-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
The report was compiled and published
On August 27-28, 2022, the "2022 Second Frontier Study Class on Research Progress in the Prevention and Treatment of Endocrine and Metabolic Diseases" jointly organized by the Department of Endocrinology of Peking University People's Hospital and the Chinese Diabetes Magazine was officially held
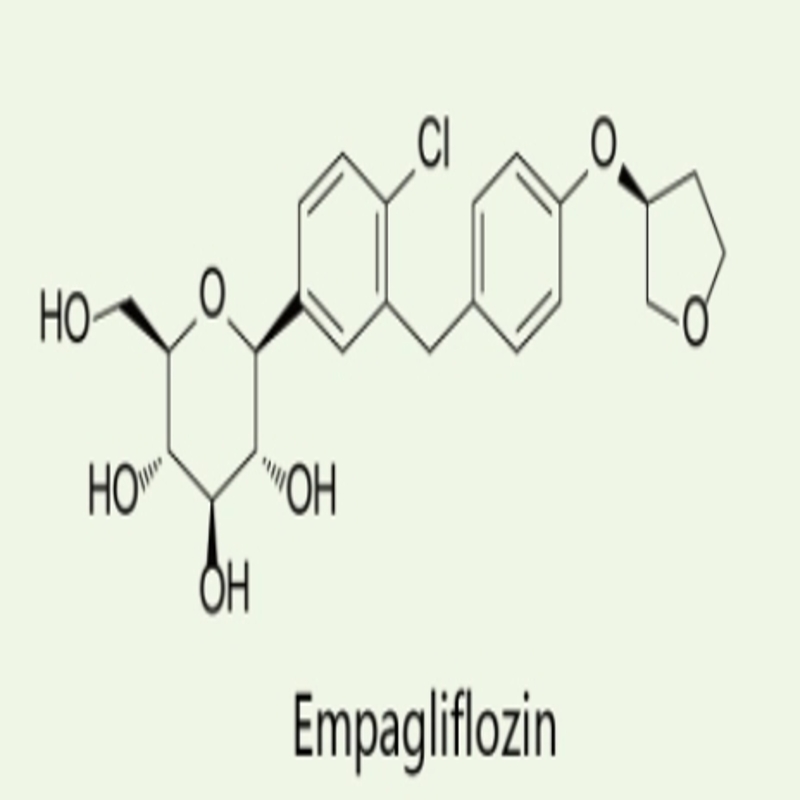
Based on evidence-based evidence- based medicine, Professor Cai Xiaoling answered 5 hot questions around SGLT2i (e.
Expert introduction
Cai Xiaoling
Chief Physician, Associate Professor, Doctoral Supervisor
Question 1: Is the efficacy of SGLT2i consistent and how safe is it in patients with different renal function?
The research team of Peking University People's Hospital provided the latest evidence-based medical evidence to answer this question, and the research report entitled "Meta-analysis of the differences in efficacy and safety of SGLT2i use in patients with different renal function" systematically evaluated the differences
The researchers searched
3.
4.
Figure 1 HbA1c and weight changes in patients with different renal function treated by SGLT2i
Figure 2 Blood pressure and eGFR changes in SGLT2i in patients with different renal function
Figure 3 Safety of SGLT2i in the treatment of patients with different renal functions
Table 1 SGLT2i treatment of hypoglycemia in patients with different renal function compared with placebo
Draw the point
➤In patients treated with SGLT2i, HbA1c and weight loss are usually parallel
to baseline eGFR levels.
➤ In patients treated with SGLT2i, a decrease in blood pressure was not associated
with baseline eGFR levels.
➤Patients with good renal function and decreased HbA1c are more likely to develop hypoglycemia
than placebo.
Question 2: Cardiovascular benefits beyond SGLT2i urine glucose excretion?
In 2022, the research team of Peking University People's Hospital published a study in the journal Dialoges Obes Metab, "Cardiovascular Benefits Beyond Urinary Glucose Excretion: Assumptions from Two Meta-Analyses", which explored this problem, and Professor Cai Xiaoling interpreted
the literature.
