-
Categories
-
Pharmaceutical Intermediates
-
Active Pharmaceutical Ingredients
-
Food Additives
- Industrial Coatings
- Agrochemicals
- Dyes and Pigments
- Surfactant
- Flavors and Fragrances
- Chemical Reagents
- Catalyst and Auxiliary
- Natural Products
- Inorganic Chemistry
-
Organic Chemistry
-
Biochemical Engineering
- Analytical Chemistry
- Cosmetic Ingredient
-
Pharmaceutical Intermediates
Promotion
ECHEMI Mall
Wholesale
Weekly Price
Exhibition
News
-
Trade Service
Author: Wu Qian , Department of Rheumatology and Immunology , Provincial Hospital Affiliated to Shandong First Medical University
immunitySummary
SummaryIdiopathic inflammatory myopathies (IIMs), also known as myositis, are a heterogeneous group of autoimmune diseases with distinct clinical manifestations, treatment responses, and prognosis
.
Muscle weakness is usually the typical clinical presentation, but other organs may also be affected, including the skin, joints, lungs, heart, and gastrointestinal tract
Idiopathic inflammatory myopathies (IIMs) are a heterogeneous group of autoimmune diseases, often characterized by chronic myositis, with variable clinical manifestations, treatment response, and prognosis
.
Myasthenia, low muscular endurance, and myalgia are common co-symptoms of IIM, but extramuscular manifestations such as rash, arthritis, interstitial lung disease (ILD), and cardiac involvement are also common, emphasizing the systemic inflammatory nature of IIM (Fig.
diagnosis
Figure 1 Performance of IIM
Figure 1 Performance of IIMNote: MDA5, melanoma differentiation-related gene 5; NXP2, nuclear matrix protein 2; SAE, small ubiquitin-like modification activating enzyme; SRP, signal recognition granule; TIF1, transcriptional mediator 1
A major advance in the field of myositis in recent years has been the discovery of myositis-specific autoantibodies, MSA (present in up to 60% of IIM patients), which aid in the diagnosis of IIM
.
MSA is closely associated with different clinical phenotypes and is therefore important for predicting organ performance and prognosis
Historically, IIM has been classified into dermatomyositis (DM, juvenile and adult onset), polymyositis (PM), inclusion body myositis (IBM), and amyopathic dermatophytes based on the clinical and histopathological manifestations of muscle tissue.
Myositis (ADM) subtype
.
With the deepening of its understanding, new IIM subtypes have been identified, namely anti-synthetase syndrome (ASyS), immune-mediated necrotizing myopathy (IMNM), cancer-associated myositis, and overlapping myositis
The current diagnosis of IIM and its subgroups is based on a combination of clinical symptoms and signs, including muscle biopsy features, MRI patterns, serological assessment, and serum muscle enzyme levels
.
Its treatment is mainly based on the combined use of high-dose glucocorticoids and other immunosuppressive drugs, but the response to treatment varies, so there is still a large clinical need for new treatments
clinical subtype
clinical subtypeDermatomyositis
DermatomyositisMost patients with dermatomyositis (DM) have MSA such as anti-Mi-2, anti-melanoma differentiation-associated gene 5 (MDA5), anti-transcriptional mediator 1 (TIF1), anti-nuclear matrix protein 2 (NXP2) or anti-small Ubiquitin-like modification activating enzyme (SAE) antibody
.
These autoantibodies are closely associated with different clinical phenotypes, therefore it is suggested to divide DM into six different subtypes - anti-Mi-2 DM, anti-MDA5 DM, anti-TIF1 DM, anti-NXP2 DM, anti-SAE DM and autoantibodies Negative DM (Figures 2 and 3)
Anti-Mi-2 DM has high creatine kinase levels, good response to treatment, and good prognosis, but frequently recurs; ILD is rare in anti-Mi-2 DM;
Patients with anti-MDA5 DM often have mild or no muscle disease
.
Anti-MDA5 DM is closely associated with ILD in most regions and ethnic groups
Anti-TIF1 DM is characterized by an extensive rash, relatively mild myositis, and dysphagia, which is associated with a high risk of malignancy
.
Patients with anti-NXP2 DM tend to have prominent muscle disease
.
