-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Source: Endocrinology Branch of Chinese Medical Association
Pituitary diseases are often accompanied by endocrine hormone disorders, tumor mass effects, and multiple comorbidities, and the epidemic of novel coronavirus infection (new crown infection) makes its management much more difficult
.
Therefore, the proposal of this clinical response guideline aims to standardize the clinical diagnosis and treatment of pituitary diseases during new crown infection, strengthen the treatment of comorbidities, and provide reference and guidance for the comprehensive management of pituitary diseases
.
Patients with pituitary disease often have endocrine hormone disorders and tumor mass effects, involving multidisciplinary management and follow-up
.
There is no clinical evidence of direct damage to the pituitary gland by SARS-CoV-2, but studies suggest that there may be some disturbance in pituitary function
.
A considerable number of patients with pituitary diseases combined with hypopituitarism, diabetes, hypertension, obesity and cardiovascular diseases, etc.
, may affect the treatment and management of new crown infection, bringing great challenges
.
In order to further standardize the comprehensive management of pituitary diseases infected with the new crown, our expert team has formulated the following clinical response guidelines
.
1.
Management of pituitary diseases
Regular endocrine hormone measurements and pituitary imaging evaluation are particularly necessary
in all patients with pituitary disease.
Patients with new-onset pituitary lesions or suspected hypopituitarism are recommended for prompt evaluation
.
A morning cortisol level of <3 micrograms/dL indicates adrenal insufficiency, > 15 micrograms/dL is excluded, and ambulatory testing is usually required at intermediate values
.
Low free thyroxine and low/or normal TSH are often suggestive of central hypothyroidism
.
Patients with tumors that are close to or compressing the optic chiasmatic nerve are recommended for regular eye examinations, including the patient's self-report and visual field assessment
.
Patients with pituitary tumors with severe vision loss should seek early medical attention
.
Patients with diabetes insipidus need to be concerned about electrolytes, water intake, and urine output, and be alert to electrolyte and fluid balance disturbances
.
Patients with functional pituitary tumors with severe clinical symptoms, or who have a strong clinical suspicion of significant changes or adverse reactions to treatment, should present promptly
.
Patients with functional pituitary tumors who are in remission or with well-controlled medical therapy are advised to maintain the original regimen
.
Patients receiving pituitary hormone replacement therapy are supplemented with a starting dose of hydrocortisone 15-25 mg / day, taken
in divided doses.
In areas at high risk of COVID exposure, alternative doses of hydrocortisone are preferably close to the upper limit of the normal range to reduce the risk
of adrenal insufficiency crisis.
In the absence of severe cardiac disease, a reasonable starting dose of thyroid hormone replacement is about 50-75 micrograms/day, with the goal of dose adjustment being to bring free thyroxine to an upper-intermediate level in the normal range
.
If possible, adequate reserves of pituitary hormone replacement drugs should be made, and cortisone and levothyroxine sodium
should not be stopped without authorization.
In addition, patients who stop growth hormone and sex hormone replacement in the short term pose less risk
to health.
1.
Prolactinoma
A detailed medication history should be sought and secondary causes, including primary hypothyroidism
, should be carefully evaluated.
A history of psychiatric and psychotropic use is important before initiating dopamine agonist therapy, and tolerance should be observed during treatment
.
Patients with macroadenomas should be concerned about visual impairment, improve visual field assessment, and carefully weigh the risks and benefits
of surgical intervention if necessary.
2.
