-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
As we all know, diabetes is associated with chronic kidney disease (CKD), atherosclerotic cardiovascular disease (ASCVD), heart failure and higher mortality
.
However, the blood glucose imbalance before the patient develops type 2 diabetes is called prediabetes and is more common than diabetes
.
An epidemiological survey of nearly 100,000 adults in China organized by the Diabetes Branch of the Chinese Medical Association in 2010 estimated that the pre-diabetes prevalence rate was 50.
1%
.
Current treatment guidelines and research mainly focus on blood sugar control and prevention of its progression to type 2 diabetes, but there are few studies on human risks
.
Some people even question the effectiveness and practicality of pre-diabetes, believing that it is a sign of over-diagnosis
.
So is this really the case? In May of this year, the Journal of the American College of Cardiology published a British study that believed that pre-diabetes is an important risk factor for CKD and ASCVD and requires the attention of medical workers
.
Research Design This study is called the British Biobank and is a prospective and observational population cohort study.
The subjects were more than 500,000 British residents aged 40-69 years recruited between 2006 and 2010
.
At the time of registration, participants provided basic information (including life>
.
At the same time, participants underwent a physical examination before joining the group
.
The research team will follow up patients regularly until the end of March 2020
.
At baseline, the participants did not have type 1 diabetes, ASCVD, heart failure or CKD.
At the same time, the participants' glycosylated hemoglobin (HbA1c), high-density lipoprotein, cholesterol, high-sensitivity C-reactive protein, urine albumin, creatinine and other related information were collected.
.
The study mainly compared type 2 diabetes (definition: diagnosed as type 2 diabetes, HbA1c≥6.
5% at baseline, and/or use of insulin), prediabetes (undiagnosed type 2 diabetes, but HbA1c≥5.
7%, <6.
5%, consistent with American Diabetes Association definition) and normal blood sugar (undiagnosed type 2 diabetes, while HbA1c <5.
7%)
.
The main observation events are ①ASCVD, which is defined as a combination of coronary artery disease, ischemic stroke and peripheral artery disease; ②CKD; ③heart failure
.
The secondary observation events were ASCVD-related mortality and all-cause mortality
.
The results of the study were more than 500,000 participants, and a total of 336,709 cases had no ASCVD, CKD or heart failure at baseline, of which 277081 (82.
3%) had normal blood sugar, 46,911 (13.
9%) had prediabetes, and 12,717 (3.
8%) For patients with type 2 diabetes
.
Their average age was 56.
3 (8.
1) years old, and 186,572 cases (55.
4%) were women
.
In general, during the follow-up period, 21769 cases (7.
9%) with normal blood sugar, 6476 cases (13.
8%) with prediabetes, 3017 cases (23.
7%) with type 2 diabetes had 1 major observational event (ASCVD, CKD) And heart failure)
.
In terms of CKD, 5473 (2.
0%) participants with normal blood sugar, 1868 (4.
0%) participants with prediabetes, and 1181 (9.
3%) participants with diabetes were diagnosed with CKD during the follow-up period; ASCVD was the most important participant.
Common main observation events, 15856 (5.
7%) normal blood sugar participants, 4681 (10.
0%) prediabetes and 2138 (16.
8%) type 2 diabetes were diagnosed as ASCVD; for heart failure, 4207 cases (1.
5%) ) Participants with normal blood sugar, 1354 cases (2.
9%) with prediabetes, and 660 cases (5.
2%) with type 2 diabetes developed heart failure during the follow-up period
.
In addition, 6589 (14%) pre-diabetic participants progressed to type 2 diabetes during the follow-up period
.
In addition, after adjusting for age, gender, and race related factors, the pre-diabetes and normal blood glucose levels were compared with ASCVD (HR=1.
44, 95% CI, 1.
39-1.
49; P<0.
001), CKD (HR=1.
48,95).
% CI, 1.
40-1.
56, P<0.
001) is associated with an increased risk of heart failure (HR=1.
46, 95% CI, 1.
38-1.
56; P<0.
001)
.
After full covariate adjustment, prediabetes remained independent of ASCVD (HR=1.
11, 95% CI, 1.
08-1.
15; P<0.
001) and CKD (HR=1.
08, 95% CI, 1.
02-1.
14; P=0.
009) Related
.