In contrast, the skin presentation is relatively mild, and some patients may not have a rash
In patients with anti-SAE DM, skin manifestations often precede muscle manifestations, and the rash may become extensive
.
In addition, dysphagia is common, and some patients may have mild ILD
.
It has also been reported to be associated with malignant tumors
.
Figure 2 Clinical manifestations of anti-TIF1, anti-NXP2 and anti-Mi-2 DM patients
Figure 3 Clinical manifestations of anti-MDA5 and anti-SAE DM patients
anti-synthetase syndrome
anti-synthetase syndromeAnti-synthetase autoantibodies bind to and inhibit the function of aminoacyl-tRNA synthetases
.
To date, eight autoantibodies have been identified in ASyS patients, including anti-Jo1, anti-Ha/YRS, anti-Zo, anti-EJ, anti-PL-7, anti-OJ, anti-KS, and anti-PL-12 antibodies
.
ASyS is a relatively homogeneous but multisystem disease (Figure 4), with chronic, progressive ILD being the most common presentation
.
Compared with patients with anti-Jo1 autoantibodies, patients with ASyS and anti-PL-7 or anti-PL-12 autoantibodies had higher morbidity and mortality from ILD
.
Figure 4 Clinical manifestations of anti-synthetase syndrome
immune-mediated necrotizing myopathy
immune-mediated necrotizing myopathyIMNM is characterized by proximal muscle weakness with a symmetrical distribution, extremely high serum muscle enzyme levels, and a myopathic EMG pattern, with muscle specimens showing necrosis or regeneration with few lymphocytic infiltrates (Figure 5)
.
Few patients have overt systemic manifestations such as rash, arthritis, or ILD
.
IMNM contains 3 subtypes: anti-HMGCR, anti-SRP, and autoantibody-negative IMNM, where myopathy associated with malignancy or drug/toxin-induced myopathy needs to be excluded
.
Compared with patients with anti-HMGCR myopathy, patients with anti-SRP myopathy tend to have more severe muscle disease and extramuscular manifestations, including cardiac involvement and dysphagia
.
Patients with anti-HMGCR myopathy have predominantly skeletal muscle disease with variable and severe muscle weakness and no other organ manifestations
.
HMGCR is a pharmacological target of statins, and anti-HMGCR myopathy has been associated with statin use, but can also be found in statin-naïve individuals
.
Few descriptions of autoantibody-negative IMNM have been reported, but it has been reported to be characterized by frequent connective tissue disease, especially in patients with systemic sclerosis, with a much higher incidence of extramuscular manifestations than in patients with seropositive IMNM
.
Figure 5 Clinical manifestations of IMNM
Inclusion body myositis
Inclusion body myositisIBM is clinically characterized by chronic, progressive, asymmetric proximal and distal weakness of the muscles, including the quadriceps femoris and long finger flexors (Figure 6), and in severe cases, severe muscle wasting and even disability
.
IBM is more common in people over the age of 50, dysphagia occurs in more than 50% of patients, and other extramuscular manifestations are rare
.
Muscle histopathological features include endomysial T-cell infiltration and vacuoles surrounded by membranous cytoplasm
.
IBM may be associated with SS, other connective tissue disorders, and nodular disorders
.
IBM has made slow progress over the past few decades, often failing to respond to immunosuppressive therapy
.
Figure 6 Clinical manifestations of IBM
polymyositis
polymyositisPM is an acquired muscle disease characterized by the involvement of the proximal muscles of the extremities.
The most commonly affected muscles are the neck flexors and the proximal muscles of the extremities.
Distal muscle weakness is relatively rare
.
In severe cases, the bulbar muscles and respiratory muscles may be involved, resulting in swallowing, dysarthria, and dyspnea
.
PM rarely affects the facial muscles and usually does not involve the extraocular muscles
.
About 30% of patients have muscle pain
.
In addition to skeletal muscle involvement, PM can still have systemic symptoms such as fatigue, fever and weight loss, joint manifestations such as arthralgia and/or arthritis, pulmonary manifestations such as ILD and pleurisy, cardiac manifestations such as arrhythmia and myocarditis, and There are manifestations such as gastrointestinal Raynaud's phenomenon of peripheral vascular
involvement .
