-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
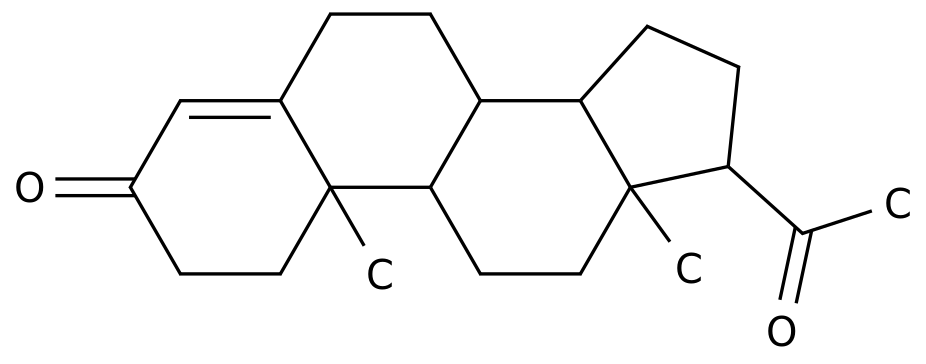
*For medical professionals to read and reference Weekly News Issue 246: Acarbose has a good effect on controlling postprandial blood sugar in Chinese, but now it is facing a crisis of failure? This week's summary Oral and intestinal microbes are not simple, and they actually make the commonly used hypoglycemic drugs in China ineffective! If women sleep less, they will have more body and visceral fat, while men will lose weight if they sleep more? In-hospital blood sugar measurement can catch diabetic patients, but everyone's measurement method is too confusing! 1 The oral and intestinal microbes are not simple, and they actually make the commonly used hypoglycemic drugs in China ineffective! Acarbose is an alpha-glucosidase inhibitor, which is commonly used in Chinese diabetic patients
.
Its main effect is to inhibit the absorption of carbohydrates, and acarbose can reduce postprandial blood sugar to a certain extent by swallowing it immediately before a meal or chewing it with the first bite.
However, recently published in the journal Nature The study found that oral and intestinal microbes can trigger a "crisis" of hypoglycemic failure! Figure 1.
1 Research published in the journal Nature This study led by Princeton University in the United States pointed out that more than 95% of acarbose remains unabsorbed in the gut, coupled with its ability to inhibit bacterial α-glucosidase, it is very important for the human body.
had a significant impact on the gut microbiome
.
The study used a metagenomic-biochemical-structural biology approach to detect acarbose-related enzymes produced by human microbes
.
These enzymes specifically metabolize and inactivate acarbose and may therefore affect the therapeutic effect of acarbose
.
Figure 1.
2 Acarbose is useless when phosphorylated by bacteria Acarbose originally came from bacteria in the soil
.
These bacteria grow their own ranks by secreting acarbose to inhibit the growth of other bacteria
.
At the same time, the bacteria that secrete acarbose do not want to be affected by acarbose themselves, so they secrete enzymes that inactivate acarbose
.
This enzyme can phosphorylate acarbose, thereby depriving acarbose of its ability to inhibit alpha-glucosidase
.
In this way, the bacteria will not be counteracted by the acarbose secreted by themselves
.
However, the bacteria's self-protection ability is not good news for humans
.
The researchers worry that not only the bacteria in the soil have the ability to inactivate acarbose, but similar bacteria may also exist in the human body
.
If acarbose is inactivated, it can no longer exert its hypoglycemic effect in the human body
.
So the research team examined the DNA sequence of the human microbiome and found that many bacteria seem to secrete an enzyme that inactivates acarbose, the AcbK clade microbiome-derived acarbose kinase (Mak)
.
These enzymes did indeed inactivate acarbose in in vitro tests
.
Many acarbose-inactivating enzyme Mak genes have been detected in human oral and intestinal microbes
.
The researchers further analyzed 16 patients with type 2 diabetes who were taking acarbose, eight of whom had the Mak gene and eight who did not
.
RESULTS: Compared with patients with the inactivated enzyme, acarbose was significantly higher on days 28 (p=0.
031), 56 (p=0.
