-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
-
Cosmetic Ingredient
- Water Treatment Chemical
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*Only for medical professionals to read and learn! On May 20-22, 2021, the 25th Academic Conference of Rheumatology Branch of Chinese Medical Association was held in Shenzhen, Guangdong Province.
During the meeting, Zhang Yuqi from the First Affiliated Hospital of Zhengzhou University shared with you a rare case.
This article summarizes the content of this case and learns with everyone~ Case introduction The patient was a 51-year-old female who suffered from "50 days of rash on both lower limbs and 20 knee joints with swelling and pain".
Tian" was admitted to the hospital.
50 days ago, the patient developed scattered erythema on both lower limbs, bright red, protruding from the surface of the skin, and accompanied by pain.
The local county hospital received anti-inflammatory and analgesic treatment (specifically unknown), but the effect was not good.
More than 20 days ago, the patient developed pain in both lower limbs with mild concave edema, pain in the shoulders, elbows, wrists, knee joints, and bilateral sternoclavicular joints without swelling.
The patient had been to the local city hospital, and the blood examination routine: WBC↑16.
6×109/L, PLT↑438×109/L, Hb↓58.
0g/L; Inflammation indicators: ESR (ESR) ↑35mm/h, C-reactive protein (CRP) ↑ 12.
10 mg/L; Immune indicators: ANA+dsDNA+ENA, ANCA, anti-ACL (-); CT of the lung: a little inflammation in the left lingual lobe and right middle lobe; lower limb skin biopsy: "panniculitis" The pathological changes; bone marrow smears: 1.
Bone marrow hyperplasia is active, the proportion of granulocytes is slightly higher, the erythroid is normal, the lymphocytes are not abnormal, and there are a lot of megakaryocytes and platelets.
3.
No blood parasites were seen.
In the treatment, small doses of hormones, hydroxychloroquine, levofloxacin, etc.
were given for more than 1 week, but the effect was poor, the edema of both lower limbs was reduced, and the pain was not relieved.
For further diagnosis and treatment, the patient was admitted to the outpatient clinic on 2019-01-07, and was admitted to the hospital with the "cause of erythema nodule".
When admitted to the hospital, he was conscious, less energetic, able to eat and sleep, and there was no significant change in weight.
Past history, personal history, and family history are normal.
▌ Admission examination: T 36.
2℃, P 89 times/min, R 22 times/min, Bp 89/57mmHg.
Both lower limbs are scattered with erythema nodules, the size of a red date (see Figure 1), accompanied by pain.
Both knee joints are swollen, tender, and restricted in movement.
The superficial lymph nodes were not palpable, and the cardiopulmonary examination (-).
The abdomen is flat, without tenderness or rebound pain, and the abdomen is soft and without lumps.
The liver and spleen are not palpable under the ribs, Murphy's sign is negative, there is no percussive pain in the left and right kidney areas, mobile dullness is negative, and bowel sounds are normal.
Figure 1 The appearance of erythema on both lower extremities on admission ▌ On the second day of admission: The patient developed fever and his body temperature fluctuated between 38.
5°C and 39°C.
▌ Laboratory test: blood routine: WBC↑17.
4×109/L, NE↑14.
55×109/L; Hb↓58.
0g/L, PLT 341×109/L; liver function: ALT↑102U/L, AST↑54U /L, ALP↑143U/L, LDH↑659U/L.
Blood coagulation: D-dimer ↑4.
71mg/L; blood lipids, renal function, urine routine, stool routine (-).
Inflammation indicators: ESR↑64mm/h, CRP↑135.
43mg/L; Ferritin↑156.
5ng/mL, C3, C4, IgG, IgA, IgM (-); Immune indicators: ANA+dsDNA+ENAs (-); ANCA (-); RF+CCP+MCV+AKA+APF(-); Infection index: PCT↑0.
