Does methotrexate not increase the risk of RA lung disease? These "lung care" methods are known to know about the seULAR 2020.
-
Last Update: 2020-07-21
-
Source: Internet
-
Author: User
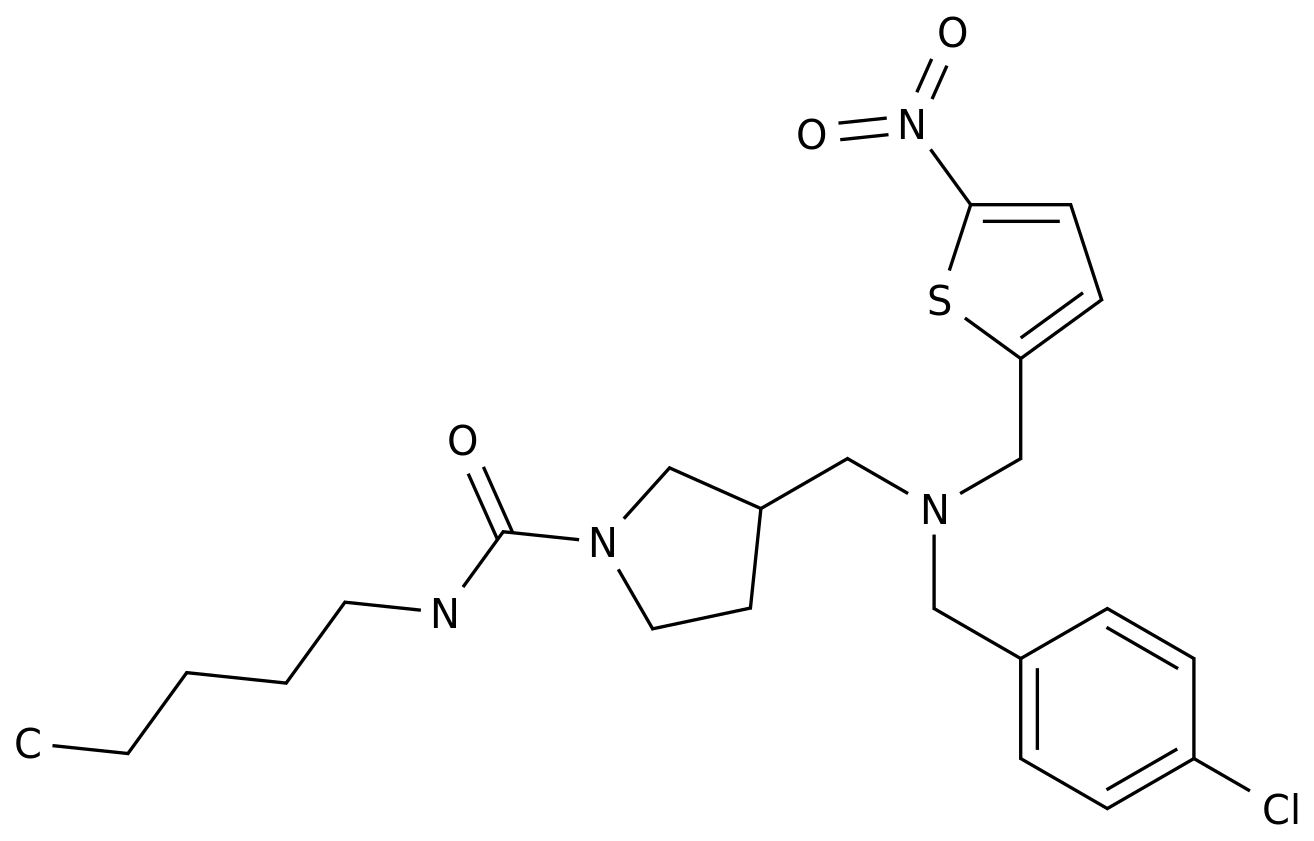
Search more information of high quality chemicals, good prices and reliable suppliers, visit
www.echemi.com
Don't want to miss Jiemei's push? Poke the blue word "medical rheumatism and nephropathy channel" to pay attention to us and click the "··" menu in the upper right corner and select "set as star" to learn about rheumatoid arthritis and lung health! About 10% - 50% of RA patients complicated with ILD rheumatoid arthritis (RA) is a progressive systemic immune disease, symmetrical polyarthritis is the main clinical manifestation, in addition, it can involve a variety of organs and tissues, such as heart, lung, blood vessels, kidney, skin and so on [1,2].interstitial lung disease (ILD) is one of the common clinical manifestations of RA patients except joint lesions. According to the statistical analysis of relevant data, 10% - 50% of RA patients involve the lung [3].an oral report at the 2020 EULAR annual meeting (Abstract: 0p0035) [4] included 8963 RA patients diagnosed from the discussion analytics jointman database to assess the epidemiological and clinical characteristics of rheumatoid arthritis with interstitial lung disease (ra-ild).the results showed that 337 patients (3.8%) had ILD after RA diagnosis or when RA was diagnosed for the first time. The median time of ILD attack after RA diagnosis was 2.3 years, and 47% of patients had ILD within 2 years after RA diagnosis.Table 1: the prevalence of ILD in RA patients was significantly higher than that in patients with RA alone (65.8 years vs 59.1 years, P & lt; 0.001).in addition, the clinical manifestations of patients at baseline were compared. It was found that compared with patients with RA only, ra-ild patients had a higher proportion of chronic obstructive pulmonary disease history, rheumatoid factor positive, rheumatoid nodules, erosive joint disease, anti cyclic citrullinated peptide antibody positive and joint swelling in the baseline period.Table 2: clinical characteristics of patients at baseline. 2. Methotrexate does not increase the risk of ILD in RA patients. The pathogenesis of ra-ild has not been fully clarified, but some risk factors are considered to play an important role, such as male, elderly, smoking, disease severity, high titer of rheumatoid factor, presence of subcutaneous rheumatoid nodules, etc. [5,6].methotrexate (MTX) is the first-line drug for the treatment of RA. The use of MTX is related to hypersensitive pneumonia and diffuse lung disease.however, it is still controversial whether MTX can increase the risk of ILD in RA patients.in the oral report of the 2020 EULAR annual meeting (Abstract: 0p0036) [7], the correlation between MTX exposure and ILD in 482 ra-ild patients and 741 RA patients without ILD was evaluated by case-control study design.the results showed that there was an inverse relationship between MTX exposure and ra-ild, and the adjusted or was 0.43 (95% Cl 0.28-0.65; P & lt; 0.0001) using a combination of derived and validated samples.compared with RA patients without ILD, the frequency of MTX use in ra-ild patients is lower.in patients with ra-ild, the onset of ILD was significantly delayed in patients who had received MTX treatment than those who had not received MTX treatment (11.5 ± 10.6 years vs 3.7 ± 7.1 years, P & lt; 0.001), and MTX was not a risk