This study systematically assessed the association between SGLT2i in the treatment of urinary glucose excretion (UGE) and cardiovascular and renal outcomes
.
The researchers searched the PubMed/Medline, Embase and Cochrane, Clinicaltrial.
gov, Scopus, and Web of Science databases (before September 2021
).
Eligible trials were analyzed using fixed-effects models, random-effects models, and ANOVA trend tests
.
Outcomes included cardiac-renal endpoints [major adverse cardiovascular events (MACE), including nonfatal myocardial infarction, nonfatal stroke, or cardiovascular death], and heart failure (HF) compound outcomes (including hospitalization due to HF, emergency visit to HF, or cardiovascular death); Renal complex outcomes (including deterioration of renal function, end-stage renal disease, or death from kidney disease
).
Through the search, a total of 661 studies were screened out by UGE, of which 653 studies were excluded and 8 studies were included; A total of 2067 studies were screened for cardiac and renal outcomes, of which 2057 studies were excluded and 10 studies
were included.
The study found that even with significant weakening of UGE, the cardiogenic benefits of SGLT2i treatment in patients with severe renal insufficiency were preserved (Figure 4
).
Figure 4 Comparison of benefits of SGLT2i under different renal function conditions
Note: A, UGE changes in patients with different renal function; B, MACE occurs in patients with different renal function (major adverse cardiovascular events, including non-fatal myocardial infarction, non-fatal stroke or cardiovascular death); C, heart failure-related outcomes by renal function, including hospitalization due to HF, emergency visits to HF, or cardiovascular death; D, a combination of renal outcomes with different renal function, including deterioration of renal function, end-stage renal disease, or death
from kidney disease.
Draw the point
➤ Even in the case of significant weakening of UGE, the cardiac-renal benefits of SGLT2i treatment in patients with severe renal insufficiency are preserved;
➤ The reduction in the risk of MACE and HF compound outcomes in patients with severe renal insufficiency was significantly preserved, and the risk reduction in MACE and HF was more significant in people with low eGFR;
➤ Conversely, the renal benefits of SGLT2i appear to be dependent on eGFR, as a greater
reduction in risk was observed in patients with good renal function.
Therefore, the renal protection and cardiovascular protection mechanisms of SGLT2is may be different
.
Question three: Does SGLT2i cause changes in "plasma fasting glucagon levels"?
In 2021, the research team of Peking University People's Hospital published a study in the journal Eur J Pharmacol, "SGLT2i Increases Plasma Fasting Glucagon Levels in Diabetic Patients: A Meta-Analysis", which explored this problem, and Professor Cai Xiaoling interpreted
the literature.
This study systematically assessed the overall effect
of SGLT2i treatment on plasma fasting glucagon levels in patients with diabetes mellitus.
Studies
published before August 2020 in the PubMed/Medline, Embase, and Cochrane databases were searched.
Clinical trials
of glucagon changes before and after SGLT2i interventions in patients with type 1 and type 2 diabetes mellitus.
Eligible trials were analyzed using fixed-effects models, random-effects models, and meta-regression analyses
.
Through the search, a total of 430 studies were screened, of which 410 studies were excluded and 10 studies
were included.
The main study endpoint was a change in plasma fasting glucagon levels before and after SGLT2i use; The secondary study endpoints were changes in
fasting blood glucose levels, fasting insulin levels, and fasting plasma ketone levels before and after SGLT2i use.
The study found that:
1.
Compared with the non-SGLT2i control group, the plasma fasting glucagon level was significantly increased in the SGLT2i treatment group (WMD, 8.
35 pg/ml; 95% Cl, 2.
17-14.
54 pg/ml, P<0.
01).
2.
In the subgroup analysis, when analyzed according to the non-SGLT2i control group, the plasma fasting glucagon level in the SGLT2i treatment group was significantly higher than that in the placebo control subgroup (WMD, 3.
00pg/ml; 95% Cl, 2.
21-3.
80 pg/ml, P<0.
01) and active drug control subgroup (12.
18 pg/ml; 95%Cl,0.
66-23.
69pg/ml,P=0.