Extramuscular involvement is more common in MSAs-positive patients
.
PM usually does not improve on its own without treatment, but a small number of patients recur after treatment, and the overall prognosis is good
.
overlapping myositis
overlapping myositisMyositis can occur with diseases such as SLE, SS, systemic sclerosis, or rheumatoid arthritis
.
Overlap myositis is a heterogeneous subgroup due to variable clinical and histological manifestations
.
Autoantibodies detected in overlapping myositis include anti-U1RNP, anti-Ku, anti-PM-Scl, anti-RuvBL1, anti-RuvBL2, anti-Ro/SS-A and anti-La/SS-B antibodies
.
Patients with features of systemic sclerosis and myositis are called sclerosing myositis
.
Head ptosis and distal weakness are common manifestations, and the incidence of extramuscular manifestations is increased in patients without systemic sclerosis-related autoantibodies
.
pathology
pathologyHistopathological features of different subtypes of IIM
DM: perifascicular atrophy and perivascular inflammatory infiltration (Fig.
7a), CD4+ cell inflammatory infiltration (Fig.
7b), B cell inflammatory infiltration (Fig.
7c), MHC I expressed on myofibers, especially in the perifascicular distribution (Fig.
Fig.
7d) and capillary membrane attack complex deposition (Fig.
7e);
Anti-synthetase syndrome: perifascicular muscle fiber necrosis, perifascicular atrophy, and perimysial fragmentation (Fig.
7f);
IMNM: myofiber necrosis (Fig.
7g), high expression of MHC I on the sarcolemma of myofibers (Fig.
7h), and deposition of myofiber capillaries and episarcolemma attack complexes (Fig.
7i);
IBM: endomysial lymphocytes and macrophages aggregate and invade muscle fibers (Fig.
7j), CD8+ inflammatory infiltrates (Fig.
7k), marginal vacuoles (Fig.
7l);
PM: endomysium infiltrated and invaded non-necrotic muscle fibers (Fig.
7n), CD8+ cells infiltrated and invaded non-necrotic myofibers (Fig.
7o)
.
Figure 7 Typical histopathological changes of IIM subtypes
treat
treatManagement of IMM is challenging due to the diverse clinical presentation, variable duration of disease, and multiorgan and systemic features
.
There are currently no proven treatments recommended by guidelines or approved by the U.
S.
Food and Drug Administration ( FDA
) .
Fortunately, an increasing number of new treatments are currently undergoing Phase II or Phase III clinical trials using validated disease classification criteria and outcomes
.
The current goal of treatment with IMM is to improve patient symptoms and restore functional levels to near baseline without interfering with daily life
.
Glucocorticoids
GlucocorticoidsDespite the lack of proven controlled clinical trials, oral corticosteroids are the first-line or initial therapy for most patients with PM, DM, ASyS, or IMNM, especially those with severe myasthenia and ILD (Figure 8)
.
For patients with severe myositis or extramuscular manifestations (eg, ILD), pulsatile glucocorticoid therapy with intravenous methylprednisone can be given, but should be limited due to the high incidence of adverse effects and long-term complications of glucocorticoids its long-term use
.