42ng/ml, T-spot(-), EBV-IgG(+), CMV-IgG(+); EBV- IgM, EBV-DNA, CMV-IgM, CMV-DNA (-); infectious diseases: HBV, HCV, HIV (-). ▌ Imaging examination: echocardiography: mild tricuspid valve insufficiency, decreased left ventricular diastolic function; abdominal ultrasound: liver diffuse echo changes, but no abnormalities; genitourinary ultrasound: kidneys, ureters, and bladder are not obvious Abnormal, there is no obvious abnormality in the uterus and appendages, the position of the intrauterine contraceptive device is normal; superficial lymph node ultrasound: there are no obvious abnormal enlarged lymph nodes in the upper and lower clavicle, axillae, and groin; lung CT: slight inflammation in both lungs.
In addition, the patient perfected the bone marrow smear + bone marrow culture, the result was negative, and the blood culture was negative; the patient had persistent fever, the reason is not clear, it is recommended to further improve the PET-CT examination.
PET-CT (see Figure 2): 1.
There are multiple soft tissue density nodules under the skin of both buttocks, lower extremities and feet.
Metabolism is active.
Consider inflammatory lesions.
2.
The high-density nodules in the oblique fissure of the left lower lobe have no abnormality in metabolism; double pneumonia; no abnormality in the local thickening of the bilateral pleura; no abnormality in the metabolism of the mediastinal lymph nodes.
Consider chronic inflammation.
3.
Poor gasification of the left frontal sinus; bilateral sphenoid sinus and right maxillary sinusitis; right tonsil calcification.
4.
Low-density nodules in the left lobe of the thyroid have no abnormalities in metabolism.
5.
After the uterine contraceptive device is inserted.
Figure 2 PET-CT lower limb skin pathology (see Figure 3): Panniculitis with fat necrosis, consider non-specific.
Initial diagnosis: Panniculitis.
Treatment: Methylprednisolone tablets (16mg tid), anti-infection, liver protection, stomach protection, calcium supplementation, maintenance of water and electrolyte balance and other symptomatic and supportive treatments, and if necessary, pain relief and fever.
Body temperature can be controlled, but the effect is not good.
Figure 3 Pathological manifestations of the skin of the lower extremities.
On the 7th day of admission, the knee joint pain increased, with tenderness and swelling, and the pain was like a knife cut.
Right knee MRI (see Figure 4): Irregular low-intensity shadows were seen on T1WI, and irregular high-intensity shadows were seen on T2WI for fat compression.
Figure 4 Right knee MRI Right knee MRI showed multiple abnormal signals on the right lower femur, upper tibia, and patella.
Considering the possibility of systemic disease bone marrow infiltration or ischemic changes or inflammation.
2.
Diffuse edema in the soft group around the right knee joint. 3.
Fluid effusion in the articular cavity and suprapatellar capsule of the right knee.
The MRI of the left knee is the same as above.
After 13 days of admission, dark red erythema nodules appeared in the upper limbs and hip area, with a diameter of about 2cm-3cm, which was higher than the skin surface (see Figure 5), and there was no sense of fluctuation.
Figure 5 The appearance of upper limb erythema 13 days after admission ▌ Another skin biopsy (see Figure 6): First report: hyperkeratosis of the epidermis, thickening of the spinous layer, lymphocytes, eosinophil infiltration, and adipose tissue around the blood vessels in the dermis Large areas of necrosis, with more proliferation of lymphocytes, foam-like tissue cells, plasma cells and fibrous tissue cells, and nuclear debris at the edges of necrosis.
The lesions showed panniculitis-like changes.
PAS, hexaamine silver, acid-fast staining and TB have been performed.
-DNA check, the results will be issued separately.
Communicate the patient's medical history and clinical manifestations with the pathology department.
The second report: Panniculitis, fat tissue necrosis is obvious, it is recommended that pancreatic panniculitis be excluded from pancreatic examination.
Special dyeing: PAS (-), hexaamine silver (-), anti-acid (-).
Figure 6 Pathological manifestations of upper extremity erythema Therefore, it is recommended that patients further improve pancreatic related indicators and abdominal CT examination: amylase ↑ 671.