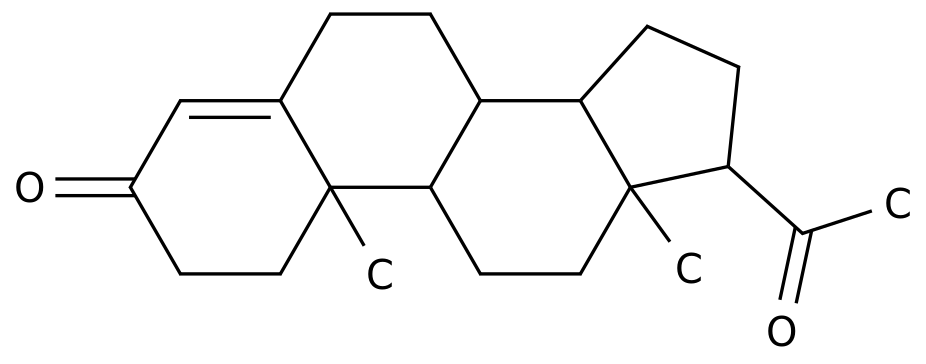
Acromegaly
Transnasal sphenoid pituitary surgery is the treatment
of choice.
Patients with visual impairment due to tumor compression should undergo prompt surgery
.
Patients with elevated levels of growth hormone and IGF-1 that do not cause visual deterioration may be considered for pharmacotherapy, including short- or long-acting somatostatin receptor analogues (SRLs) and growth hormone receptor antagonists, and treatment options should be individualized
.
For patients treated with long-acting SRL, increase the dose of SRL to reduce the frequency
of injections if necessary.
During the application of SRL, patients should eat a light diet, avoid greasy, and if there is abdominal pain and other discomfort, they should see a doctor
as soon as possible.
3.
Cushing's disease
There is considerable heterogeneity in the clinical phenotype of Cushing disease
.
Patients with highly specific symptoms such as easy bruising, hirsutism, broad purple striae, proximal limb weakness, and hypokalemia require prompt medical attention for screening and treatment
.
Postoperative adrenal insufficiency in patients receiving glucocorticoid replacement should increase glucocorticoid replacement dose if symptoms of underlying infection or inadequate replacement are present, balancing the risk of
overreplacement.
Active patients receiving cortisol-lowering drugs should be aware of a history of abnormal liver and kidney function, and regularly monitor liver function, renal function, and electrolytes during medication
.
The starting dose of cortisol should be reduced as small as possible and increased slowly to avoid adrenal insufficiency, and oral corticosteroids
can be used at home if necessary.
If the patient presents with fever, cortisol-lowering agents should be discontinued and seen promptly, and specialist consultation should be consulted for resumption of therapy
.
4.
Non-functional pituitary tumor
When the patient does not have tumor compressive symptoms, the evaluation period
for non-functioning pituitary tumors can be appropriately extended.
If your condition changes, you need to seek medical attention
promptly.
5.
Hypopituitarism and vacuolar sella syndrome
In asymptomatic or mild infections, the usual replacement dose of oral corticosteroids is doubled in hypopituitaristic patients, progressing to 20 mg of hydrocortisone every 6 hours in moderately infected patients, and switching to intravenous glucocorticoid infusions (hydrocortisone is preferred)
in severely infected patients.
Pay attention to water-electrolyte balance, especially if you have
fever, shortness of breath, diarrhoea, and/or vomiting.
Central diabetes insipidus should avoid hyponatremia and, if necessary, delay or reduce desmopressin administration to reduce dilutive hyponatremia
due to excessive water intake.
Vacuolar sella syndrome such as normal pituitary function, combined with new crown infection treatment is the same as the general population, and patients with abnormal function should be treated
appropriately.
