-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*Only for medical professionals to read and reference.
Explore and develop for decades, GLP-1RA drugs help blood sugar reach the standard
.
Reviewer: Professor Guo Lixin, Beijing Hospital National Geriatrics Center Hyperglycemia is a common feature of all diabetic patients
.
Long-term hyperglycemia can damage blood vessels throughout the body and increase the risk of a series of microvascular and macrovascular complications.
Hyperglycemia and other metabolic abnormalities have brought many harms to diabetic patients [1]
.
Studies have shown that for every 1% reduction in glycated hemoglobin (HbA1c), the risk of diabetic microvascular and macrovascular complications is significantly reduced [2]
.
It can be seen that "hypoglycemic" is an important part of the goal of comprehensive management of diabetes
.
In order to better meet the hypoglycemic needs of diabetic patients, new hypoglycemic drugs emerge one after another
.
The long development road of GLP-1RA has benefited from the continuous exploration of medical clinicians and scientific researchers.
The incretin drug glucagon-like peptide-1 receptor agonist (GLP-1RA) is a “rookie” in the hypoglycemic field.
", has attracted much attention due to its unique mechanism, hypoglycemic efficacy and multiple benefits
.
The development of GLP-1RA was a long and difficult process
.
From 1932, when La Barre first proposed the concept of incretin [3], to the birth of GLP-1RA, it has gone through decades of research
.
In 2009, exenatide was approved for marketing in China.
In 2011, the first GLP-1RA daily preparation liraglutide entered China.
In 2019, GLP-1RA weekly preparation dulaglutide was approved in China.
The 1RA weekly preparation semaglutide was successfully launched in China, and the GLP-1RA family gradually expanded
.
With the accumulation of evidence-based evidence, the status of GLP-1RA in diabetes treatment has been increasing day by day, and it has been recommended by major diabetes guidelines at home and abroad, opening a new chapter in diabetes drug treatment[4-6]
.
The pharmacological basis of GLP-1RA for hypoglycemic GLP-1RA exerts hypoglycemic effect by activating glucagon-like peptide-1 receptor (GLP-1R), stimulating insulin secretion and inhibiting glucagon secretion in a glucose concentration-dependent manner [5], thereby reducing the risk of hypoglycemia while effectively reducing blood sugar
.
Under physiological conditions, elevated glucose concentrations stimulate insulin secretion
.
Under the action of GLP-1RA, the above pathways are amplified
.
After GLP-1RA binds to GLP-1R on β cells, adenylate cyclase (AC) is activated, which increases the level of cyclic adenosine monophosphate (cAMP) in cells, thereby prompting islet β cells to secrete more insulin.
Hypoglycemic effect [7-10]
.
At the same time, GLP-1RA can increase glucose uptake in muscle and adipose tissue, and inhibit the production of hepatic glucose to further exert hypoglycemic effect [5]
.
In addition, GLP-1RA can improve β-cell function in patients with type 2 diabetes (T2DM) by bidirectionally regulating islet α- and β-cells, reducing β-cell apoptosis, reducing inflammatory cell infiltration, and reducing lipotoxicity.
β-cell sensitivity to glucose, promote insulin secretion, and significantly reduce insulin resistance [11-14]
.
Trace back to the source, and manage blood sugar from the root cause of diabetes
.
Strong and safe, GLP-1RA significantly improves the compliance rate Good blood sugar control is the fundamental benefit of T2DM throughout the whole process.
In the face of difficult blood sugar control, GLP-1RA prescription that effectively lowers blood sugar without increasing the risk of hypoglycemia is an ideal choice for patients
.
I Evidence-based, how does GLP-1RA safely lower blood sugar? The safe hypoglycemic effect of GLP-1RA daily preparation liraglutide has been verified in large clinical studies
.
The LEAD series studies and the LIRA-DPP-4 study showed [15-21] that liraglutide can significantly reduce HbA1c (p < 0.