0 U/L (0-220 U/L), lipase ↑ 551.
8 U/L (13-60 U/L), Tumor markers(-).
Enhanced CT of the upper abdomen (see Figure 7): Cystic lesions behind the head of the pancreas, pancreatic pseudocyst formation? The patchy calcification density shadow can be seen inside, and the enhancement seems to be the enhancement of the cyst wall, please combine with the clinical.
Figure 7 The upper abdomen enhanced CT follow-up medical history: 3 months ago, there was a transient abdominal pain without treatment.
Final diagnosis: panniculitis, polyarthritis and pancreatitis syndrome (PPP syndrome).
This patient has a cyst (inflammation or tumor?) behind the head of the pancreas, pancreatic panniculitis, and polyarthritis.
Combining the relevant literature, let's understand that PPP syndrome ~ PPP syndrome is a rare disease.
The population is mainly middle-aged men, with a peak of 50-60 years old.
Most patients have a history of heavy drinking. PPP syndrome is related to pancreatic related diseases such as acute/chronic pancreatitis, pancreatic cancer (usually pancreatic carcinoma), neuroendocrine tumor, insulinoma, pancreatic division, pancreatic vascular fistula, traumatic pancreatitis, and pancreatic duct stenosis.
The pathogenesis is not clear.
It may be that excessive secretion of trypsin increases the permeability of the microcirculation, and lipase and amylase enter the fat lobules, leading to the dissolution of subcutaneous fat and intramedullary fat, and secondary inflammatory reactions.
About two-thirds of patients have no obvious abdominal symptoms, which can easily lead to misdiagnosis and missed diagnosis of pancreatic disease.
Panniculitis is more common in the lower extremities, with painful/painless reddish-brown nodules (0.
5cm-5cm), which can form aseptic abscesses, some of which may ulcer spontaneously, and exudate viscous, chylo-like aseptic fat necrosis.
Arthritis mainly affects the ankle, knee, metacarpophalangeal joints, etc.
It can be single joint, oligo-joint or multiple joints at the same time, with multiple joints being the most common.
In laboratory tests, most lipase and amylase are elevated, and some patients are normal, and the degree of pancreatin elevation does not match the severity of the disease.
