-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
*It is only for medical professionals to read for reference.
There is one more consideration when encountering hyperkalemia in clinical practice! The topic reappeared in a forum and saw a case sharing: in a certain year, a patient with a peripherally placed central venous catheter (PICC) was infused and the tube was sealed.
When the tube was half injected, the patient suddenly felt chest tightness, Out of breath, the nurse immediately stopped the bolus, but did not report to the doctor
.
About half an hour later, the patient hurriedly ran to the nurse's station and asked the head nurse if the nurse had used the wrong medicine, because it had never been so uncomfortable to inject the sealing liquid before
.
Listening to the patient's words, the head nurse felt a little stunned: Did the nurse seal the tube with potassium chloride as normal saline? The patient was immediately lifted to the bed and reported to the doctor in charge
.
The doctor in charge felt unbelievable at first, but after listening to the analysis of the head nurse, he immediately treated the symptoms as hyperkalemia
.
After treatment, the patient's symptoms were relieved and he was discharged from the hospital after a few days of observation
.
The final result verified the head nurse’s guess: the remaining tube-sealing solution was sent to the laboratory for testing, which confirmed that the tube-sealing solution contained a high concentration of potassium ions
.
It turns out that the nurse mistakenly used potassium chloride as normal saline when drawing the sealing solution, so 10 ml of the 20ml sealing solution was normal saline and 10ml was 10% potassium chloride
.
After reading the above cases, do you as a clinician find it a little weird? However, this case resonated with the nursing colleagues: the packaging of 10ml potassium chloride was exactly the same as normal saline.
Potassium chloride was used as normal saline to prepare the skin test solution, and 20ml potassium chloride was mistakenly used as the solvent diluent
.
Fortunately, some of the clinical errors were prevented in time, and some were discovered in time.
In the end, the patients were spared
.
But not every mistake is so lucky.
If the head nurse did not consider that the nurse might have taken potassium chloride by mistake, if the doctor on the shift did not see the potassium chloride ampoule, the consequences would be really unexpected
.
The purpose of sharing this case is to remind clinicians that one more consideration should be given to hyperkalemia in clinical practice
.
Rescue Collection Hyperkalemia is one of the common clinical emergencies.
Next, let's explore the classification, diagnosis and treatment plan of acute hyperkalemia
.
If you know what is happening, you must also know why, so you will be confident when you deal with it
.
1.
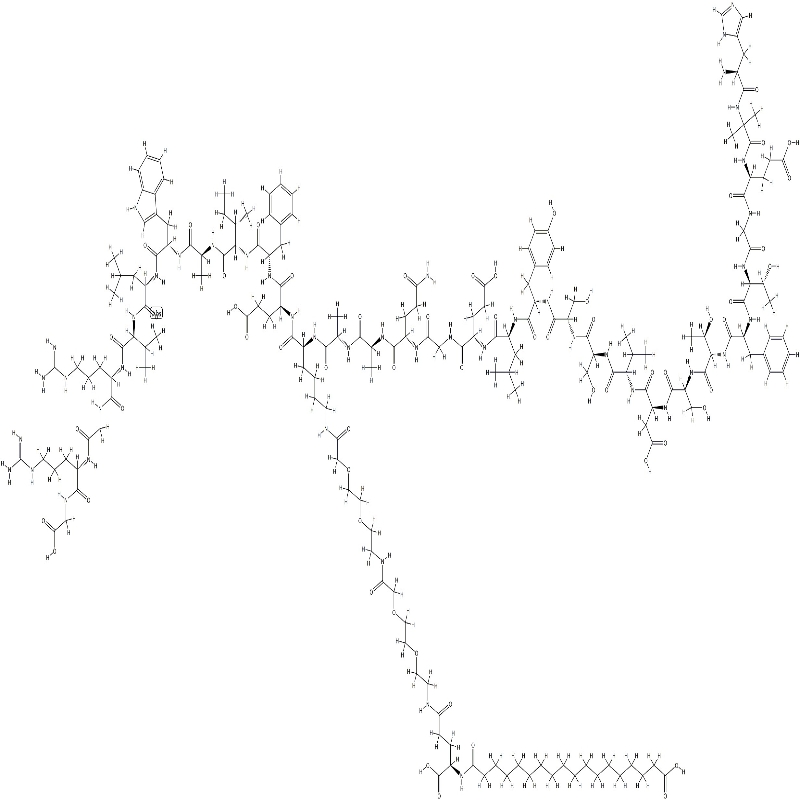
Classification of hyperkalemia Figure 1 2.
Diagnosis of acute hyperkalemia Figure 2 3.
Treatment of acute hyperkalemia 1.
Immediate use of intravenous calcium is the first-line treatment for hyperkalemia
.