05), by as much as 1.
6%, regardless of whether it is used alone or in combination with other oral hypoglycemic agents or insulin.
, and significantly reduced fasting blood glucose (FPG) and postprandial blood glucose (PPG)
.
A meta-analysis of the LEAD series of studies [22] found that compared with other control drugs, T2DM patients treated with liraglutide 1.
8mg and 1.
2mg achieved the composite target rate (HbA1c<7% + no hypoglycemia + no weight gain).
) was significantly higher than that of other hypoglycemic drugs
.
It can be seen that liraglutide has both hypoglycemic efficacy and safety, and no weight gain, meeting the multiple needs of diabetes management
.
The large-scale clinical study of GLP-1RA weekly preparation confirmed its safe hypoglycemic effect
.
The AWARD series of studies have shown that the hypoglycemic effect of dulaglutide is better than that of other hypoglycemic drugs such as metformin, sitagliptin, exenatide, and insulin glargine
.
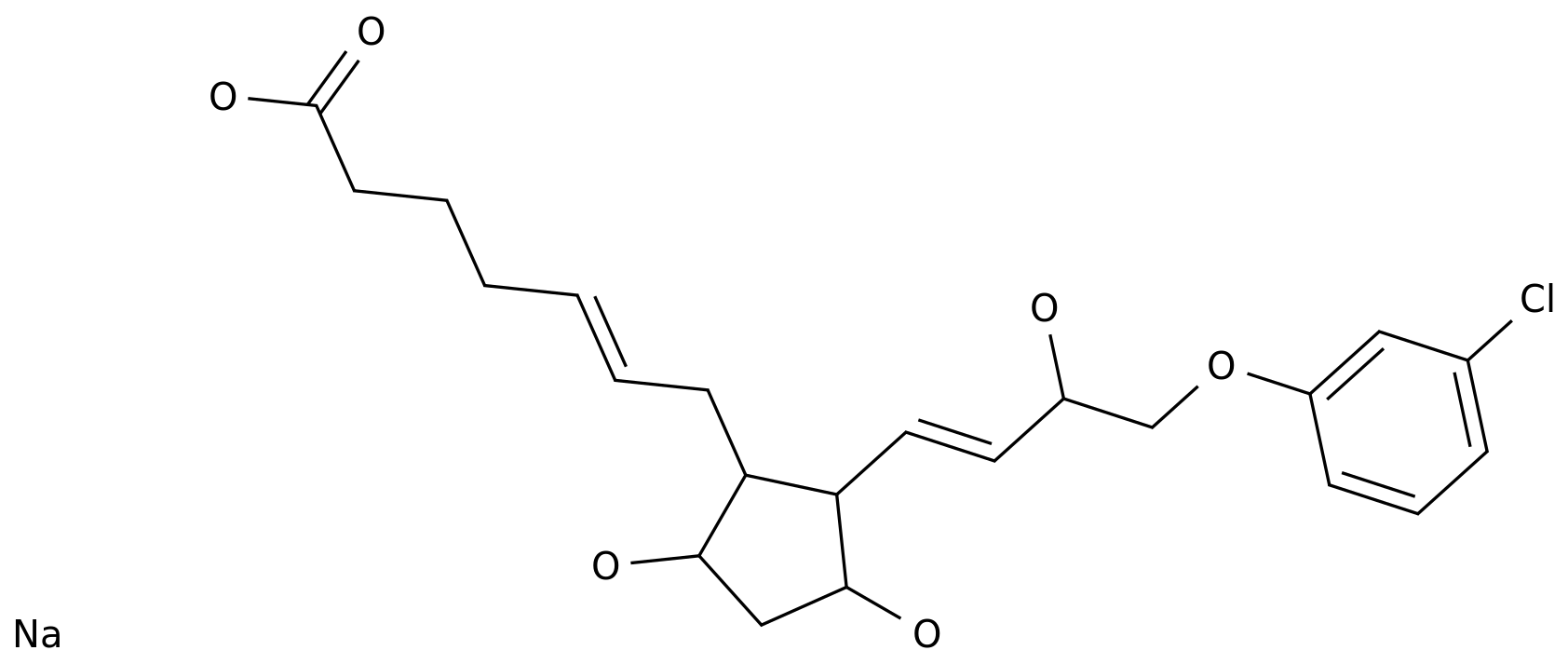
The SUSTAIN series of studies have shown [23-30] that semaglutide can significantly reduce HbA1c (p < 0.