In imaging examinations, pancreatic diseases can be detected by abdominal ultrasound and enhanced CT.
MRI can confirm intramedullary necrosis.
The typical manifestation is that the lesion is low-intensity shadow on T1WI and high-intensity shadow on T2WI lipid phase.
X-ray films show osteolytic damage to the cortex around the joints and worm-like changes.
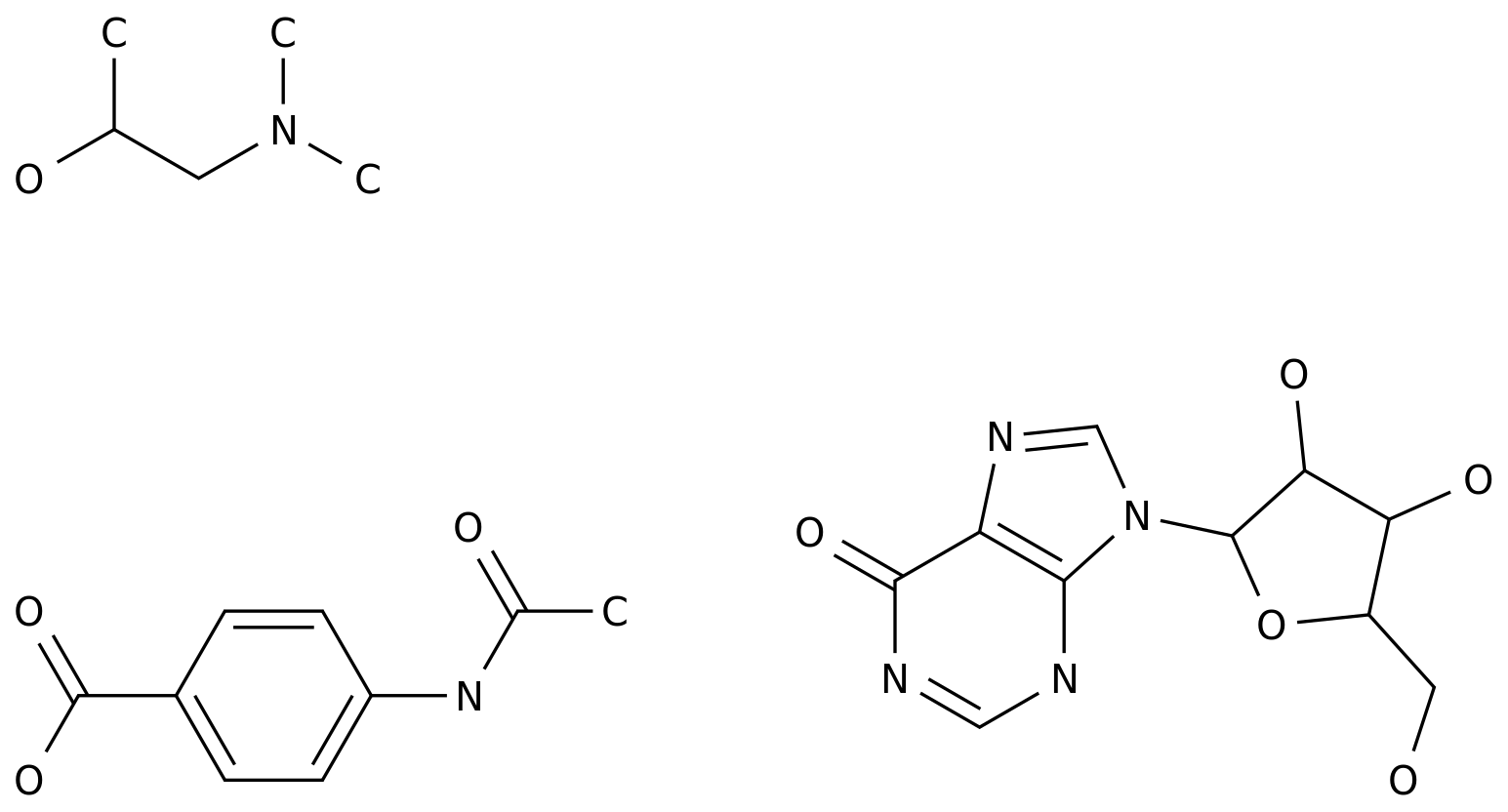
Pathological manifestations (see Figure 8): focal fat necrosis, mainly fat lobule necrosis without vasculitis.
Fat cells form thick-walled "ghost" cells without nucleus.
There are varying degrees of fine spot-like basophilic calcium salt deposition and infiltration of neutrophils, lymphocytes, foam-like cells, and multinucleated giant cells in the edges of necrotic fat or in fat cells.
Figure 8 Pathological manifestations The treatment and prognosis of this disease depend on pancreatic disease, which requires active recognition and effective treatment.
Acute/chronic pancreatitis is mainly treated conservatively; pancreatic tumors are treated by chemotherapy or surgery; pancreatic pseudocysts are often removed by fluid drainage, surgery or endoscopy.
The use of hormones and non-steroidal anti-inflammatory drugs (NSAIDs) is controversial, and long-term large-scale use is not recommended; some panniculitis and osteoarthritis lesions of PPP syndrome respond poorly to hormones.
In this case, fasting, fluid rehydration, proton pump inhibitors, somatostatin analogs, methylprednisolone, and leflunomide were given treatment.
The patient's rash subsided significantly, and the swelling and pain of both knee joints were relieved compared with before.
Recheck the pancreas-related indicators (see Table 1).
Table 1 Changes in related indicators of the pancreas.
Conclusion: PPP syndrome is a rare disease with rapid progress and poor prognosis.
Patients often have no obvious abdominal symptoms, which can easily delay diagnosis and treatment.
When unexplained erythema nodosa/panniculitis and arthralgia occur, consider pancreatic panniculitis and PPP syndrome.
Sensitive examination methods are expected to improve the efficiency of diagnosis and treatment, but at present, histopathology is still the gold standard for diagnosis of this disease.