factor for ra-ild.3ra-ild has a poor prognosis. It is very important to assess the risk stratification of ra-ild. The onset of ra-ild is insidious. The early onset characteristics of ra-ild are not obvious. In the late stage, irreversible pulmonary fibrosis may occur, eventually leading to respiratory failure and poor prognosis.an oral report of the 2020 EULAR annual meeting (Abstract: 0p0039) [8] included 21525 RA patients (2965 RA patients with pulmonary disease) to assess the risk of all-cause, respiratory related hospitalization and mortality in patients with and without pulmonary disease.the results showed that RA with pulmonary disease was associated with an increased risk of all-cause hospitalization / death (HR 1.26; 95% Cl 1.13-1.40), and the risk of respiratory related events increased nearly four times (HR 3.95; 95% Cl 3.20-4.88).Table 3: risk relationships of all-cause, respiratory related hospitalization and mortality between RA patients with pulmonary disease and those without pulmonary disease. A series of previous studies have shown that ILD is closely related to the prognosis of RA. At present, the biggest challenge for rheumatologists is to assess the risk stratification of ILD in RA patients.high resolution computed tomography (HRCT) is the gold standard for ra-ild diagnosis, but the cost and ionizing radiation limit its application in clinical practice.an oral report at the 2020 EULAR annual meeting (0p0038) [9] suggested that circulating biomarkers might be helpful for rheumatologists to assess the risk stratification of ILD in RA patients.the results show that KL-6 is related to the diagnosis and prognosis of ra-ild, and can be used as a circulating noninvasive first-line marker to assess the risk stratification of ILD in RA patients, so as to guide the use of HRCT.how to carry out lung rehabilitation training for patients with 4ra-ild? Reasonable, scientific and systematic respiratory training can effectively relieve the clinical symptoms of ra-ild patients, improve their lung function, and significantly reduce the impact of respiratory problems on patients' daily life.common pulmonary function exercise methods [10-13]: contraction lip abdominal breathing: Patients calm mood for 30 minutes, take half lying position, knee flexion.exhale through the mouth and inhale through the nose. When exhaling, the lips are retracted. At the same time, the abdominal muscles are forced to contract, and the abdominal wall will sink. At this time, the gas in the lung is slowly exhaled through the mouth, and the abdominal muscles are relaxed when inhaling, so as to make the abdomen bulge as much as possible.the time ratio of exhalation and inspiration is 2:1, about 10 breaths per minute, 10-15 minutes each time, 2-3 times a day.balloon blowing: choose a balloon with a capacity of 800-1000ML. The patient inhales deeply until the balloon can not be inhaled. Blow the air in the lung into the balloon as much as possible. Blow the balloon up several times to make the diameter of the balloon reach 5cm-30cm.10-15min / time, 2-3 times a day.resistance breathing training device: the breathing training device is composed of a shell, a float, a connecting pipe and a bite.take out the breathing training device, connect the connecting pipe with the interface of the shell and bite, and place it vertically to maintain normal breathing.hold the mouthpiece to inhale, and keep the float rising with deep and uniform suction flow for a long time as possible.remove the breathing apparatus and