046), and 84 (p=0.
003) of acarbose initiation.
HbA1c was better reduced in patients without the inactivating enzyme; on the 84th day of starting acarbose (p=0.
026), the effect of acarbose in reducing fasting blood glucose also began to differ between the two groups of patients.
Patients with inactivated enzymes did better with acarbose
.
Figure 1.
3 Decreased hypoglycemic efficacy with acarbose in Mak-positive patients In future studies, longitudinal metagenomic analyses of the gut and oral microbiomes may be required to examine the Detailed evaluation of clinical response, so as to clarify the influence of Mak gene on the treatment effect of diabetic patients and guide future medication
.
REF: Balaich J, Estrella M, Wu G, et al.
The human microbiome encodes resistance to the antidiabetic drug acarbose.
Nature.
2021 Dec;600(7887):110-115.
doi: 10.
1038/s41586-021-04091-0.
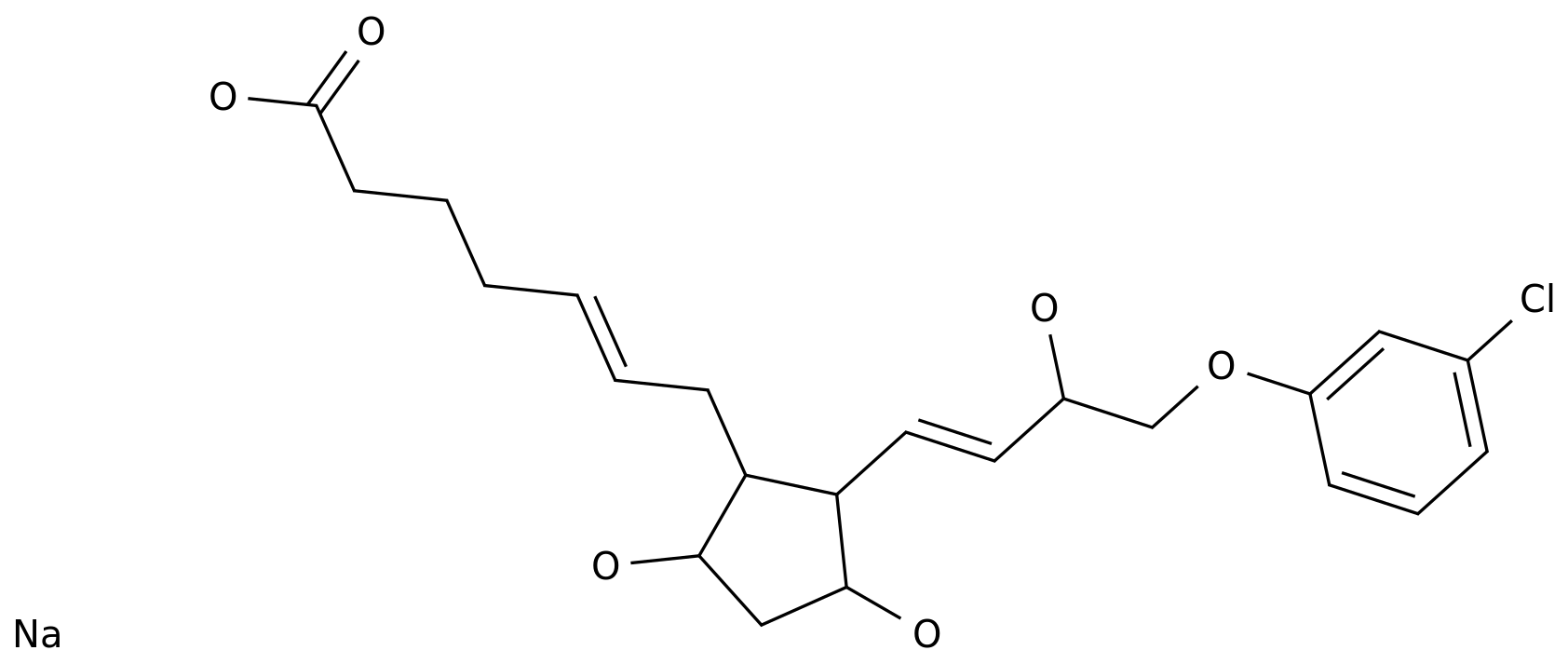
2 If women sleep less, they will have more body and visceral fat, while men will lose weight if they sleep more? The prevalence of obesity is rising, and sleep deprivation and poor sleep quality are becoming more common
.