05), with a maximum reduction of 1.
8%, regardless of whether it is used alone or in combination with other oral hypoglycemic agents or insulin (Figure 1)
.
Semaglutide achieves target HbA1c (<7%) in approximately 80% of T2DM patients without increasing the risk of hypoglycemia
.
Figure 1 Semaglutide is effective in lowering blood sugar, significantly reducing HbA1c by 1.
8%.
The analysis of the SUSTAIN study showed that [31], regardless of background treatment and the duration of diabetes, semaglutide significantly reduced HbA1c, and with baseline With the increase of HbA1c, the hypoglycemic extent of semaglutide increases.
In patients with baseline HbA1c greater than 9%, semaglutide can significantly reduce HbA1c by 2.
7%, helping blood sugar reach the target
.
The SUSTAIN China study [32] showed that after semaglutide treatment, the HbA1c compliance rate (<7%) of T2DM patients was as high as 86.
1%, suggesting that semaglutide has significantly reduced blood sugar in Chinese and global studies.
curative effect
.
A meta-analysis of 296 clinical trials (264,087 participants) of 296 clinical trials (264,087 participants) that included metformin in addition to some GLP-1RA or insulin showed that HbA1c reduction was higher in metformin in addition to some GLP-1RA or insulin.
Among them, the patients treated with semaglutide had the highest average HbA1c amplitude of 1.
33% (Figure 2)
.
Figure 2 On the basis of metformin, semaglutide combined with semaglutide can effectively lower blood sugar, and the HbA1c range can reach 1.
33%
.
Among GLP-RA drugs, weekly preparations are widely used in clinical practice, and one injection per week can effectively control glucose
.
Dulaglutide is injected once a week, 1.
5mg each time
.
The dose of semaglutide can be adjusted according to the individual situation of the patient, usually the recommended starting dose is 0.
25mg once a week (QW); after 4 weeks, it can be increased to 0.
5mg QW; after at least 4 weeks of treatment with 0.
5mg QW , the dose can be increased to 1 mg once a week, and self-monitoring of blood glucose is not required to adjust the dose of this product
.
Clinically, the application of weekly preparation GLP-1RA has significantly improved the compliance of patients
.
In addition, the study showed that after a single subcutaneous injection of semaglutide 0.
5 mg for subjects with different liver function status, the blood concentration of semaglutide was detected.
Pharmacokinetic parameters were not significantly affected [34]; this is also true in patients with impaired renal function, and semaglutide was tested after a single subcutaneous injection of semaglutide 0.
5 mg in subjects with different renal function status Changes in the plasma concentration of glutide, after adjusting for factors such as age and gender, impaired renal function had no significant effect on the pharmacokinetic parameters of semaglutide[35]
.
Therefore, no dose adjustment is required for patients with mild, moderate or severe hepatic and renal impairment
.
Summary: The burden of diabetes is becoming heavier, and reaching blood glucose targets is the cornerstone of diabetes management
.
In the field of diabetes, GLP-1RA has become a rising "new star", taking into account the effective hypoglycemic and cardiovascular benefits, which is undoubtedly an ideal choice for the treatment of T2DM
.
The GLP-1RA weekly preparation, the flexibility of injection and the convenience of the program, provide a favorable help for patients to reach the blood sugar target
.