exhale.repeat step 2 and 3 for breathing training for 10-15 minutes, and then rest after normal breathing.physical function exercise: mainly includes gymnastics club chest expansion and body rotation.hold the gymnastic club under the armpit, lift and lower the gymnastic club up and down for chest expansion when inhaling and exhaling, and turn left and right side at the same time of inspiration or exhalation. each training lasted for 15 minutes, twice a day, 5 days a week. References: [1] Zhang Yangwen. Detection and significance of serum RF and CCP antibodies in rheumatoid arthritis [J]. Journal of practical medicine, 2015,31 (1): 108-109. [2] Ding Shuang, Duan Hongmei, Fang Fang, et al. Analysis of connective tissue growth factors in serum of patients with rheumatoid arthritis [J]. Journal of cell and molecular immunology, 2015,31 (1): 97-99. [3] Zheng Xuejun, Wang Xiaoxia, Research progress of rheumatoid arthritis complicated with interstitial lung disease [J]. Hebei Medical Journal, 2016,38 (11). [4] examination of international disease in patients with rheumatoid arthritis prevalance, time to set, and clinical characteristics.2020 Eular (Abstract:0P0035).doi:#!resources/examination-of-interstitial-lung-disease-in-patients-with-rheumatoid-arthritis-prevalence-time-to-onset-and-clinical-characteristics[5]Bes C. Comprehensive review of current diagnostic and treatment approaches to interstitial lung disease associated with rheumatoid arthritis[J]. European journal of rheumatology, 2019, 6(3): 146.[6]Lake F , Proudman S . Rheumatoid Arthritis and Lung Disease: From Mechanisms to a Practical Approach[J]. Semin Respir Crit Care Med, 2014, 35(02):222-238.[7]Methotrexate and Rheumatoid Arthritis associated Interstitial Lung Disease.2020 Eular (Abstract:0P0036).doi:#!resources/methotrexate-and-rheumatoid-arthritis-associated-interstitial-lung-disease[8]Hospitalization and mortality outcomes in rheumatoid arthritis patients with lung disease.2020 Eular (Abstract:0P0039).doi:#!resources/hospitalization-and-mortality-outcomes-in-rheumatoid-arthritis-patients-with-lung-disease[9]Improving risk-stratification of rheumatoid arthritis patients for interstitial lung disease.2020 Eular (Abstract: 0p0038). Doi: Resources / improving risk stratification of rheumatoid arthritis patients for interstitial lung disease [10] Luo Jian, Xu Yulan. Clinical nursing thinking and practice in rheumatology and Immunology [M]. People's Health Press, 2014. [11] ascherman D P. interactive lung disease in rheumatoid arthritis [J]. Current rheumatology reports, 2010, Chinese Journal of clinicians: electronic edition, 2013,7 (1): 185-187. [13] Ma Qiwen, Ou Yinghui, Lin Jiahong, et al. Effects of three kinds of respiratory training on pulmonary function in patients with rheumatoid arthritis complicated with interstitial pneumonia [J]. Journal of practical medical technology, 2016,23 (3): 315-316
This article is an English version of an article which is originally in the Chinese language on echemi.com and is provided for information purposes only.
This website makes no representation or warranty of any kind, either expressed or implied, as to the accuracy, completeness ownership or reliability of
the article or any translations thereof. If you have any concerns or complaints relating to the article, please send an email, providing a detailed
description of the concern or complaint, to
service@echemi.com. A staff member will contact you within 5 working days. Once verified, infringing content
will be removed immediately.