Although there is a lot of evidence that lack of sleep is an important risk factor for obesity, there are also studies that suggest that there is no significant relationship between sleep duration and obesity, and men who sleep less may not necessarily be fat.
Not good, will it make you fat? To answer this question, a recent study published in the journal BMC Endocr Disord assessed the relationship between self-reported sleep duration and various indicators of obesity
.
Figure 2.
1 Study published in the journal BMC Endocr Disord This study from Nankai University School of Medicine used data from a chronic disease cohort study of natural populations living in communities in the Beijing-Tianjin-Hebei region
.
A total of 9069 participants were included in the study, of whom 63.
08% were female, and the age range of the participants was 19 to 91 years, with an average age of 45.
0 years
.
The study determined the duration of sleep based on the participants' self-reports.
The participants' height and weight were also measured, and a body mass index (BMI) was calculated; and the participants' body fat percentage (PBF) and internal organs were assessed by bioelectrical impedance analysis.
Fat Area (VFA)
.
According to the recommendations of the guidelines, general obesity is defined as BMI ≥ 28kg/m2; high PBF is defined as PBF>25% in males and PBF>35% in females; visceral obesity is defined as VFA≥100cm2
.
Figure 2.
2 The distribution of survey points in the chronic disease cohort study of natural population living communities in the Beijing-Tianjin-Hebei region found that compared with the participants with optimal sleep (sleep duration of 7-9 hours per day), the participants in short sleep (sleep duration <7 hours per day) The risk of systemic obesity (OR 1.
62, 95%CI 1.
24-2.
12) and visceral obesity (OR 1.
22, 95%CI 1.
02-1.
45) were both increased, but the risk of high PBF was not significantly increased (OR 1.
13, 95%CI 0.
95-1.
35)
.
Meanwhile, participants with long sleep (≥9 hours of sleep per day) had greater overall (OR 1.
06, 95%CI 0.
77-1.
45), visceral (OR 1.
10, 95%CI 0.
92-) adiposity compared with optimal sleep participants 1.
32) and high PBF (OR 1.
05, 95% CI 0.
88-1.
26) were also not significantly elevated
.
According to the analysis of gender, the relationship between sleep and obesity was also different between men and women
.
Among women, participants with short sleep had a 62% increased risk of overall obesity (OR 1.
62, 95%CI 1.
24-2.
12) and a 22% increased risk of visceral obesity (OR 1.
22, 95%CI 1.
02-1.
45)
.
However, among men, the risk of visceral obesity was reduced by 21% (OR 0.
79, 95% CI 0.
64-0.
99) in participants who slept longer
.
No relationship was found between sleep duration and higher risk of PBF in both sexes
.
The study showed that women who slept less were associated with an increased risk of obesity, while men who slept more were associated with a lower risk of visceral obesity
.
The researchers point out that there may be a mechanistic relationship between sleep duration and obesity
.
For example, sleep deprivation may increase appetite-stimulating hormone levels, while leptin levels decrease
.
At the same time, lack of sleep can also cause a series of problems such as sympathetic nervous system activation, impaired glucose metabolism, and increased inflammatory response, which may also lead to obesity
.
In addition, there are differences in the relationship between sleep duration and obesity between the sexes, and future research needs to further explore the reasons for this difference
.
REF: Fan Y, Zhang L, Wang Y, et al.
Gender differences in the association between sleep duration and body mass index, percentage of body fat and visceral fat area among chinese adults: a cross-sectional study.
BMC Endocr Disord.
2021 Dec 24;21(1):247.
doi: 10.
1186/s12902-021-00913-4.
3 Diabetic patients can be caught by measuring blood sugar in hospital, but everyone's measuring method is too confusing! Diagnosis of diabetes is generally not complicated, but a large number of people with diabetes remain undiagnosed
.