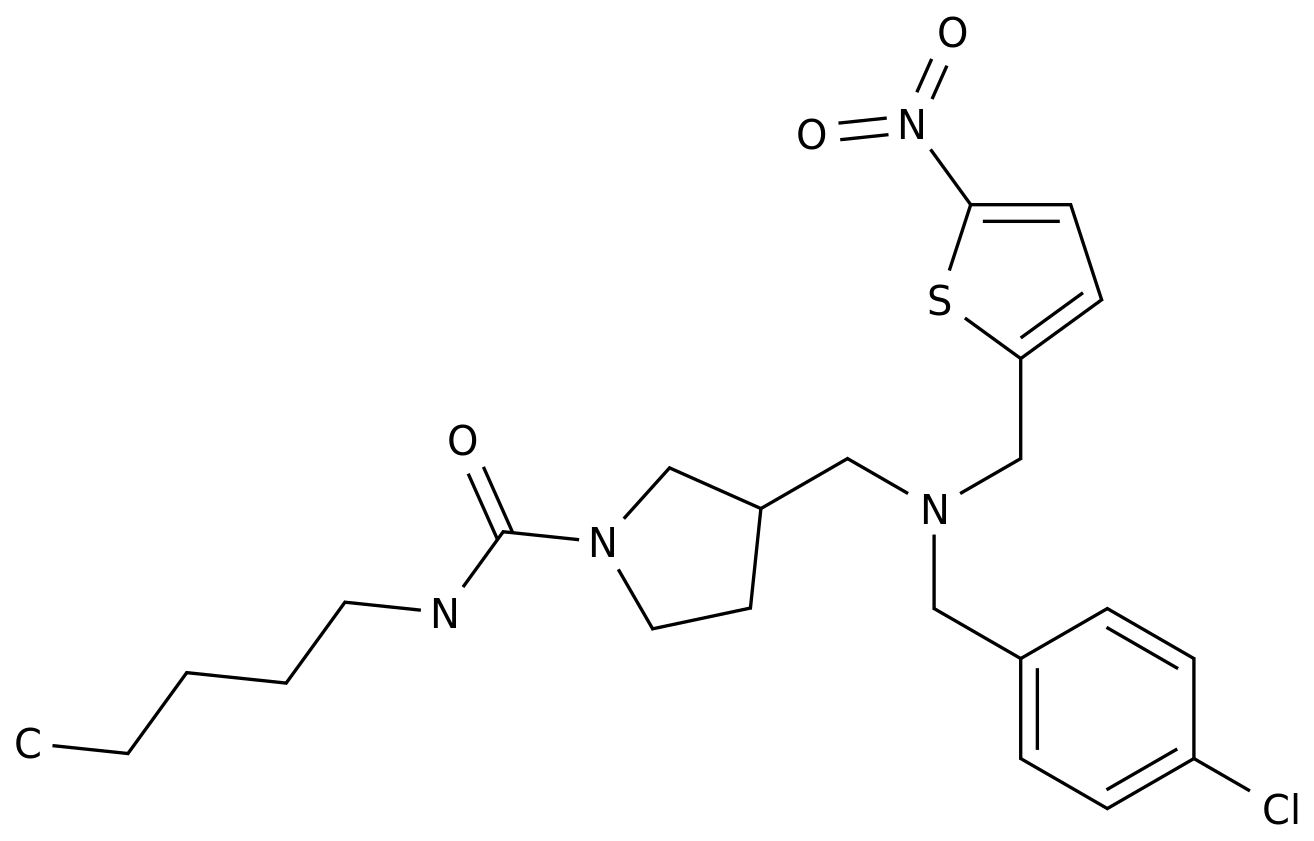
Figure 8 Common pharmacology and other therapies for IIM, except IBM
adrenocorticotropic hormone
adrenocorticotropic hormoneStored corticotropin injection (RCI) is a preparation containing corticotropin and other opioid-melanocortinopeptides that stimulate the melanocortin receptor
.
In a 24-week open-label trial of RCI in 10 patients with refractory PM or DM, 70% achieved the level of improvement defined by the International Myositis Assessment and Clinical Study Group (IMACS) (primary efficacy endpoint)
.
RCI is an FDA-approved drug for the treatment of PM and DM, but due to lack of data from randomized controlled trials and high cost, it is only used as a third-line or follow-up treatment
.
traditional immunosuppressants
traditional immunosuppressantsMost clinicians use methotrexate or azathioprine in combination with glucocorticoids as initial therapy in patients with myositis unless contraindicated (Figure 8)
.
Azathioprine is the drug of choice for patients with alcohol consumption, liver disease, or concomitant ILD, and is relatively safe during pregnancy
.
A growing number of retrospective and prospective studies support the efficacy of mycophenolate mofetil in myositis and related diseases such as ILD and refractory DM rash
.
Mycophenolate mofetil is usually a second-line treatment for myositis, but in patients with moderate-to-severe myositis associated with ILD, it can be used as a first-line drug
.
