-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*For medical professionals only to read reference
lupus nephritis descending step treatment, realized!
The annual American College of Rheumatology (ACR) Annual Meeting has just ended, as a gathering of the most cutting-edge research in the field of rheumatology and immunity, the ACR Annual Meeting has always attracted the attention
of clinicians at home and abroad.
At the meeting, Professor Maria Dall'Era from Rheumatology at the University of California, San Francisco, gave a wonderful report
on the new progress in the treatment of lupus nephritis (LN).
In line with the purpose of "spreading the strongest voice of rheumatism and creating a new academic fashion", the Rheumatology and Immunology Channel of the Medical Community specially invited Professor Zhang Hui, a youth committee member of the Rheumatology Branch of the Chinese Medical Association and the First Affiliated Hospital of Sun Yat-sen University, to explain this content
.
This article sorts out the key points and shares the academic feast
with everyone.
LN: How to pursue the minimization of drug toxicity
Rethinking LN: Step-down treatmentHere, Professor Zhang Hui first introduced a case: a 31-year-old woman who was diagnosed with SLE 1 year ago, with cheek erythema, mouth ulcers, wrist arthritis and small arthritis
.
Laboratory tests: ANA(+) 1:160, normal anti-dsDNA (+), anti-Sm (+), C3, and C4
.
Hydroxychloroquine (HCQ) 200mg/day, MTX 12.
5mg/wk, prednisone 5mg/day
.
The above symptoms are well controlled
.
The patient developed nocturia, eye swelling, and foot/ankle swelling in the past 4 weeks
.
Further related examinations: physical examination:
blood pressure 160/90mmHg, P 90 times/min; Mild periorbital edema; normal cardiopulmonary capacity; Symmetrical moderate edema of the plantar of the
foot.
Laboratory tests: normal blood routine, SCr 0.
90mg/dl (eGFR 82ml/min), antinuclear antibody 1:
160, anti-dsDNA antibody 65 IU/ml, C3 45g/L, C4 10g/L
.
Urine test: RBC 11-20, WBC 5-10 urine protein-to-creatinine ratio 4.
4
.
Renal biopsy: IV+V LN, activity index: 9/24, chronic index: 2/12, no vascular involvement
.
Professor Zhang Hui pointed out that rheumatologists often encounter such conditions
in the clinic.
Renal involvement is evident and treatment should be adjusted
.
The traditional treatment strategy for LN is glucocorticoids plus immunosuppressants, and if the patient does not respond to treatment, switch regimens or use biologics such as rituximab
.
In traditional regimens, immunosuppressants are mainly mycophenolate mofetil or cyclophosphamide
.
LN therapy now has more immunosuppressants/immunomodulators, mainly including belimumab, which targets B lymphocyte stimulating factor (BAFF), and Voclosporin
, a novel calcineurin inhibitor.
Therefore, there are more options for the treatment of LN
.
Compared to the traditional ascending ladder therapy for LN therapy, Professor Maria Dall'Era proposed a new strategy for LN therapy at this ACR Annual Meeting and defined it as descending step therapy: combination of immunosuppressants/immunomodulators as the initial treatment regimen
.
Over time, the drug is adjusted according to the patient's response, and there is a chance to stop the drug
.
So, what is the rationale for the paradigm shift in treatment?
Professor Zhang Hui shared that traditional treatment options have great limitations:
1 incomplete renal response and long induction time;
2.
High rate of relapse of kidney disease;
3.
Chronic renal insufficiency, end-stage renal disease and high mortality rates;
4.
Long-term use of glucocorticoids is associated with more side effects;
5.
Traditional immunosuppressants are poorly tolerated
.
Considering the relevant mechanism of LN kidney injury, early treatment and response of LN is essential to protect the patient's kidney function, and the kidney is time!
of LN treatment.
Belimumab, a recombinant human IgG1λ monoclonal antibody that inhibits the survival of B cells (including autoreactive B cells) and reduces the differentiation of B cells into plasma cells by binding to BAFF, has been approved for use in patients 5 years of age or older with active autoantibody positive SLE and adult patients
with active LN who are receiving standard therapy.
BLISS-LN is a large phase III, multi-country, multicenter RCT study of 448 patients with renal biopsy-confirmed LN types III, IV, and/or V with inclusion criteria: urine protein/creatinine ratio (UPCR) > 1, eGFR > 30 ml/min
.