Therefore, taking every possible opportunity to screen people who may have diabetes can effectively reduce unnecessary medical burden
.
Blood glucose testing in hospitalized patients is routinely performed in the clinic, and a recent study published in the journal Diabet Med evaluated the effectiveness of “opportunistically” screening for diabetes while patients were hospitalized
.
Figure 3.
1 Research published in Diabet Med This systematic review from Exeter College and Clinical Medicine, University of Oxford, UK, included 12 studies of diabetes screening in hospitalized patients
.
These studies first performed random blood glucose testing in adult hospitalized patients, and then further performed glycated hemoglobin (HbA1c) testing in patients with abnormal random blood glucose testing in an attempt to identify true diabetic patients
.
A total of 25,987 hospitalized patients who underwent random blood glucose testing were included in the studies, of which 5,517 participants were considered too high blood sugar and were further tested for HbA1c levels
.
It turned out that everyone is very keen on testing the blood sugar of hospitalized patients, and many diabetic patients have been identified, but everyone's testing standards are really varied
.
The 12 included studies used 10 different random blood glucose thresholds, ranging from 5.
5 mmol/L to 11.
1 mmol/L for hyperglycemia, and there was no consensus on what hyperglycemia was
.
Consequently, the proportion of hyperglycemic patients detected in the studies varied widely, ranging from 3.
3% to 62.
1%
.
Those patients identified as hyperglycemic underwent further HbA1c testing
.
As can be imagined, the proportion of these so-called hyperglycemic patients who actually had diabetes also varied widely, ranging from 4.
1% to 90%
.
Notably, all relevant studies have identified patients with diabetes in hospitalized patients, suggesting that screening for diabetes during hospitalization does have some value
.
The researchers noted that in-hospital screening for hyperglycemia could provide a valuable opportunity for early diabetes diagnosis by identifying individuals at high risk
.
Inpatient blood glucose screening can facilitate the diagnosis of diabetes
.
At the same time, the proportion of hyperglycemic participants with currently undiagnosed diabetes varied widely, suggesting the need for further research and consistency in defining nosocomial hyperglycemia
.
This may help develop standardized screening protocols to identify patients who may have diabetes but have not yet been diagnosed
.
REF: Thornton-Swan TD, Armitage LC, Curtis AM, Farmer AJ.
Assessment of glycaemic status in adult hospital patients for the detection of undiagnosed diabetes mellitus: a systematic review.
Diabet Med.
2021 Dec 24:e14777.
doi: 10.
1111/dme .
14777.
.
Its main effect is to inhibit the absorption of carbohydrates, and acarbose can reduce postprandial blood sugar to a certain extent by swallowing it immediately before a meal or chewing it with the first bite.
However, recently published in the journal Nature The study found that oral and intestinal microbes can trigger a "crisis" of hypoglycemic failure! Figure 1.
1 Research published in the journal Nature This study led by Princeton University in the United States pointed out that more than 95% of acarbose remains unabsorbed in the gut, coupled with its ability to inhibit bacterial α-glucosidase, it is very important for the human body.
had a significant impact on the gut microbiome
.
The study used a metagenomic-biochemical-structural biology approach to detect acarbose-related enzymes produced by human microbes
.
These enzymes specifically metabolize and inactivate acarbose and may therefore affect the therapeutic effect of acarbose
.
Figure 1.
2 Acarbose is useless when phosphorylated by bacteria Acarbose originally came from bacteria in the soil
.
These bacteria grow their own ranks by secreting acarbose to inhibit the growth of other bacteria
.
At the same time, the bacteria that secrete acarbose do not want to be affected by acarbose themselves, so they secrete enzymes that inactivate acarbose
.
This enzyme can phosphorylate acarbose, thereby depriving acarbose of its ability to inhibit alpha-glucosidase
.
In this way, the bacteria will not be counteracted by the acarbose secreted by themselves
.
However, the bacteria's self-protection ability is not good news for humans
.