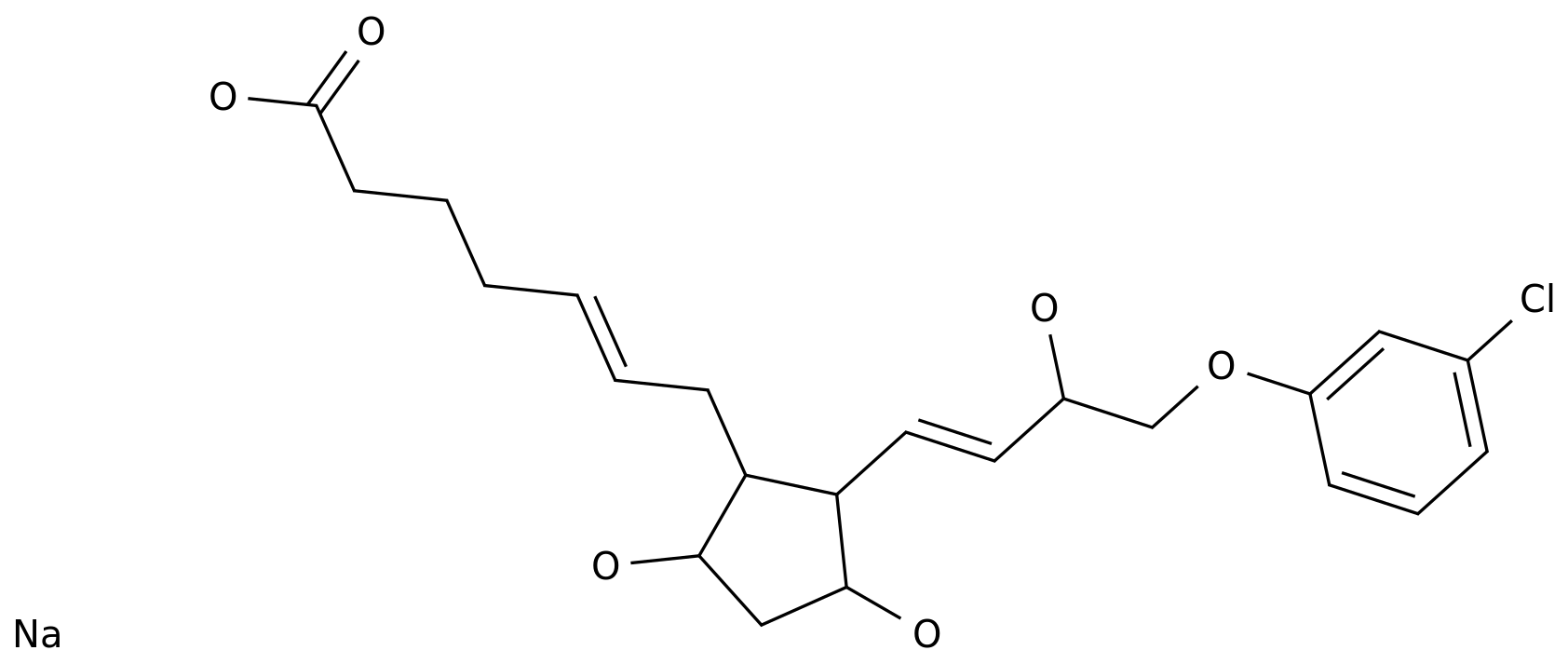
Second, the management of pituitary disease comorbidities
Given the immunosuppressive effect of hypercortisolemia, patients are at increased risk of infection when Cushing's disease is not controlled
.
Functional pituitary tumors, including Cushing's disease, often have a combination of metabolic and cardiovascular diseases that increase the risk of death
.
Patients with pituitary disorders, particularly Cushing disease and acromegaly, recommend aggressive treatment and monitoring
for comorbidities such as hypertension, diabetes, hyperlipidemia, osteoporosis, heart failure, and sleep apnea.
According to the principle of stratified management, it is comprehensively managed
of blood glucose, blood pressure and blood lipid level.
Given the increased risk of venous thromboembolism, consider regular activity and/or prophylactic low molecular weight heparin therapy if permitted, while monitoring bleeding risk
.
Patients with functional pituitary tumors receiving pharmacologic therapy to control high hormone levels must be closely followed up and re-dosed for comorbid conditions, particularly insulin, other glucose-lowering drugs, antihypertensive drugs, and potassium supplementation once the drug dose is changed or discontinued
.
Third, the acute state of pituitary disease response
1.
Adrenal insufficiency
Prompt and adequate glucocorticoid replacement should be performed, with concern for symptoms such as anorexia, weight loss, diarrhea, hyponatremia, and/or hyperkalemia
.
Other anterior pituitary hormone deficiencies should also be assessed
.
Patients with suspected adrenal insufficiency crisis should consider early use of stress-dose glucocorticoids
.