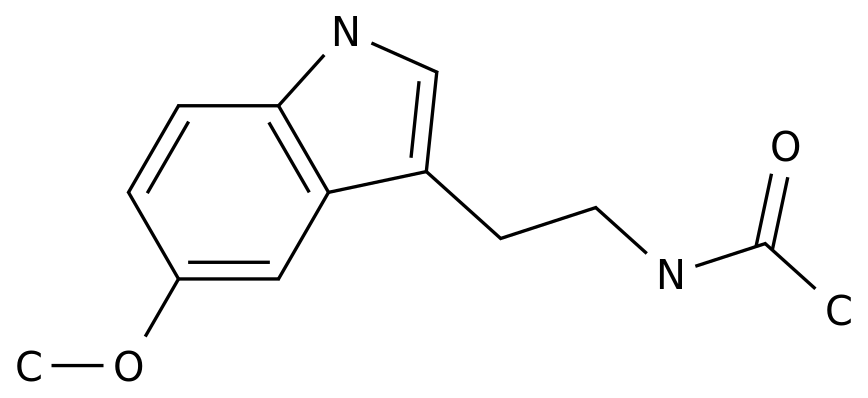
Cyclosporine and tacrolimus, calcineurin inhibitors that inhibit T-cell activation, can be used as second-line therapy in patients with refractory myositis with myasthenia or related ILD (Figure 9), but require Close monitoring of its toxic and side effects, such as regular blood levels
.
The use of cyclophosphamide is limited to severe refractory myasthenia, rapidly progressive ILD, or systemic vasculitis associated with PM or DM
.
Cyclophosphamide in combination with rituximab can be used in patients with positive anti-synthetase autoantibodies and severe ILD or in patients with positive anti-MDA5 autoantibodies, but it may be associated with a higher risk of infection
.
Figure 9 Treatment considerations for patients with refractory myositis based on clinical serology
Immunoglobulin
ImmunoglobulinIVIg is a drug with anti-inflammatory and immunomodulatory mechanisms without direct immunosuppressive effects
.
IVIg can be used in combination with glucocorticoids and/or other immunosuppressive agents as second- or third-line treatment of IIM or after failure of conventional therapy
.
In recent years, IVIg has been increasingly used as a first-line treatment for myositis, especially IMNM
.
A large, randomized, placebo-controlled phase III study demonstrated the efficacy and safety of IVIg in patients with refractory DM with muscle weakness and rash
.
IVIg has several advantages, such as its concomitant use with other immunosuppressive drugs or in the setting of pregnancy, infection or malignancy
.
Biologics
BiologicsRituximab depletes CD20+ B cells that may be involved in the pathogenesis of certain subpopulations of myositis
.
Several open-label studies have reported safety and efficacy in patients with severe and refractory myositis, including a subgroup of IMNM patients with anti-SRP autoantibodies, a marker of poor prognosis
.
The presence of anti-synthetase autoantibodies, anti-Mi2 autoantibodies, juvenile DM, and low disease activity at trial initiation were strong predictors of a beneficial response to rituximab
.
Rituximab is increasingly used in myositis-related ILD, especially ASyS, with positive results in retrospective and prospective studies
.
Although tumor necrosis factor (TNF) has been implicated in the pathogenesis of myositis, the efficacy of anti-TNF drugs such as etanercept and infliximab has been dismal
.
Currently, anti-TNF therapy is generally not recommended or considered in adults with myositis, although it may play a role in calcinosis in juvenile DM
.
Exercise and Physical Therapy
Exercise and Physical TherapyNew data support the safety and efficacy of exercise in adult IIM patients
.
Exercise improves muscle function and quality of life (QoL) in patients
.
Exercise programs that enhance strength and function have been shown to activate molecular pathways that regulate aerobic capacity, capillary growth, and muscle remodeling, while reducing muscle inflammation
.
Therefore, it is recommended that patients exercise as early as possible, especially as directed by a physical therapist, and in a sequential manner based on individual responses
.
Most patients tolerate exercise without adverse effects, so physical activity should be considered the standard of care for myositis in adults and juveniles
.
Article taken from:
Lundberg IE, Fujimoto M, Vencovsky J, et al.
Idiopathic inflammatory myopathies.
Nat Rev Dis Primers.
2021 Dec 2;7(1):86.
Source: Rheumatology and Immunology Editor: Snow is only for doctors to learn and communicate
Source: Rheumatology and Immunology Editor: Snow is only for doctors to learn and communicate .Leave a message here