The researchers worry that not only the bacteria in the soil have the ability to inactivate acarbose, but similar bacteria may also exist in the human body
.
If acarbose is inactivated, it can no longer exert its hypoglycemic effect in the human body
.
So the research team examined the DNA sequence of the human microbiome and found that many bacteria seem to secrete an enzyme that inactivates acarbose, the AcbK clade microbiome-derived acarbose kinase (Mak)
.
These enzymes did indeed inactivate acarbose in in vitro tests
.
Many acarbose-inactivating enzyme Mak genes have been detected in human oral and intestinal microbes
.
The researchers further analyzed 16 patients with type 2 diabetes who were taking acarbose, eight of whom had the Mak gene and eight who did not
.
RESULTS: Compared with patients with the inactivated enzyme, acarbose was significantly higher on days 28 (p=0.
031), 56 (p=0.
046), and 84 (p=0.
003) of acarbose initiation.
HbA1c was better reduced in patients without the inactivating enzyme; on the 84th day of starting acarbose (p=0.
026), the effect of acarbose in reducing fasting blood glucose also began to differ between the two groups of patients.
Patients with inactivated enzymes did better with acarbose
.
Figure 1.
3 Decreased hypoglycemic efficacy with acarbose in Mak-positive patients In future studies, longitudinal metagenomic analyses of the gut and oral microbiomes may be required to examine the Detailed evaluation of clinical response, so as to clarify the influence of Mak gene on the treatment effect of diabetic patients and guide future medication
.
REF: Balaich J, Estrella M, Wu G, et al.
The human microbiome encodes resistance to the antidiabetic drug acarbose.
Nature.
2021 Dec;600(7887):110-115.
doi: 10.
1038/s41586-021-04091-0.
2 If women sleep less, they will have more body and visceral fat, while men will lose weight if they sleep more? The prevalence of obesity is rising, and sleep deprivation and poor sleep quality are becoming more common
.
Although there is a lot of evidence that lack of sleep is an important risk factor for obesity, there are also studies that suggest that there is no significant relationship between sleep duration and obesity, and men who sleep less may not necessarily be fat.
Not good, will it make you fat? To answer this question, a recent study published in the journal BMC Endocr Disord assessed the relationship between self-reported sleep duration and various indicators of obesity
.
Figure 2.
1 Study published in the journal BMC Endocr Disord This study from Nankai University School of Medicine used data from a chronic disease cohort study of natural populations living in communities in the Beijing-Tianjin-Hebei region
.
A total of 9069 participants were included in the study, of whom 63.
08% were female, and the age range of the participants was 19 to 91 years, with an average age of 45.
0 years
.
The study determined the duration of sleep based on the participants' self-reports.
The participants' height and weight were also measured, and a body mass index (BMI) was calculated; and the participants' body fat percentage (PBF) and internal organs were assessed by bioelectrical impedance analysis.
Fat Area (VFA)
.
According to the recommendations of the guidelines, general obesity is defined as BMI ≥ 28kg/m2; high PBF is defined as PBF>25% in males and PBF>35% in females; visceral obesity is defined as VFA≥100cm2
.
Figure 2.
2 The distribution of survey points in the chronic disease cohort study of natural population living communities in the Beijing-Tianjin-Hebei region found that compared with the participants with optimal sleep (sleep duration of 7-9 hours per day), the participants in short sleep (sleep duration <7 hours per day) The risk of systemic obesity (OR 1.
62, 95%CI 1.
24-2.
12) and visceral obesity (OR 1.
22, 95%CI 1.
02-1.
45) were both increased, but the risk of high PBF was not significantly increased (OR 1.
13, 95%CI 0.
95-1.
35)
.
Meanwhile, participants with long sleep (≥9 hours of sleep per day) had greater overall (OR 1.
06, 95%CI 0.
77-1.
45), visceral (OR 1.
10, 95%CI 0.
92-) adiposity compared with optimal sleep participants 1.
32) and high PBF (OR 1.
05, 95% CI 0.
88-1.
26) were also not significantly elevated
.
According to the analysis of gender, the relationship between sleep and obesity was also different between men and women
.