Usage and dosage: 1.
Slowly inject 10% calcium chloride or calcium gluconate intravenously under ECG monitoring, which takes effect in 1 to 3 minutes and lasts for 30 to 60 minutes
.
If no effect is seen, the injection can be repeated
.
2.
Calcium should be used with caution in patients using digitalis preparations, because hypercalcemia may aggravate the toxic effect on the myocardium
.
In this case, 10 ml of 10% calcium gluconate can be added to 5% GS 100 ml for intravenous infusion for 20 to 30 minutes to allow sufficient time for calcium ions to be evenly distributed inside and outside the cell to prevent hypercalcemia
.
Mechanism of action: Calcium ions can quickly counter the effect of potassium ions on the action potential of the myocardium, stabilize the cell membrane potential, and restore the excitability of myocardial cells to normal
.
Note: Calcium gluconate is less irritating to veins, and peripheral intravenous injection can be used.
However, large doses of calcium chloride may cause tissue necrosis, so central intravenous drip is required
.
The second method is to promote potassium ions to enter cells and reduce blood potassium levels
.
1: It is recommended to use 10% glucose injection (GS) 500 ml+10 IU regular insulin intravenous drip for more than 1 h
.
Mechanism of action: Intravenous infusion of insulin and glucose can reduce the blood potassium concentration by promoting the transport of potassium ions into the cells
.
Generally, it takes effect 10-20 minutes after injection, the peak is 30-60 minutes, and it is maintained for 4-6 hours, which can reduce serum potassium by 0.
6-1.
0 mmol/L
.
Note: In case of patients with heart failure or oliguria, the infusion speed should be slow
.
If you want to limit the amount of water, you can increase the glucose solution concentration to 50%, and adjust the insulin dosage according to the blood sugar level
.
Closely monitor changes in blood potassium and blood sugar during the infusion process to avoid hypoglycemia
.
2: 150-250 ml of 5% sodium bicarbonate is injected intravenously, which takes effect within 5-10 minutes and lasts for about 2 hours
.
Mechanism of action: If the patient has metabolic acidosis, sodium bicarbonate can be injected intravenously to promote the entry of potassium ions into the cells through H+-Na+ exchange
.
Note: Sodium ions may aggravate the volume load of patients with chronic kidney disease (CKD), and should be used with caution in patients with heart failure
.
In the absence of metabolic acidosis, the clinical benefit and long-term prognosis of short-term use of sodium bicarbonate need to be further observed
.
3: For example, 10-20 mg salbutamol spray can reduce serum potassium concentration by 0.
5-1.
5 mmol/L within 30-60 minutes
.
Mechanism of action: β-adrenergic receptor stimulants can transfer potassium ions into cells, which usually take effect within 30 minutes and last for about 2 hours
.
Note: Because the combination of salbutamol and high-glycemic insulin is more effective, it is necessary to evaluate the patients for contraindications before use, and it is emphasized that it is not suitable as a single drug for patients with severe hyperkalemia
.
Reminder: The above method of lowering potassium only takes a few hours, and cannot discharge potassium ions, which is prone to rebound
.
The third method is to promote the excretion of potassium ions from the body and reduce the total potassium content in the body
.
①Diuretics: The combination of loop diuretics and thiazide diuretics is more effective, but for patients with hypovolemia, it may reduce the glomerular filtration rate, affect kidney function and aggravate hyperkalemia
.
It has limited effect on renal potassium excretion in patients with severe CKD, but it has a better effect on patients with hyporenin and hypoaldosteronemia
.
② Cation exchange resin: Polystyrene can be taken orally or as an enema, which can effectively bind potassium ions in the intestinal juice
.
Usage: Oral 15~30 g/time, 1~2 times/d, if not taken orally, enema can be given, the dosage is 30 g, 1~2 times/d
.
The sodium ions contained in polysulfonate are exchanged with blood potassium ions and then enter the body.
Patients with heart failure may cause aggravation of the condition, so attention should be paid when using it
.
Such drugs can easily cause constipation, and have the risk of intestinal obstruction and intestinal perforation
.
③A new type of potassium ion binder: It can capture potassium ions with high selectivity by replacing sodium/hydrogen ions in the whole intestine, reducing the absorption of potassium ions in the intestine, thereby quickly and effectively reducing the blood potassium concentration
.
④ Dialysis treatment: It is the first choice for treating severe hyperkalemia, especially for patients with end-stage renal failure (ESRD) with vascular access
.
Hemodialysis is better than peritoneal dialysis in reducing potassium.
In patients with unstable hemodynamics, continuous renal replacement therapy (CRRT) is used more
.
4 hours of hemodialysis can remove 40-120 mmol potassium ions on average
.
At the end of the article