment measures cannot be used): Oral administration, giving the lowest possible dose, usually 2.
5-10 mg/d, with or without a small amount of thyroid hormone
.
Children: ➤The initial dose is determined according to the severity of the disease, 0.
3-0.
5 mg·kg-1·d-1; ➤The maintenance dose is 0.
2-0.
3 mg·kg-1·d-1, plus thyroid hormone therapy as needed
.
3.
Which patients are prohibited from using it? MMI is contraindicated in people who are allergic to this drug or other thiourea derivatives or its excipients, moderate to severe neutropenia, patients with cholestasis caused by non-hyperthyroidism, and agranulocytosis or agranulocytosis after receiving this drug or PTU treatment.
Severe bone marrow suppression or acute pancreatitis, and breastfeeding women
.
4.
Adverse reactions and treatment Adverse reactions: Allergic skin reactions may occur after medication, manifested as itching, rash, etc.
, most of which can be relieved by themselves
.
Treatment: If the rash is mild and scattered, consider combined antihistamine treatment.
If the treatment effect is poor or worsened, the drug should be discontinued and changed to 131I or surgical treatment
.
Other adverse reactions and treatment: joint pain (may appear after several months of treatment), decreased taste, nausea, vomiting, upper abdominal discomfort, dizziness, headache, etc.
may occur
.
It can cause systemic adverse reactions such as abnormal liver function and leukopenia.
If an intolerable adverse reaction occurs, the drug should be stopped and seek medical attention
.
If the baseline transaminase is greater than 3 to 5 times the upper limit of normal (ULN), avoid ATD treatment.
It is recommended to transfer to a higher-level hospital to further check the cause of abnormal liver function, receive corresponding treatment, and decide the next treatment plan based on the condition
.
5.
Drug interactions ➤Patients with hyperthyroidism who have received stable doses of digitalis, theophylline, and β-adrenergic receptor blockers, may increase serum digitalis levels when using MMI and returning to a normal state of thyroid function.
Need to reduce the dose of digoxigenin; ➤Insufficient iodine can increase the thyroid's responsiveness to the drug, and excessive iodine can reduce the thyroid's responsiveness to the drug; ➤Cross allergic reaction with thiourea ATD
.
Hyperthyroidism treatment drug-propylthiouracil (PTU) 1.
Who is suitable for? PTU is suitable for various types of hyperthyroidism, especially suitable for the following conditions: ➤Slight illness, mild to moderate thyroid enlargement; ➤Age<20 years old, hyperthyroidism in pregnancy, old and weak; ➤combined with severe heart, liver, Patients with kidney disease who cannot tolerate surgery, those who are not suitable for surgery or radioactive iodine treatment, and those who relapse after surgery are not suitable for radioactive iodine treatment; ➤ As an adjuvant treatment during radioactive iodine treatment
.
2.
Usage and Dosage of Propylthiouracil The daily dose of PTU should be taken orally in divided doses with the interval as even as possible
.
The dosage is adjusted at any time according to the condition
.
Adults: ➤Hyperthyroidism: The initial dose is generally 300mg/d, depending on the severity of the disease, 150-400mg/d, the maximum dose is 600mg/d, orally in 3 doses
.
After the condition is controlled, the dose is gradually reduced, and the drug is reduced once every 2 to 4 weeks, and the maintenance dose is 50 to 100 mg/d
.
Levothyroxine or thyroid tablets may be added as appropriate when hypothyroidism or thyroid enlargement occurs during treatment
.
➤Thyroid crisis: 400-800mg/d, divided into 3 to 4 times, the course of treatment generally does not exceed 1 week
.
➤Preoperative preparation for hyperthyroidism: 100mg/time, 3~4 times/d, to restore thyroid function to normal or close to normal, and then take iodine for 2 weeks before surgery
.
Children: The starting dose is 4 mg·kg-1·d-1 according to body weight, divided orally, and the maintenance dose should be reduced
.
3.
Which patients are prohibited from using it? It is contraindicated in those with severe liver damage, those with severe white blood cell deficiency, and those who are allergic to thiourea drugs
.
4.
Adverse reactions and treatment PTU-related adverse reactions mostly occurred in the first 2 months of initial medication
.
Headache, dizziness, joint pain, swollen salivary glands and lymph nodes, and gastrointestinal reactions are common
.
There will also be allergic reactions such as skin rashes and drug fever.
Be wary of individual patients who can develop exfoliative dermatitis, jaundice and toxic hepatitis
.
The number of white blood cells in the peripheral blood decreases.
If agranulocytosis occurs and the neutrophil count is less than 1.
5×10^9/L, the drug should be stopped immediately, and the risk of adverse blood reactions in elderly patients increases
.
5.
Drug interactions ➤Combined use with oral anticoagulants can increase the anticoagulant effect; ➤sulfonamides, p-aminosalicylic acid, phenylbutazone, barbiturates, phentolamine, tolazoline, vitamin B12 , Sulfonylureas, etc.
, have the effect of inhibiting thyroid function and causing goiter, so pay attention when using them together; ➤The intake of high-iodine foods or drugs can aggravate the hyperthyroidism, so avoid taking iodine before taking this product.
Agent
.
Adjuvant treatment of hyperthyroidism-propranolol 1.
Who is suitable for? Propranolol is a non-selective beta blocker
.
It can improve the symptoms of tachycardia, palpitations, irritability and hyperhidrosis, and reduce the transition from T4 to T3 in peripheral tissues
.
Mainly used for: ➤ Thyroid crisis or aura of crisis; ➤ Preoperative preparation for subtotal thyroidectomy; ➤ For patients with severe hyperthyroidism, it is used to control symptoms before antithyroid drugs or radioactive iodine treatment has not yet taken effect
.