Among women, participants with short sleep had a 62% increased risk of overall obesity (OR 1.
62, 95%CI 1.
24-2.
12) and a 22% increased risk of visceral obesity (OR 1.
22, 95%CI 1.
02-1.
45)
.
However, among men, the risk of visceral obesity was reduced by 21% (OR 0.
79, 95% CI 0.
64-0.
99) in participants who slept longer
.
No relationship was found between sleep duration and higher risk of PBF in both sexes
.
The study showed that women who slept less were associated with an increased risk of obesity, while men who slept more were associated with a lower risk of visceral obesity
.
The researchers point out that there may be a mechanistic relationship between sleep duration and obesity
.
For example, sleep deprivation may increase appetite-stimulating hormone levels, while leptin levels decrease
.
At the same time, lack of sleep can also cause a series of problems such as sympathetic nervous system activation, impaired glucose metabolism, and increased inflammatory response, which may also lead to obesity
.
In addition, there are differences in the relationship between sleep duration and obesity between the sexes, and future research needs to further explore the reasons for this difference
.
REF: Fan Y, Zhang L, Wang Y, et al.
Gender differences in the association between sleep duration and body mass index, percentage of body fat and visceral fat area among chinese adults: a cross-sectional study.
BMC Endocr Disord.
2021 Dec 24;21(1):247.
doi: 10.
1186/s12902-021-00913-4.
3 Diabetic patients can be caught by measuring blood sugar in hospital, but everyone's measuring method is too confusing! Diagnosis of diabetes is generally not complicated, but a large number of people with diabetes remain undiagnosed
.
Therefore, taking every possible opportunity to screen people who may have diabetes can effectively reduce unnecessary medical burden
.
Blood glucose testing in hospitalized patients is routinely performed in the clinic, and a recent study published in the journal Diabet Med evaluated the effectiveness of “opportunistically” screening for diabetes while patients were hospitalized
.
Figure 3.
1 Research published in Diabet Med This systematic review from Exeter College and Clinical Medicine, University of Oxford, UK, included 12 studies of diabetes screening in hospitalized patients
.
These studies first performed random blood glucose testing in adult hospitalized patients, and then further performed glycated hemoglobin (HbA1c) testing in patients with abnormal random blood glucose testing in an attempt to identify true diabetic patients
.
A total of 25,987 hospitalized patients who underwent random blood glucose testing were included in the studies, of which 5,517 participants were considered too high blood sugar and were further tested for HbA1c levels
.
It turned out that everyone is very keen on testing the blood sugar of hospitalized patients, and many diabetic patients have been identified, but everyone's testing standards are really varied
.
The 12 included studies used 10 different random blood glucose thresholds, ranging from 5.
5 mmol/L to 11.
1 mmol/L for hyperglycemia, and there was no consensus on what hyperglycemia was
.
Consequently, the proportion of hyperglycemic patients detected in the studies varied widely, ranging from 3.
3% to 62.
1%
.
Those patients identified as hyperglycemic underwent further HbA1c testing
.
As can be imagined, the proportion of these so-called hyperglycemic patients who actually had diabetes also varied widely, ranging from 4.
1% to 90%
.
Notably, all relevant studies have identified patients with diabetes in hospitalized patients, suggesting that screening for diabetes during hospitalization does have some value
.
The researchers noted that in-hospital screening for hyperglycemia could provide a valuable opportunity for early diabetes diagnosis by identifying individuals at high risk
.
Inpatient blood glucose screening can facilitate the diagnosis of diabetes
.
At the same time, the proportion of hyperglycemic participants with currently undiagnosed diabetes varied widely, suggesting the need for further research and consistency in defining nosocomial hyperglycemia
.
This may help develop standardized screening protocols to identify patients who may have diabetes but have not yet been diagnosed
.
REF: Thornton-Swan TD, Armitage LC, Curtis AM, Farmer AJ.
Assessment of glycaemic status in adult hospital patients for the detection of undiagnosed diabetes mellitus: a systematic review.
Diabet Med.
2021 Dec 24:e14777.
doi: 10.
1111/dme .
14777.