The objective is to evaluate the efficacy and safety of belimumab in combination with standard therapy (mycophenolate mofetil or cyclophosphamide) in patients with active LN[2].
The results showed that after 2 years of treatment, belimumab combined with standard therapy improved the rate of complete renal remission in patients with active LN, reduced the risk of worsening of kidney disease, and improved the long-term prognosis
of patients.
As a novel calcineurin inhibitor, voltroxysporine inhibits IL-2 expression and T cell-mediated immune response, while stabilizing renal podocytes
.
The FDA has approved fluciclosporin in combination with immunosuppressants for the treatment of active LN
in adults.
A multicenter, randomized, double-blind phase III RCT study (AURORA1) conducted in 142 hospitals in 27 countries evaluated the efficacy and safety of combining with mycophenolate in combination with cyclosporine for LN in addition to standard care (mycophenolate mofetil) [3].
。 The study included 357 patients with renal biopsy-confirmed LN types III, IV, and/or V, and included criteria: UPCR> 1.
5/2 g; eGFR >45 ml/min
。 In this pivotal phase III clinical trial, LN patients receiving amvuclosporine plus standard therapy achieved a significantly higher proportion of patients with LN achieving complete renal remission at week 52 than in the standard therapy group
.
Combined with the data from the above clinical studies and the inclusion criteria, the combination regimen of belimumab or vorciclosporin in addition to standard treatment for LN has shown better results
than standard therapy.
In the selection of combination treatment regimen, Professor Zhang Hui gave the following suggestions for combination treatment regimen for different types of LN patients:
with eGFR≥45ml/min, no obvious chronization on renal biopsy, and high proteinuria (≥3g).
In addition, combination therapy with cyclosporine is more appropriate if the patient prefers oral pharmacotherapy/is able to adhere to oral pharmacotherapy
.
The combination of other drugs for the treatment of LN is not supported
by high-quality clinical studies.
A small real-world retrospective study from Japan showed that belimumab in combination with tacrolimus in patients with LN reduced recurrence of kidney disease and maintained low disease activity
.
In combination with biologics, data from two phase II clinical trials exploring the sequential use of belimumab after rituximab treatment for refractory LN show that rituximab combined with belimumab is generally safe, can more effectively clear B cells and reduce patients' autoantibody levels, but the effectiveness of its combination in the treatment of LN remains to be confirmed by further multicenter large-sample randomized controlled RCTs
。
Combination therapy for LN: What should we think about?
Finally, Professor Zhang Hui raised several questions about the combination treatment of LN and thought together with everyone:
1 How do patients be graded and the right treatment plan taken?
2. Which therapies are used to treat flare-ups and which are used to maintain quiescence?
3. Can diagnosis and intervention be made early in the course of the disease or in 'high-risk' populations?
4. how long it should be treated; Should we finally stop treatment?
5. How can patient adherence to treatment be maximized? Expert profiles
lupus nephritis descending step treatment, realized!
The annual American College of Rheumatology (ACR) Annual Meeting has just ended, as a gathering of the most cutting-edge research in the field of rheumatology and immunity, the ACR Annual Meeting has always attracted the attention
of clinicians at home and abroad.
At the meeting, Professor Maria Dall'Era from Rheumatology at the University of California, San Francisco, gave a wonderful report
on the new progress in the treatment of lupus nephritis (LN).
In line with the purpose of "spreading the strongest voice of rheumatism and creating a new academic fashion", the Rheumatology and Immunology Channel of the Medical Community specially invited Professor Zhang Hui, a youth committee member of the Rheumatology Branch of the Chinese Medical Association and the First Affiliated Hospital of Sun Yat-sen University, to explain this content
.
This article sorts out the key points and shares the academic feast
with everyone.
LN: How to pursue the minimization of drug toxicity
LN is a common and serious complication of systemic lupus erythematosus (SLE), and about 40%~60% of SLE patients will develop LN
.
It is reported that LN is the disease with the highest mortality rate in the organs and systems affected by SLE, which seriously threatens the health and life of patients, and is characterized by the deposition of glomerular immune complexes and subsequent inflammatory responses
.
LN is not only a common and serious complication of SLE, but also an important cause
of kidney injury and end-stage renal disease in SLE patients.