It is expected that GLP-1RA drugs can be applied to more patients, help patients achieve blood sugar standards, improve patients' quality of life and clinical outcomes, and open a new chapter in hypoglycemia
.
Expert Profile Professor Guo Lixin, National Geriatrics Center, Beijing Hospital, Chief Physician, Professor, and Doctoral Supervisor, Institute of Geriatrics, Chinese Academy of Medical Sciences Vice President of Beijing Medical Association Executive Director of Beijing Medical Association President of Endocrinologist Branch of Beijing Medical Association The editor-in-chief enjoys special allowances from the State Council References: [1]Paul S,et al.
J Diabetes Complications.
2020 Aug;34(8):107613.
[2]Stratton IM,et al.
BMJ.
2000 Aug 12;321(7258) :405-12.
[3]Nature Milestones in Diabetes.
https:// Branch of Chinese Medical Association.
Chinese Journal of Practical Internal Medicine.
2018; 38(04):292-344.
[5]Diabetes Branch of Chinese Medical Association.
International Journal of Endocrinology and Metabolism.
2021;41(05):482-548.
[6]Diabetes Care.
2022 Jan;45(Suppl 1): S1-S264.
[7]Drucker DJ.
Cell Metab 2006;3:153–165.
[8]Hinke SA et al.
J Physiol 2004;558:369–380.
[9]Henquin JC.
Diabetes.
2000;49: 1751–1760.
[10]Henquin JC.
Diabetes.
2004;53:S48–S58.
[11]Shao Y,et al.
Peptides.
2014 Feb;52:134-42.
[12]Luo X,et al.
J Diabetes.
2013 Dec;5(4):421-428.
[13]Shao S,et al.
J Cell Biochem.
2014 Jun;115(6):1166-75.
[14]Grigoropoulou P, et al.
Curr Diabetes Rev.
2013;9(5):412-7.
[15]Marre et al.
Diabet Med.
2009;26;268–278.
[16]Nauck et al.
Diabetes Care.
2009;32;84–90.
[17]Garber et al.
Lancet.
2009;373:473–481.
[18]Zinman et al.
Diabetes Care.
2009;32:1224–1230.
[19]Russell- Jones et al.
Diabetologia.
2009;52:2046–2055.
[20]Buse et al.
Lancet.
2009;374:39–47.
[21]Pratley et al.
Lancet.
2010:375;1447–1456.
[22 ] Zinman, et al.
Diabetes Obes Metab.
2012; 14: 77–82.
[23] Sorli C, et al.
Lancet Diabetes Endocrinol.
2017; 5: 251–60.
[24] Ahrén B, et al.
Lancet Diabetes Endocrinol.
2017;5:341–54.
[25]Ahmann AJ,et al.
Diabetes Care.
2018;41:258–66.
[26]Aroda VR,et al.
Lancet Diabetes Endocrinol.
2017;5:355–66 .
[27]Rodbard HW, et al.
J Clin Endocrinol Metab.
2018;103:2291–301.
[28]Pratley RE, et al.
Lancet Diabetes Endocrinol.
2018;6:275–86.
[29]Lingvay I, et al.
Lancet Diabetes Endo, crinol.
2019;7(11):834-844.
[30]Zinman B,et al.
Lancet Diabetes Endocrinol.
2019;7:356-67.
[31]Linong Ji,et al.
Diabetes Obes Metab.
2020;22:303-314.
[32]Ji,et al.
Diabetes Obes Metab.
2021; 23(2):404-14.
[33]Tsapas A, et al.
Ann Intern Med 2020;173:278–286.
[34]Jensen L, et al.
Diabetes Obes Metab.
2018;20:998–1005.
[35] Marbury TC, et al.
Clin Pharmacokinet.
2017;56:1381–90.
-End- "This article is only used to provide scientific information to medical and health professionals, and does not represent the platform's position" Contribution/Reprint/Business cooperation, Please contact: pengsanmei@yxj.
org.
cn