Treating pancreatic related problems is the key to treating this disease.
During the meeting, Zhang Yuqi from the First Affiliated Hospital of Zhengzhou University shared with you a rare case.
This article summarizes the content of this case and learns with everyone~ Case introduction The patient was a 51-year-old female who suffered from "50 days of rash on both lower limbs and 20 knee joints with swelling and pain".
Tian" was admitted to the hospital.
50 days ago, the patient developed scattered erythema on both lower limbs, bright red, protruding from the surface of the skin, and accompanied by pain.
The local county hospital received anti-inflammatory and analgesic treatment (specifically unknown), but the effect was not good.
More than 20 days ago, the patient developed pain in both lower limbs with mild concave edema, pain in the shoulders, elbows, wrists, knee joints, and bilateral sternoclavicular joints without swelling.
The patient had been to the local city hospital, and the blood examination routine: WBC↑16.
6×109/L, PLT↑438×109/L, Hb↓58.
0g/L; Inflammation indicators: ESR (ESR) ↑35mm/h, C-reactive protein (CRP) ↑ 12.
10 mg/L; Immune indicators: ANA+dsDNA+ENA, ANCA, anti-ACL (-); CT of the lung: a little inflammation in the left lingual lobe and right middle lobe; lower limb skin biopsy: "panniculitis" The pathological changes; bone marrow smears: 1.
Bone marrow hyperplasia is active, the proportion of granulocytes is slightly higher, the erythroid is normal, the lymphocytes are not abnormal, and there are a lot of megakaryocytes and platelets.
3.
No blood parasites were seen.
In the treatment, small doses of hormones, hydroxychloroquine, levofloxacin, etc.
were given for more than 1 week, but the effect was poor, the edema of both lower limbs was reduced, and the pain was not relieved.
For further diagnosis and treatment, the patient was admitted to the outpatient clinic on 2019-01-07, and was admitted to the hospital with the "cause of erythema nodule".
When admitted to the hospital, he was conscious, less energetic, able to eat and sleep, and there was no significant change in weight.
Past history, personal history, and family history are normal.
▌ Admission examination: T 36.
2℃, P 89 times/min, R 22 times/min, Bp 89/57mmHg.
Both lower limbs are scattered with erythema nodules, the size of a red date (see Figure 1), accompanied by pain.
Both knee joints are swollen, tender, and restricted in movement.
The superficial lymph nodes were not palpable, and the cardiopulmonary examination (-).
The abdomen is flat, without tenderness or rebound pain, and the abdomen is soft and without lumps.
The liver and spleen are not palpable under the ribs, Murphy's sign is negative, there is no percussive pain in the left and right kidney areas, mobile dullness is negative, and bowel sounds are normal.
Figure 1 The appearance of erythema on both lower extremities on admission ▌ On the second day of admission: The patient developed fever and his body temperature fluctuated between 38.
5°C and 39°C.
▌ Laboratory test: blood routine: WBC↑17.
4×109/L, NE↑14.
55×109/L; Hb↓58.
0g/L, PLT 341×109/L; liver function: ALT↑102U/L, AST↑54U /L, ALP↑143U/L, LDH↑659U/L.
Blood coagulation: D-dimer ↑4.
71mg/L; blood lipids, renal function, urine routine, stool routine (-).
Inflammation indicators: ESR↑64mm/h, CRP↑135.
43mg/L; Ferritin↑156.
5ng/mL, C3, C4, IgG, IgA, IgM (-); Immune indicators: ANA+dsDNA+ENAs (-); ANCA (-); RF+CCP+MCV+AKA+APF(-); Infection index: PCT↑0.
42ng/ml, T-spot(-), EBV-IgG(+), CMV-IgG(+); EBV- IgM, EBV-DNA, CMV-IgM, CMV-DNA (-); infectious diseases: HBV, HCV, HIV (-). ▌ Imaging examination: echocardiography: mild tricuspid valve insufficiency, decreased left ventricular diastolic function; abdominal ultrasound: liver diffuse echo changes, but no abnormalities; genitourinary ultrasound: kidneys, ureters, and bladder are not obvious Abnormal, there is no obvious abnormality in the uterus and appendages, the position of the intrauterine contraceptive device is normal; superficial lymph node ultrasound: there are no obvious abnormal enlarged lymph nodes in the upper and lower clavicle, axillae, and groin; lung CT: slight inflammation in both lungs.