At present, the main treatment goal of LN is to control the disease and avoid progression to chronic kidney disease
.
Although the prognosis of patients with LN has improved over the past few decades, there are still problems such as
unsatisfactory complete response rates, slow treatment responses, and high incidence of adverse effects.
In recent years, people have not only paid attention to the effectiveness of LN drug treatment, but also pursued the minimization
of drug toxicity.
[1]
Rethinking LN: Step-down treatmentHere, Professor Zhang Hui first introduced a case: a 31-year-old woman who was diagnosed with SLE 1 year ago, with cheek erythema, mouth ulcers, wrist arthritis and small arthritis
.
Laboratory tests: ANA(+) 1:160, normal anti-dsDNA (+), anti-Sm (+), C3, and C4
.
Hydroxychloroquine (HCQ) 200mg/day, MTX 12.
5mg/wk, prednisone 5mg/day
.
The above symptoms are well controlled
.
The patient developed nocturia, eye swelling, and foot/ankle swelling in the past 4 weeks
.
Further related examinations: physical examination:
blood pressure 160/90mmHg, P 90 times/min; Mild periorbital edema; normal cardiopulmonary capacity; Symmetrical moderate edema of the plantar of the
foot.
Laboratory tests: normal blood routine, SCr 0.
90mg/dl (eGFR 82ml/min), antinuclear antibody 1:
160, anti-dsDNA antibody 65 IU/ml, C3 45g/L, C4 10g/L
.
Urine test: RBC 11-20, WBC 5-10 urine protein-to-creatinine ratio 4.
4
.
Renal biopsy: IV+V LN, activity index: 9/24, chronic index: 2/12, no vascular involvement
.
Professor Zhang Hui pointed out that rheumatologists often encounter such conditions
in the clinic.
Renal involvement is evident and treatment should be adjusted
.
The traditional treatment strategy for LN is glucocorticoids plus immunosuppressants, and if the patient does not respond to treatment, switch regimens or use biologics such as rituximab
.
In traditional regimens, immunosuppressants are mainly mycophenolate mofetil or cyclophosphamide
.
LN therapy now has more immunosuppressants/immunomodulators, mainly including belimumab, which targets B lymphocyte stimulating factor (BAFF), and Voclosporin
, a novel calcineurin inhibitor.
Therefore, there are more options for the treatment of LN
.
Compared to the traditional ascending ladder therapy for LN therapy, Professor Maria Dall'Era proposed a new strategy for LN therapy at this ACR Annual Meeting and defined it as descending step therapy: combination of immunosuppressants/immunomodulators as the initial treatment regimen
.
Over time, the drug is adjusted according to the patient's response, and there is a chance to stop the drug
.
So, what is the rationale for the paradigm shift in treatment?
Professor Zhang Hui shared that traditional treatment options have great limitations:
1 incomplete renal response and long induction time;
2.
High rate of relapse of kidney disease;
3.
Chronic renal insufficiency, end-stage renal disease and high mortality rates;
4.
Long-term use of glucocorticoids is associated with more side effects;
5.
Traditional immunosuppressants are poorly tolerated
.
Considering the relevant mechanism of LN kidney injury, early treatment and response of LN is essential to protect the patient's kidney function, and the kidney is time!