2.
Propranolol usage and dosage ➤Hyperthyroidism: 10-20mg/time, 3 times/d
.
➤Thyroid crisis: 60~80mg/time, 1 time/4h
.
➤Pre-operative preparation for hyperthyroidism: Orally, 20-40mg/time, 1 time/6 h, increase the amount if necessary, until the symptoms of hyperthyroidism are controlled and the heart rate drops to the normal range
.
You need to take the medicine once in the morning on the day of the operation, and continue to take it for a few days after the operation; the dosage will be gradually reduced according to the condition.
If the condition is stable, the medicine can be stopped after 1 week.
.
Note that orthostatic hypotension may occur when the dose is large
.
3.
Which patients are prohibited from using it? It is contraindicated in bronchial asthma, cardiogenic shock, sinus bradycardia, second and third degree atrioventricular block, acute heart failure, unless the heart failure is caused by propranolol treatable arrhythmia
.
4.
Adverse reactions and treatment Most of the adverse reactions are mild and short in duration, and do not need to be stopped
.
Central nervous system adverse reactions such as dizziness, confusion (especially in the elderly), depression, and unresponsiveness may occur; dizziness (due to hypotension); bradycardia (<50 beats/min); less common Bronchial spasm and dyspnea, congestive heart failure; less common are fever and sore throat (agranulocytosis), skin rash (allergic reaction), bleeding tendency (thrombocytopenia)
.
When adverse reactions persist, be extra vigilant against Raynaud’s sign like cold limbs, diarrhea, fatigue, dry eyes or skin, nausea, numbness of the fingers and toes, and abnormal fatigue
.
5.
Drug interactions ➤Combined use with reserpine, monoamine oxidase inhibitors, and haloperidol can cause hypotension; ➤Combined use with epinephrine, phenylephrine or sympathomimetic amines can cause significant hypertension and bradycardia Atrioventricular block may also occur; ➤When combined with digitalis and calcium antagonists, be very vigilant against the inhibition of the myocardium and conduction system; ➤Combined with isoproterenol or xanthine, the latter can weaken the efficacy of the latter; ➤Aluminum hydroxide and alcohol can reduce the absorption of propranolol; ➤Phenytoin, phenobarbital and rifampicin can accelerate the clearance of propranolol, antipyrine, theophylline, cimetidine, chlorine Promazine and lidocaine can reduce the clearance rate of propranolol; ➤ combined with thyroxine can cause a decrease in T3 concentration; ➤ can affect blood sugar levels, so when using together with hypoglycemic drugs, the dose of the latter needs to be adjusted
.
Adjuvant treatment of hyperthyroidism-Metoprolol 1.
Who is suitable for? Metoprolol is a selective β1 receptor blocker
.
Patients with bronchial asthma or wheezing bronchitis can choose metoprolol when propranolol is contraindicated, and the indications are the same as propranolol
.
2.
The usage and dosage of metoprolol are taken orally, 25-50 mg/time, 2-3 times/d, or 100 mg/time, 2 times/d
.
3.
Which patients are prohibited from using it? Contraindicated in cardiogenic shock, sick sinus syndrome, second and third degree atrioventricular block, unstable and decompensated heart failure (pulmonary edema, hypoperfusion or hypotension), symptomatic hypercardiac Metoprolol should not be used for patients with suspected acute myocardial infarction, that is, patients with heart rate <45 beats/min, PQ interval> 0.
24 s, or systolic blood pressure <100 mmHg (1 mmHg=0.
133 kPa).
Patients with severe peripheral vascular disease who are at risk of gangrene, and those who are allergic to any of the ingredients in this product or other β-blockers
.
4.
Adverse reactions and treatment Adverse reactions are often related to dosage
.
Common adverse reactions include fatigue, headache, dizziness, chills, bradycardia, palpitations, abdominal pain, nausea, vomiting, diarrhea, and constipation
.
Rare adverse reactions include chest pain, weight gain, temporary worsening of heart failure, sleep disturbance, paresthesia, shortness of breath, bronchial asthma, or bronchospasm in those with asthma symptoms
.
If serious adverse reactions or untolerable adverse reactions occur, the drug should be discontinued and seek medical attention
.
5.
Drug interactions ➤ Drugs that inhibit CYP2D6 (such as quinidine, terbinafine, paroxetine, fluoxetine, sertraline, celecoxib, propafenone, and diphenhydramine) can affect metoprolol For the plasma concentration of Lolol, the dose of metoprolol should be reduced when starting the above-mentioned drug treatment; ➤If combined with cimetidine or hydralazine, the plasma concentration of metoprolol will increase; ➤Metoprolol should be Avoid combined use with barbiturates, propafenone, and verapamil; ➤with amiodarone, class I antiarrhythmic drugs, non-steroidal anti-inflammatory/anti-rheumatic drugs (NSAID), diphenhydramine Dose adjustment may be required when drugs such as diltiazem, epinephrine, quinidine, and clonidine are used in combination; ➤ Note that patients receiving β-blocker therapy should readjust the dose of oral hypoglycemic drugs
.
Download link of the full version of the guide: http://guide.
medlive.
cn/guideline/23504 The above content is extracted from: Chinese Medical Association, Chinese Medical Association Clinical Pharmacy Branch, Chinese Medical Association Journal, etc.
Guidelines for rational use of drugs for hyperthyroidism [J].
Chinese Journal of General Practitioners, 2021,20(5):515-519.
DOI: 10.
3760/cma.
j.
cn114798-20210317-00249.