Conclusion The research team believes that early intervention for patients with prediabetes will help reduce the risk of ASCVD and CKD
.
In addition to life>
.
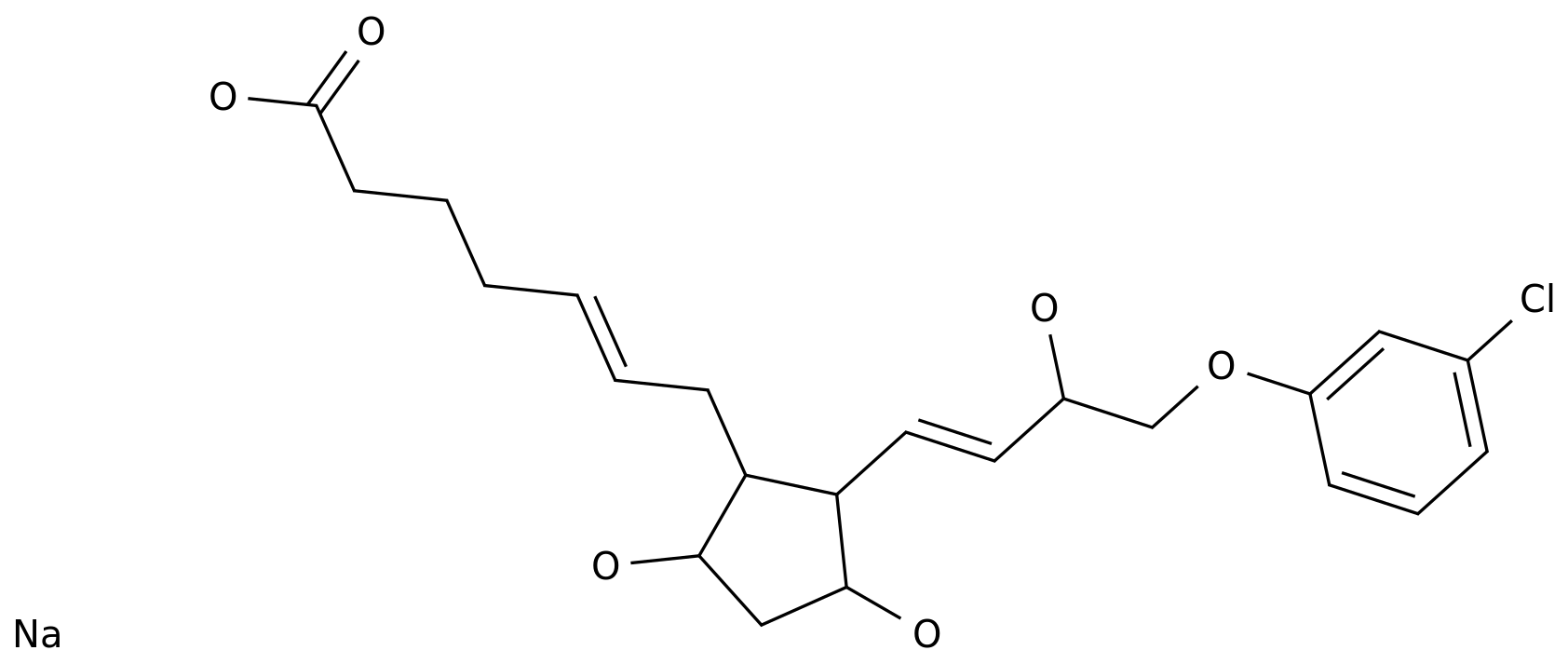
The research team recommends that patients with prediabetes should be the focus of future prevention trials, and the trial can use new hypoglycemic drugs such as sodium-glucose cotransporter 2 inhibitors to intervene in patients
.
Medical staff can consider "moving forward", intervene in pre-diabetes patients in time, monitor the patient's kidney and cardiovascular system in a targeted manner, and block CKD and ASCVD in advance! References: 1.
Honigberg MC, Zekavat SM, Pirruccello JP, et al.
Cardiovascular and Kidney Outcomes across the Glycemic Spectrum: Insights from the UK Biobank.
J Am Coll Cardiol.
2021 May 11:S0735-1097(21)05045-2.
2 .
Xu Y, Wang L, He J, et al.
Prevalence and control of diabetes in Chinese adults.
JAMA.
2013 Sep 4;310(9):948-59.