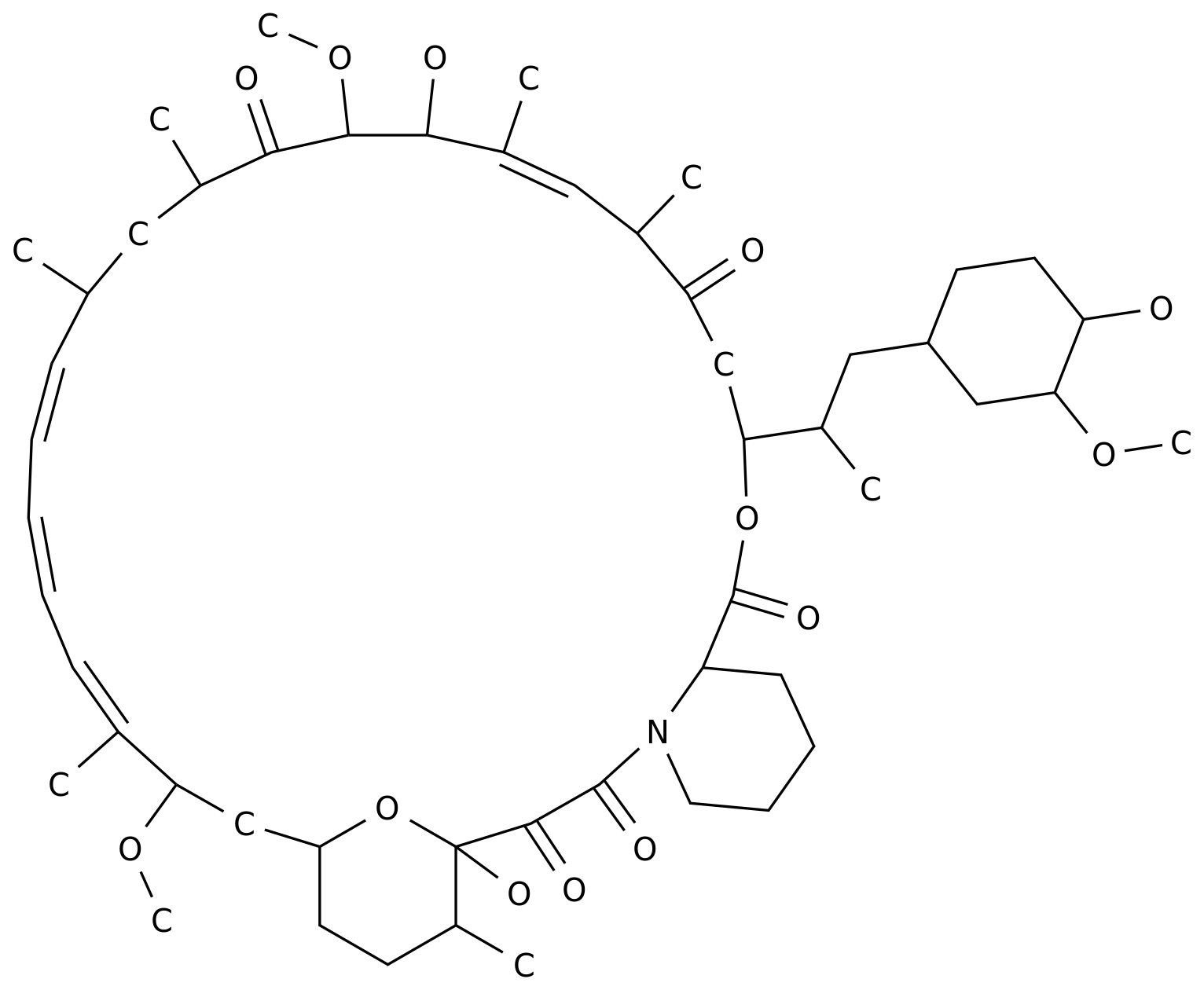
Fig.
1 Mechanisms related to LN kidney injury
RCTs were used as a starting point to explore "individualized" LN combination regimens
of LN treatment.
Belimumab, a recombinant human IgG1λ monoclonal antibody that inhibits the survival of B cells (including autoreactive B cells) and reduces the differentiation of B cells into plasma cells by binding to BAFF, has been approved for use in patients 5 years of age or older with active autoantibody positive SLE and adult patients
with active LN who are receiving standard therapy.
BLISS-LN is a large phase III, multi-country, multicenter RCT study of 448 patients with renal biopsy-confirmed LN types III, IV, and/or V with inclusion criteria: urine protein/creatinine ratio (UPCR) > 1, eGFR > 30 ml/min
.
The objective is to evaluate the efficacy and safety of belimumab in combination with standard therapy (mycophenolate mofetil or cyclophosphamide) in patients with active LN[2].
The results showed that after 2 years of treatment, belimumab combined with standard therapy improved the rate of complete renal remission in patients with active LN, reduced the risk of worsening of kidney disease, and improved the long-term prognosis
of patients.
As a novel calcineurin inhibitor, voltroxysporine inhibits IL-2 expression and T cell-mediated immune response, while stabilizing renal podocytes
.
The FDA has approved fluciclosporin in combination with immunosuppressants for the treatment of active LN
in adults.