In addition, the patient perfected the bone marrow smear + bone marrow culture, the result was negative, and the blood culture was negative; the patient had persistent fever, the reason is not clear, it is recommended to further improve the PET-CT examination.
PET-CT (see Figure 2): 1.
There are multiple soft tissue density nodules under the skin of both buttocks, lower extremities and feet.
Metabolism is active.
Consider inflammatory lesions.
2.
The high-density nodules in the oblique fissure of the left lower lobe have no abnormality in metabolism; double pneumonia; no abnormality in the local thickening of the bilateral pleura; no abnormality in the metabolism of the mediastinal lymph nodes.
Consider chronic inflammation.
3.
Poor gasification of the left frontal sinus; bilateral sphenoid sinus and right maxillary sinusitis; right tonsil calcification.
4.
Low-density nodules in the left lobe of the thyroid have no abnormalities in metabolism.
5.
After the uterine contraceptive device is inserted.
Figure 2 PET-CT lower limb skin pathology (see Figure 3): Panniculitis with fat necrosis, consider non-specific.
Initial diagnosis: Panniculitis.
Treatment: Methylprednisolone tablets (16mg tid), anti-infection, liver protection, stomach protection, calcium supplementation, maintenance of water and electrolyte balance and other symptomatic and supportive treatments, and if necessary, pain relief and fever.
Body temperature can be controlled, but the effect is not good.
Figure 3 Pathological manifestations of the skin of the lower extremities.
On the 7th day of admission, the knee joint pain increased, with tenderness and swelling, and the pain was like a knife cut.
Right knee MRI (see Figure 4): Irregular low-intensity shadows were seen on T1WI, and irregular high-intensity shadows were seen on T2WI for fat compression.
Figure 4 Right knee MRI Right knee MRI showed multiple abnormal signals on the right lower femur, upper tibia, and patella.
Considering the possibility of systemic disease bone marrow infiltration or ischemic changes or inflammation.
2.
Diffuse edema in the soft group around the right knee joint. 3.
Fluid effusion in the articular cavity and suprapatellar capsule of the right knee.
The MRI of the left knee is the same as above.
After 13 days of admission, dark red erythema nodules appeared in the upper limbs and hip area, with a diameter of about 2cm-3cm, which was higher than the skin surface (see Figure 5), and there was no sense of fluctuation.
Figure 5 The appearance of upper limb erythema 13 days after admission ▌ Another skin biopsy (see Figure 6): First report: hyperkeratosis of the epidermis, thickening of the spinous layer, lymphocytes, eosinophil infiltration, and adipose tissue around the blood vessels in the dermis Large areas of necrosis, with more proliferation of lymphocytes, foam-like tissue cells, plasma cells and fibrous tissue cells, and nuclear debris at the edges of necrosis.
The lesions showed panniculitis-like changes.
PAS, hexaamine silver, acid-fast staining and TB have been performed.
-DNA check, the results will be issued separately.
Communicate the patient's medical history and clinical manifestations with the pathology department.
The second report: Panniculitis, fat tissue necrosis is obvious, it is recommended that pancreatic panniculitis be excluded from pancreatic examination.
Special dyeing: PAS (-), hexaamine silver (-), anti-acid (-).
Figure 6 Pathological manifestations of upper extremity erythema Therefore, it is recommended that patients further improve pancreatic related indicators and abdominal CT examination: amylase ↑ 671.
0 U/L (0-220 U/L), lipase ↑ 551.
8 U/L (13-60 U/L), Tumor markers(-).
Enhanced CT of the upper abdomen (see Figure 7): Cystic lesions behind the head of the pancreas, pancreatic pseudocyst formation? The patchy calcification density shadow can be seen inside, and the enhancement seems to be the enhancement of the cyst wall, please combine with the clinical.