04)
。
Figure 5 Forest plot of plasma fasting glucagon levels in the SGLT2i treatment group and control group
3.
In subgroup analysis, when analyzing by disease type, plasma fasting glucagon level in T1DM patients was significantly increased after treatment with SGLT2i (WMD, 35.
00 pg/ml; 95% CI, 23.
61–46.
39 pg/ml, P<0.
01), while plasma fasting glucagon levels were not significantly increased<b10> in patients with T2DM.
Fig.
6 Forest plots were analyzed in a stratified subgroup of disease types to compare plasma fasting glucagon changes in the SGLT2i treatment group and the control group
4.
For the analysis of the uncontrolled group of trials, the plasma absolute fasting glucagon level after SGLT2i treatment was significantly higher than the baseline (WMD, 15.
38 pg/ml; 95%CI,0.
78–29.
99 pg/ml,P=0.
04)
Overall, significantly elevated in patients with T1DM (WMD, 53.
00 pg / ml; 95% CI, 45.
63–60.
37 pg/ml, P<0.
01), no significant increase<b10> in T2DM.
Figure 7 Forest plots were analyzed by disease type stratified subgroup to compare fasting glucagon changes at baseline and endpoint
5.
Meta-regression analysis showed that baseline characteristics, including age, proportion of male patients, course of diabetes mellitus, baseline HbA1c level, baseline fasting glucagon level were not related to changes in fasting glucagon after SGLT2i treatment; In addition, changes in FPG or fasting insulin levels after SGLT2i treatment were not associated
with changes in glucagon.
Draw the point
➤ SGLT2i intervention therapy increases plasma fasting glucagon levels in patients with diabetes mellitus;
➤ An increase in fasting glucagon may be associated with a decrease in fasting insulin, which may increase the glucagon/insulin ratio, making patients prone to ketosis;
➤ When using SGLT2i to lower diabetes, changes
that may accompany glucagon and insulin should be taken into account.
Individualized assessment of patients with diabetes may contribute to better treatment
with SGLT2i.
Question 4: Is the use of SGLT2i related to the occurrence of "diabetic retinopathy"?
In 2022, the research team of Peking University People's Hospital published a study in the journal Expert Rev Clin Pharmacol, "The Use of SGLT2i and the Association with the Risk of Diabetic Retinopathy and Other Eye Diseases: A Systematic Review and Meta-Analysis", which explored this problem, and Professor Cai Xiaoling made a literature interpretation
.
This study systematically assessed the association
between SGLT2i treatment and the occurrence of diabetic retinopathy.
The researchers searched
for studies published before October 2021 in the PubMed/Medline, Embase, and Cochrane databases.
Randomised controlled trials reporting on the incidence of diabetic retinopathy and other eye diseases in users and non-users of SGLT2i were included
.
Eligible trials were analyzed using fixed-effects models, random-effects models, and meta-regression analyses
.
The primary study endpoint was the relationship between SGLT2i use and the incidence of sugar mesh; The secondary study endpoint was the relationship between SGLT2i use and the incidence of glyconetic reticulum during the proliferation phase; The endpoint of the exploratory study was the relationship between
SGLT2i use and the incidence of other eye diseases (cataracts, glaucoma, macular degeneration, and vascular lesions).
Through the search, a total of 3013 studies were screened, of which 2965 studies were excluded and 48 studies
were included.
The study found that:
1.
The use of SGLT2i was not significantly associated with the occurrence of diabetic retinopathy (OR=0.
80, 95% CI, 0.
61-1.
06, P=0.
12).
Figure 8 Risk of diabetic retinopathy in patients treated with SGLT2i
2.
The use of SGLT2i was not significantly associated with the occurrence of sugar mesh in the proliferative period (OR=0.
83, 95% Cl, 0.
58-1.
17, P=0.
28).
Fig.
9 Risk of developing glycotic reticulum in patients treated with SGLT2i
3.
The use of SGLT2i is not significantly associated
with the occurrence of hemorrhage and retinal detachment.
Figure 10 Risk of bleeding in patients treated with SGLT2i
4.
Subgroup analysis: In patients with a < 10 years of disease, the use of SGLT2i was associated with a reduced risk of sugar mesh (Figure 11
).