A multicenter, randomized, double-blind phase III RCT study (AURORA1) conducted in 142 hospitals in 27 countries evaluated the efficacy and safety of combining with mycophenolate in combination with cyclosporine for LN in addition to standard care (mycophenolate mofetil) [3].
。 The study included 357 patients with renal biopsy-confirmed LN types III, IV, and/or V, and included criteria: UPCR> 1.
5/2 g; eGFR >45 ml/min
。 In this pivotal phase III clinical trial, LN patients receiving amvuclosporine plus standard therapy achieved a significantly higher proportion of patients with LN achieving complete renal remission at week 52 than in the standard therapy group
.
Combined with the data from the above clinical studies and the inclusion criteria, the combination regimen of belimumab or vorciclosporin in addition to standard treatment for LN has shown better results
than standard therapy.
In the selection of combination treatment regimen, Professor Zhang Hui gave the following suggestions for combination treatment regimen for different types of LN patients:
● Compared with vocyclosporine, belimumab is more suitable for patients with LN with eGFR≤45 ml/min and/or significant chronicized renal biopsy and low proteinuria (<3 g<b10>).
In addition, belilumab is more appropriate if the patient has a significant history of infection/safety concerns, has difficulty adhering to oral therapy or prefers injectable therapy, or has concomitant extrarenal disease such as cutaneous lupus erythematosus or arthritis
.
with eGFR≥45ml/min, no obvious chronization on renal biopsy, and high proteinuria (≥3g).
In addition, combination therapy with cyclosporine is more appropriate if the patient prefers oral pharmacotherapy/is able to adhere to oral pharmacotherapy
.
The combination of other drugs for the treatment of LN is not supported
by high-quality clinical studies.
A small real-world retrospective study from Japan showed that belimumab in combination with tacrolimus in patients with LN reduced recurrence of kidney disease and maintained low disease activity
.
In combination with biologics, data from two phase II clinical trials exploring the sequential use of belimumab after rituximab treatment for refractory LN show that rituximab combined with belimumab is generally safe, can more effectively clear B cells and reduce patients' autoantibody levels, but the effectiveness of its combination in the treatment of LN remains to be confirmed by further multicenter large-sample randomized controlled RCTs
。
Combination therapy for LN: What should we think about?
Finally, Professor Zhang Hui raised several questions about the combination treatment of LN and thought together with everyone:
1 How do patients be graded and the right treatment plan taken?
2. Which therapies are used to treat flare-ups and which are used to maintain quiescence?
3. Can diagnosis and intervention be made early in the course of the disease or in 'high-risk' populations?
4. how long it should be treated; Should we finally stop treatment?
5. How can patient adherence to treatment be maximized? Expert profiles
Professor Zhang Hui
Doctor of Medicine, Doctoral Supervisor
Deputy Director of the Department of Rheumatology and Immunology of the First Affiliated Hospital of Sun Yat-sen University
Independent PI of the Institute of Precision Medicine
Selected for the National Young Talents Program
Guangdong Province "Pearl River Talent Program" young top-notch talents
Sun Yat-sen University's "Hundred Talents Program" young and middle-aged outstanding talents
National Youth Committee Member of Rheumatology Branch of Chinese Medical Association
He has been engaged in clinical and scientific research of rheumatic and immuno-related diseases for a long time, presided over the National Natural Science Foundation of China and other funds, and published more than 30 papers, including the first (including co-)author in Cell Research, Cell Discovery,Molecular He has published more than 10 papers in international journals such as Therapy, PNAS, and Circulation
.
[1] LI Wanxing, ZHOU Xiaoshuang, LI Rongshan.
Recent progress in the treatment of lupus nephritis[J].
Journal of Clinical Nephrology, 2022,22(08):696-700
[2]Furie R, Rovin B H, Houssiau F, et al.
Two-Year, Randomized, Controlled Trial of Belimumab in Lupus Nephritis[J].
N Engl J Med, 2020,383(12):1117-1128.
DOI:10.
1056/NEJMoa2001180.
[3] Rovin B H, Teng Y, Ginzler E M, et al.
Efficacy and safety of voclosporin versus placebo for lupus nephritis (AURORA 1): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial[J].
Lancet, 2021,397(10289):2070-2080.
DOI:10.
1016/S0140-6736(21)00578-X.