Figure 7 The upper abdomen enhanced CT follow-up medical history: 3 months ago, there was a transient abdominal pain without treatment.
Final diagnosis: panniculitis, polyarthritis and pancreatitis syndrome (PPP syndrome).
This patient has a cyst (inflammation or tumor?) behind the head of the pancreas, pancreatic panniculitis, and polyarthritis.
Combining the relevant literature, let's understand that PPP syndrome ~ PPP syndrome is a rare disease.
The population is mainly middle-aged men, with a peak of 50-60 years old.
Most patients have a history of heavy drinking. PPP syndrome is related to pancreatic related diseases such as acute/chronic pancreatitis, pancreatic cancer (usually pancreatic carcinoma), neuroendocrine tumor, insulinoma, pancreatic division, pancreatic vascular fistula, traumatic pancreatitis, and pancreatic duct stenosis.
The pathogenesis is not clear.
It may be that excessive secretion of trypsin increases the permeability of the microcirculation, and lipase and amylase enter the fat lobules, leading to the dissolution of subcutaneous fat and intramedullary fat, and secondary inflammatory reactions.
About two-thirds of patients have no obvious abdominal symptoms, which can easily lead to misdiagnosis and missed diagnosis of pancreatic disease.
Panniculitis is more common in the lower extremities, with painful/painless reddish-brown nodules (0.
5cm-5cm), which can form aseptic abscesses, some of which may ulcer spontaneously, and exudate viscous, chylo-like aseptic fat necrosis.
Arthritis mainly affects the ankle, knee, metacarpophalangeal joints, etc.
It can be single joint, oligo-joint or multiple joints at the same time, with multiple joints being the most common.
In laboratory tests, most lipase and amylase are elevated, and some patients are normal, and the degree of pancreatin elevation does not match the severity of the disease.
In imaging examinations, pancreatic diseases can be detected by abdominal ultrasound and enhanced CT.
MRI can confirm intramedullary necrosis.
The typical manifestation is that the lesion is low-intensity shadow on T1WI and high-intensity shadow on T2WI lipid phase.
X-ray films show osteolytic damage to the cortex around the joints and worm-like changes.
Pathological manifestations (see Figure 8): focal fat necrosis, mainly fat lobule necrosis without vasculitis.
Fat cells form thick-walled "ghost" cells without nucleus.
There are varying degrees of fine spot-like basophilic calcium salt deposition and infiltration of neutrophils, lymphocytes, foam-like cells, and multinucleated giant cells in the edges of necrotic fat or in fat cells.
Figure 8 Pathological manifestations The treatment and prognosis of this disease depend on pancreatic disease, which requires active recognition and effective treatment.
Acute/chronic pancreatitis is mainly treated conservatively; pancreatic tumors are treated by chemotherapy or surgery; pancreatic pseudocysts are often removed by fluid drainage, surgery or endoscopy.
The use of hormones and non-steroidal anti-inflammatory drugs (NSAIDs) is controversial, and long-term large-scale use is not recommended; some panniculitis and osteoarthritis lesions of PPP syndrome respond poorly to hormones.
In this case, fasting, fluid rehydration, proton pump inhibitors, somatostatin analogs, methylprednisolone, and leflunomide were given treatment.
The patient's rash subsided significantly, and the swelling and pain of both knee joints were relieved compared with before.
Recheck the pancreas-related indicators (see Table 1).
Table 1 Changes in related indicators of the pancreas.
Conclusion: PPP syndrome is a rare disease with rapid progress and poor prognosis.
Patients often have no obvious abdominal symptoms, which can easily delay diagnosis and treatment.
When unexplained erythema nodosa/panniculitis and arthralgia occur, consider pancreatic panniculitis and PPP syndrome.
Sensitive examination methods are expected to improve the efficiency of diagnosis and treatment, but at present, histopathology is still the gold standard for diagnosis of this disease.
Treating pancreatic related problems is the key to treating this disease.