Figure 11 Forest plots are analyzed in subgroups grouped by disease course
5.
Subgroup analysis: The use of SGLT2i was associated
with a reduced risk of sugar mesh compared to the active control group.
Figure 12 Subgroup analysis of forest plots grouped by control type
Draw the point
➤The use of SGLT2i was not significantly associated with the occurrence of diabetic retinopathy;
➤ In patients with a course of illness within 10 years, the use of SGLT2i is associated with a reduction in the risk of sugar mesh;
➤ Using SGLT2i as early as possible may bring greater eye benefits
.
Question 5: Is there a correlation between the use of SGLT2i and "lower extremity complications"?
In 2021, the research team of Peking University People's Hospital published a study on SGLT2i and Lower Limb Complications: An Updated Meta-analysis published in the journal Cardiovasc Diabetol to explore this problem, and Professor Cai Xiaoling interpreted
the literature.
This study systematically assessed the relationship between SGLT2i treatment and the risk of lower extremity complications and analyzed the associated factors
.
Using the PubMed, Medline, Embase, Cochrane, and clinicaltrial.
go websites, the researchers searched for studies
published between the beginning of the database and November 2020.
Randomized controlled studies of SGLT2i were included in which amputation, peripheral arterial disease and diabetic foot events
were reported.
The corresponding analysis is performed by fixed-effects models, random-effects models, and meta-regression analysis
.
Outcome indicators were the correlation between SGLT2i treatment and the risk of amputation, peripheral arterial disease and diabetic foot occurrence and related factors
.
Through the search, a total of 1223 studies were screened, of which 1184 studies were excluded and 39 randomized controlled studies were included.
The study found that:
1.
Compared with the non-SGLT2i control group, the risk of amputation was slightly increased in the SGLT2i treatment group (OR=1.
23, 95% CI: 1.
08-1.
40, P=0.
002).
2.
According to the type of study (cardiovascular and renal outcome test and efficacy and safety evaluation trial), the increased risk of amputation was mainly caused by cardiovascular and renal outcome tests (amputation risk: OR=1.
23, 95% C: 1.
07-1.
40, P=0.
003).
Figure 13 Risk of amputation in patients treated with SGLT2i
3.
Compared with the non-SGLT2i control group, the risk of peripheral arterial disease was slightly increased in the SGLT2i treatment group (OR=1.
21, 95% CI, 1.
03-1.
42, P=0.
02).
4.
According to the type of study (cardiovascular and renal outcomes trial and efficacy and safety evaluation trial), the increased risk of peripheral arterial disease was mainly caused by cardiovascular and renal outcome tests (OR=1.
24, 95% Cl:1.
05-1.
46, P=0.
01).
Figure 14 SGLT2i treats patients with peripheral arterial disease risk
5.
Subgroup analysis showed that only patients with diabetes mellitus, placebo-controlled studies, follow-up cycles>52 weeks were associated
with a significant increase in the risk of amputation.
Table 2 SGLT2i treats patients with the risk of amputation events
Table 3 SGLT2i treats patients with amputation, peripheral arterial disease and diabetic foot events
6.
The greater the degree of weight loss in the SGLT2i treatment group, the higher the
risk of amputation, peripheral artery disease and diabetic foot.
Table 4 Factors and risks associated with lower extremity complications in SGLT2i treatment patients
7.
The lower the baseline diastolic blood pressure and the greater the decrease in systolic and diastolic blood pressure in the SGLT2i treatment group, which were associated
with amputation, peripheral arterial disease and increased risk of diabetic foot, respectively.
Table 5 Factors and risks associated with lower extremity complications in patients treated with SGLT2i
Draw the point
➤ Patients treated with SGLT2i had a slight increased risk of amputation and peripheral arterial disease compared with patients treated with non-SGLT2i;
➤ In patients treated with SGLT2i, the more weight and blood pressure are reduced, the greater the risk of developing complications of the lower extremities;
➤ For patients at high risk of lower extremity complications, monitoring reduced body weight and blood pressure may be an important risk prevention measure
when using SGLT2i.