2.
Pituitary stroke
The possibility of pituitary stroke is of high concern, particularly in known pituitary adenomas, pregnant women, and people
taking antiplatelet drugs.
Initial evaluation of suspected pituitary stroke can be based on typical clinical findings, including acute onset of severe headache, nausea/vomiting, decreased vision, diplopia, ptosis, and impaired consciousness
.
Clinical assessment of visual field of vision, cranial nerves, and level of consciousness helps confirm the severity of
the disease.
Urgent arrangements should be made for patients to undergo a CT scan of the brain for differential diagnosis, particularly with subarachnoid haemorrhage and meningitis, and further refinement of pituitary MRI scan
if available.
Supportive measures to ensure hemodynamic stability and stress-dose glucocorticoid therapy are recommended, with reassessment of anterior pituitary hormone deficiency after 6 weeks
.
In addition, ongoing neurological and ophthalmologic monitoring is required, with regular examination of blood electrolytes
.
3.
Evaluation of the hypothalamic-pituitary-adrenal (HPA) axis in patients treated with glucocorticoids for new crown infection
In patients with new crown infection treated with dexamethasone, no impaired adrenal cortex function was found, so routine assessment of adrenal cortex function
was not necessary.
In patients receiving glucocorticoids for <3 weeks in the acute phase of the disease, clinically significant suppression of the HPA axis rarely occurs
.
HPA axis suppression is unavoidable in patients taking ≥ 15 mg/day prednisolone ≥for 3 weeks and can be evaluated
after reduction and cessation of glucocorticoid use.
4.
Life management of patients with pituitary diseases
Pay attention to personal hygiene, practice social distancing, avoid cold, and reduce the risk of
infection.
Ensure adequate sleep, relax your mood, have a regular schedule, and avoid overwork
.
Balanced nutrition, avoid greasy diet, reduce food intake with high glycemic index, control weight, strengthen self-monitoring
of blood sugar and blood pressure.
Pay attention to mental health, for patients with mental illnesses such as depression and anxiety, it is necessary to take medication regularly and regularly go to a specialist for evaluation
.
Appropriate exercise should be selected when permitted, and regular activity can help reduce the risk
of venous thromboembolism.
It is important to note that strenuous exercise should be avoided to reduce the risk of
fracture.
If there is any change or discomfort, go to the hospital in time
.
Members of the expert group that developed this guide
(The following is sorted by last name stroke):
Wang Weiqing Ruijin Hospital, Shanghai Jiao Tong University School of Medicine
Ningguang Ruijin Hospital affiliated to Shanghai Jiao Tong University School of Medicine
Mu Yiming, Chinese General Hospital of the People's Liberation Army
Cheng Jinluo Changzhou Second People's Hospital affiliated to Nanjing Medical University
Zhu Dalong Drum Tower Hospital Affiliated to Nanjing University School of Medicine
Liu Libin Union Hospital, Fujian Medical University
Liu Jianmin Ruijin Hospital Affiliated to Shanghai Jiao Tong University School of Medicine
Li Ling Shengjing Hospital Affiliated to China Medical University
Xiao Haipeng The First Affiliated Hospital of Sun Yat-sen University
Weiwei Zhou Ruijin Hospital, Shanghai Jiao Tong University School of Medicine
Zhongyan Shan The First Affiliated Hospital of China Medical University
Zhao Zhigang Zhengzhou Summer Hospital, Henan University
Zhao Jiajun Affiliated Provincial Hospital of Shandong First Medical University
Ji Qiuhe Xijing Hospital, Air Force Military Medical University
Disclaimer: This platform is designed to deliver more medical information
to healthcare professionals.
The content published on this platform cannot replace professional medical guidance in any way, nor should it be regarded as diagnosis and treatment advice
.
If such information is used for purposes other than understanding medical information, this platform does not assume relevant responsibilities
.
The content published by this platform does not mean that it agrees with its description and views
.
If copyright issues are involved, please contact us and we will deal with
it as soon as possible.